Abstract
The present study evaluated the simplicity and accuracy of a new modified blood pressure-to-height ratio (MBPHR3) in identifying hypertension among Han children aged 7–12 years. In 2011, anthropometric measurements were collected as part of a cross-sectional population-based study of 1352 Han children aged 7–12 years. Receiver operating characteristic curve analyses were performed to assess the accuracy of the modified systolic blood pressure-to-height ratio (MSBPHR3) and the modified diastolic blood pressure-to-height ratio (MDBPHR3) as diagnostic tests for the detection of elevated SBP and DBP, respectively. The accuracies of MSBPHR3 and MDBPHR3 (as assessed by the area under the curve) in identifying elevated SBP and DBP were greater than 0.85 (0.974–0.995). When the MBPHR3 was used to identify hypertensive children, the sensitivity was 100% in boys and 100% in girls. The specificity was 93.8% in boys and 97.1% in girls. In conclusion, the MBPHR3 is a simple, accurate and non-age-dependent index for the screening of hypertension in Han children.
Similar content being viewed by others
Introduction
Childhood hypertension has become a widely investigated topic within the last decade due to its increasing prevalence.1 Obesity increases the occurrence of hypertension; steep body mass index (BMI) increases during childhood leading to adolescent increases in blood pressure.2 Childhood hypertension is often asymptomatic. However, hypertension in childhood and adolescence is not a benign disease and causes significant target organ damage, which is already present at diagnosis.3 Appropriate early-stage diagnosis of hypertension is important for the timely and appropriate intervention of hypertension in children and adolescents. The availability of robust nomograms is essential for the correct evaluation of blood pressure values in children.4 Identifying hypertension in children and adolescents is more complicated than in adults because it is based on a set of age-, gender- and height-specific references for systolic blood pressure (SBP) and diastolic blood pressure (DBP).5 The age-, gender- and height-specific standards for SBP and DBP are less easily used by parents, non-professionals and even pediatric clinicians.
In 2011, we evaluated, for the first time, the performance of the blood pressure-to-height ratio (BPHR) in identifying elevated blood pressure among Han adolescents.6 We found that the BPHR was an accurate index for the identification of elevated blood pressure in adolescents. Other studies have confirmed the high performance of the BPHR in identifying elevated blood pressure in children and adolescents.7, 8, 9, 10, 11 Inconsistent with its performance in adolescents,6 the BPHR was negatively correlated with age in children. Thus, we proposed age-dependent cutoff points for children.12
Recently, Mourato and co-workers13 found that the modified blood pressure-to-height ratio (MBPHR=BP/(height (cm)+7 × (13−age in years))) showed better sensitivity and specificity than the BPHR in screening for blood pressure abnormalities in Brazilian children aged 5–12 years. We tested the applicability of this index on a population of 1352 Han children aged 7–12 years. The MBPHR was positively correlated with age in children. In the formula, the coefficient of ‘(13−age in years)’ was 7. This leads to the question of whether we can eliminate the correlation between age and the MBPHR by changing the coefficient (i.e., 6, 5, 4, 3, 2 or 1).
In this study, we explored a new MBPHR to identify hypertension in Han children.
Methods
Subjects
We analyzed data on 1352 Han children (679 boys and 673 girls) aged 7–12 years from the 2011 children hypertension survey of Qinhuangdao. This study was approved by the ethics committee of the First Hospital of Qinhuangdao. All of the participants were required to be healthy. Both a detailed medical history and a complete physical examination were performed prior to the study. Children with a diagnosis of secondary hypertension, acute or chronic illnesses, infections, renal or hepatic diseases, or neoplasia or who were receiving medical treatment were excluded.
Measurements
Anthropometric measurements of height and weight were collected while the subjects were without shoes and in light clothing. Height and weight were measured to the nearest 0.1 cm and 0.1 kg, respectively. The standing height without shoes was measured three times with a stadiometer, and the three measurements were averaged for the analysis. Blood pressure was measured three times with a mercury sphygmomanometer while the subject was seated after 10 min of rest, and the three measurements were averaged for the analysis. The blood pressure cuff width was 40–50% of the arm circumference. SBP was determined at the onset of the 'tapping' Korotkoff sounds (K1), and DBP was determined at the fifth Korotkoff sound (K5). If a very low K5 persisted, then the blood pressure at K4 (muffling of the sounds) was recorded as the DBP. The following equations for the BPHR were used: systolic blood pressure-to-height ratio (SBPHR)=SBP (mm Hg)/height (cm) and diastolic blood pressure-to-height ratio (DBPHR)=DBP (mm Hg)/height (cm).
After the first screening, the cutoff points of the BPHR were determined according to the definition of hypertension approved by the 2004 National High Blood Pressure Education Program Working Group (gold standard).14 For all of the children in the hypertensive range (children with an SBP/DBP ⩾95th percentile and/or children with an SBPHR/DBPHR that exceeded the gold standard cutoff point), we repeated the measurements on two subsequent occasions. The (gold standard) definition of hypertension was a mean SBP and/or DBP ⩾95th percentile for all three screenings, and the (gold standard) definition of stage 2 hypertension was a mean SBP and/or DBP ⩾99th percentile+5 mm Hg for all three screenings.14
Research procedures
Step 1. Compare the modified blood pressure-to-height ratio with age
The formula for the modified blood pressure-to-height ratio (MBPHR) was MBPHRn=BP/(height (cm)+x × (13−age in years)), where x=1∼7.
For example: MBPHR7=BP/(height (cm)+7 × (13−age in years))
MBPHR6=BP/(height (cm)+6 × (13−age in years))
MBPHR5=BP/(height (cm)+5 × (13−age in years))
All of the analyses were performed using the SPSS 11.5 statistical software (SPSS 11.5 for Windows; SPSS, Inc., Chicago, IL, USA). The Pearson’s correlation coefficient was used to test the association between the MBPHRx and age. The new MBPHR, which is not correlated with age, is denoted as MBPHRx. P<0.05 was considered to be statistically significant.
Step 2. Compare the accuracy of the BPHR, MBPHR7 and MBPHRx in identifying elevated blood pressure in Han children
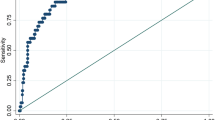
By using a receiver operating characteristic (ROC) analysis, the ROC curves of the SBPHR, MSBPHR7 and MSBPHRx were drawn to show how well they could separate subjects into groups with or without an elevated SBP (using both mean SBP ⩾95th percentile and mean SBP ⩾99th percentile+5 mm Hg as cutoffs) compared with the gold standard age-, gender- and height-specific references for SBP. Similarly, the ROC curves of the DBPHR, MDBPHR7 and MDBPHRx were drawn to show how well they could separate subjects into groups with and without an elevated DBP (using both the mean DBP ⩾95th percentile and the mean DBP ⩾99th percentile+5 mm Hg as cutoffs) compared with the gold standard age-, gender- and height-specific references for DBP. The ROC curves were plotted using measures of sensitivity and specificity based on various anthropometric cutoff values. ROC curves demonstrate the overall discriminatory power of a diagnostic test over the whole range of testing values. A better diagnostic test shows a curve skewed toward the upper left corner. The area under the curve (AUC) is a measure of the diagnostic power of a test. A perfect test will have an AUC of 1.0, and an AUC of 0.5 means that the test performs no better than chance. A test with an AUC ⩾0.85 is considered an accurate test.15 The sensitivity and specificity of the anthropometric measurements were calculated at all possible cutoff points to find the optimal cutoff value. The optimal cutoff value is the value that yields the maximum sensitivity and specificity from the ROC curve.
Step 3. Compare the sensitivity and specificity of the MBPHRx with those of other screening tools in identifying elevated blood pressure in Han children
Different screening tools have been proposed to simplify the diagnosis of high BP in children, such as the Somu formula, Mitchell table, Chiolero table and Kaelber table16, 17, 18, 19 (Supplementary Table S1). Sensitivities and specificities for each screening tool were calculated and compared with the MBPHRx. All of the analyses were performed with MedCalc 11.4.2.0 software (Ostend, Belgium).
Step 4. Determine the sensitivity and specificity of the MBPHRx in identifying hypertension in Han children
The hypertensive status of each child after three screenings was determined by the gold standard method and the MBPHRx (new standard). We then computed the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the MBPHRx to predict hypertension for subgroups of gender, BMI (stratified as normal, overweight or obese) and age group (7–9 and 10–12 years). The BMI groups were age- and gender-specific and based on normalized BMI cutoff reference values for Chinese children and adolescents.20 The likelihood ratios (positive (LR+) and negative (LR−)) were also computed in our study. The LR+ of a positive test result is calculated by dividing sensitivity by 1-specificity and indicates the increased odds of a disease when a test is positive. Conversely, the LR− is calculated by dividing 1-sensitivity by specificity and indicates the decreased odds of a disease when a test is negative.
Results
The prevalences of hypertension were 2.7% (stages 1 and 2) and 0.3% (stage 2). The mean and s.d. of height, age, SBP and DBP are presented in Table 1. Table 2 presents the Pearson correlation coefficients between age, MBPHR and BPHR for boys and girls. Age showed a strong positive correlation with the MSBPHR5-7 and MDBPHR5-7 in boys (P<0.05). Age showed a strong negative correlation with the MSBPHR1-2, SBPHR, MDBPHR1-2 and DBPHR in boys (P<0.05). Age showed a strong positive correlation with the MSBPHR4-7 and MDBPHR4-7 in girls (P<0.05). Age showed a strong negative correlation with the MSBPHR1, SBPHR, MDBPHR1 and DBPHR in girls (P<0.05). There was no relationship between age and MBPHR3 for both boys and girls (P>0.05).
The abilities of the MBPHR7, MBPHR3 and BPHR to accurately define elevated blood pressure were assessed by the AUC. Table 3 shows that, for both genders, the accuracy levels of the MBPHR7, MBPHR3 and BPHR in identifying elevated blood pressure (as assessed by AUC) were greater than 0.85 (AUC: 0.935–0.996). The AUC of MSBPHR3 was higher than the AUC of SBPHR for both boys and girls (for an elevated SBP defined as both the mean SBP ⩾95th percentile and the mean SBP ⩾99th percentile +5 mm Hg, P<0.05). The AUC of the MDBPHR3 was higher than the AUC of the DBPHR for both boys and girls (an elevated DBP was defined as a mean DBP ⩾95th percentile, P<0.05). The AUC of the MSBPHR3 was higher than the AUC of the MSBPHR7 for both boys and girls (an elevated SBP was defined as a mean SBP ⩾95th percentile, P<0.05). The AUC of the MDBPHR3 was higher than the AUC of the MDBPHR7 for boys (an elevated DBP was defined as a mean DBP ⩾95th percentile, P<0.05). The AUC of the MBPHR7 was higher than the AUC of the BPHR, but the difference was not significant (P>0.05).
The sensitivity of the MBPHR3 was higher than that of the BPHR (P<0.05) and was similar to that of the MBPHR7, Somu formulas, Mitchell table, Chiolero table and Kaelber table in boys (P>0.05). The specificity of the MBPHR3 was lower than that of the Somu formulas and Chiolero table (P<0.01) and was higher than that of the Mitchell table and Kaelber table in boys (P<0.01) (Table 4). The sensitivity of the MBPHR3 was higher than that of the BPHR and Chiolero table (P<0.05) and was similar to that of the MBPHR7, Somu formulas, Mitchell table and Kaelber table in girls (P>0.05). The specificity of the MBPHR3 was lower than that of the Somu formulas and Chiolero table (P<0.01) and was higher than that of the BPHR, MBPHR7, Mitchell table and Kaelber table in girls (P<0.05) (Table 5).
The optimal threshold of the MSBPHR3 for defining SBP ⩾95th percentile was 0.75 in boys and 0.77 in girls. The optimal threshold of the MSBPHR3 for defining SBP ⩾99th percentile+5 mm Hg was 0.84 in boys and 0.83 in girls. The optimal threshold of the MDBPHR3 for defining DBP ⩾95th percentile was 0.51 in boys and 0.50 in girls. The optimal threshold of the MDBPHR3 for defining DBP ⩾99th percentile+5 mm Hg was 0.56 in boys and 0.57 in girls. Two boys who had MSBPHR3 values that exceeded the cutoff points did not repeat their BP measurements on two subsequent occasions. These children were not defined as having hypertension by the gold standard. We assumed that these children were false positives of MSBPHR3. When the MBPHR3 (new standard) predicted hypertension, the sensitivity was 100% and the specificity was greater than 90%. The NPVs were much higher (100%), and the PPVs were lower (ranging from 28.1 to 60.0%) (Table 6). The MBPHR3 also had a better sensitivity and specificity when stratified by BMI into categories of normal, overweight or obesity (Supplementary Table S2) and by age into categories of 7–9 years and 10–12 years (Supplementary Table S3).
Discussion
The MBPHRx index had an adjustable feature for the identification of hypertension in children. As we changed the coefficient from 7 to 1, the relationship between age and the MBPHRx transitioned from a positive correlation to negative correlation. When the coefficient was 3, there was no relationship between age and the MBPHRx for both boys and girls. The levels of BP and height did not increase at the same rate during childhood.13 After adjusting for age, the MBPHR was independent of age. Thus, we were able to propose non-age-dependent cutoff points for the MBPHR3. The formula for the MBPHR3 is more complicated than for the BPHR. However, through the calculation, the number of cutoff points was reduced from 24 to 4, a number that is easy and feasible to manipulate for both professionals and lay people.
In this study, we found that the MBPHR3 was also an accurate indicator of hypertension in children. The areas under the ROC curve ranged from 0.974 to 0.995 and were consistent with robust diagnostic performance, indicating that the MSBPHR3 and the MDBPHR3 have powerful discriminative abilities to identify those with and those without elevated SBP and DBP. When hypertension was identified by the MSBPHR3/MDBPHR3, we found that both the sensitivities and specificities were greater than 90%. Compared with the age-dependent cutoff points of the BPHR (sensitivity: boys 100%, girls 95.0%; specificity: boys 94.3%, girls 96.8%),12 the non-age-dependent cutoff points of the MBPHR3 achieved the same results.
In a diagnostic testing, the PPV is the proportion of subjects with positive test results who are correctly diagnosed. The PPV is not intrinsic to the test, and it also depends on the prevalence. PPV is directly proportional to the prevalence of the disease or condition. Repeated measurements are required to confirm the diagnosis of hypertension in children. The prevalence of hypertension was only 2.7% at the third visit. If the study sample included a higher proportion of children with hypertension, then the PPV would probably increase.
However, given the low PPV, the MBPHR3 cannot completely replace blood pressure in this population. This means that some children without hypertension were misdiagnosed for hypertension according to the cutoff points of the MBPHR3. However, the NPVs were much higher (100%). This means that MBPHR3 did not miss any children with hypertension. After screening by the MBPHR3, only 57 boys (8.4% of boys) and 39 girls (5.8% of girls) needed further assessment to determine whether they were hypertensive. These results suggest that the MBPHR3 is a good screening method and can greatly reduce the work load of pediatric clinicians.
Several scholars produced simple tables and formulas to reduce the number of thresholds. The Somu formulas are simple equations that relate BP thresholds to age.19 The Mitchell table divides age into five-year categories and is independent of sex and height.18 The Chiolero table provides height-specific BP thresholds.16 The Kaelber table is age- and gender-specific but is independent of height.17 The MBPHR3 had a higher specificity than the Mitchell and Kaelber tables. The specificity of the MBPHR3 was lower than that of the Somu formulas and Chiolero table. However, the sensitivity of the MBPHR3 was higher than that of the Chiolero table in girls and higher than that of the Somu formulas in girls, although this comparison was not significant (P-value=0.0891). The MBPHR3 is an accurate and user-friendly screening tool. Compared with other screening tools, the MBPHR3 identifies hypertensive children with only four thresholds and, therefore, can be used in any setting.
The study has some limitations. First, it included children of Han ethnicity only, limiting the ability to generalize the study results to the other ethnic groups. Thus, this index should be validated in other ethnic groups. The performance of the BPHR to identify elevated blood pressure in children and adolescents was similar between different ethnic groups.7, 8, 9, 10, 11 Thus, we speculate that this new method could be applied to other ethnic groups. Second, children with stage 2 hypertension may need more prompt evaluation and pharmacologic therapy. The MBPHR3 was useful for identifying hypertension, especially stage 2 hypertension. However, due to the low prevalence, there were only four children with stage 2 hypertension in our study. A study with a larger sample size is needed to verify the accuracy of the MBPHR3 in identifying stage 2 hypertension.
In summary, the MBPHR3 is a simple, accurate and non-age-dependent index for the screening of hypertension in Han children. The method might be applicable to other ethnic groups, but should be validated in those groups.
References
Feber J, Ahmed M . Hypertension in children: new trends and challenges. Clin Sci (Lond) 2010; 119: 151–161.
Kuwahara E, Asakura K, Nishiwaki Y, Komatsu H, Nakazawa A, Ushiku H, Maejima F, Nishigaki Y, Hasegawa T, Okamura T, Takebayashi T . Steeper increases in body mass index during childhood correlate with blood pressure elevation in adolescence: a long-term follow-up study in a Japanese community. Hypertens Res 2014; 37: 179–184.
Antoniewicz J, Litwin M, Daszkoska J, Niemirska A, Sladowska J, Wierzbicka A, Wawer Z, Grenda R . Target organ damage in children with newly diagnosed and untreated essential hypertension. Przegl Lek 2006; 63: 101–106.
Cantinotti M, Giordano R, Scalese M, Molinaro S, Murzi B, Assanta N, Crocetti M, Marotta M, Ghione S, Iervasi G . Strengths and limitations of current pediatric blood pressure nomograms: a global overview with a special emphasis on regional differences in neonates and infants. Hypertens Res 2015; 38: 577–587.
Hansen ML, Gunn PW, Kaelber DC . Underdiagnosis of hypertension in children and adolescents. JAMA 2007; 298: 874–879.
Lu Q, Ma CM, Yin FZ, Liu BW, Lou DH, Liu XL . How to simplify the diagnostic criteria of hypertension in adolescents. J Hum Hypertens 2011; 25: 159–163.
Ejike CE . Blood pressure to height ratios as simple, sensitive and specific diagnostic tools for adolescent (pre)hypertension in Nigeria. Ital J Pediatr 2011; 37: 30.
Kelishadi R, Heshmat R, Ardalan G, Qorbani M, Taslimi M, Poursafa P, Keramatian K, Taheri M, Motlagh ME . First report on simplified diagnostic criteria for pre-hypertension and hypertension in a national sample of adolescents from the Middle East and North Africa: the CASPIAN-III study. J Pediatr (Rio J) 2014; 90: 85–91.
Outdili Z, Marti-Soler H, Simonetti GD, Bovet P, Paccaud F, Burnier M, Paradis G, Chiolero A . Performance of blood pressure-to-height ratio at a single screening visit for the identification of hypertension in children. J Hypertens 2014; 32: 1068–1074.
Rabbia F, Rabbone I, Totaro S, Testa E, Covella M, Berra E, Bertello MC, Gioia E, Cerutti F, Veglio F . Evaluation of blood pressure/height ratio as an index to simplify diagnostic criteria of hypertension in Caucasian adolescents. J Hum Hypertens 2011; 25: 623–624.
Xi B, Zhang M, Zhang T, Liang Y, Li S, Steffen LM . Hypertension screening using blood pressure to height ratio. Pediatrics 2014; 134: e106–e111.
Lu Q, Ma C, Yin F, Wang R, Lou D, Liu X . Blood pressure-to-height ratio as a screening measure for identifying children with hypertension. Eur J Pediatr 2013; 172: 99–105.
Mourato FA, Nadruz W Jr, Moser LR, de Lima Filho JL, Mattos SS . A modified blood pressure to height ratio improves accuracy for hypertension in childhood. Am J Hypertens 2015; 28: 409–413.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004; 114: 555–576.
Zou KH, O'Malley AJ, Mauri L . Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation 2007; 115: 654–657.
Chiolero A, Paradis G, Simonetti GD, Bovet P . Absolute height-specific thresholds to identify elevated blood pressure in children. J Hypertens 2013; 31: 1170–1174.
Kaelber DC, Pickett F . Simple table to identify children and adolescents needing further evaluation of blood pressure. Pediatrics 2009; 123: e972–e974.
Mitchell CK, Theriot JA, Sayat JG, Muchant DG, Franco SM . A simplified table improves the recognition of paediatric hypertension. J Paediatr Child Health 2011; 47: 22–26.
Somu S, Sundaram B, Kamalanathan AN . Early detection of hypertension in general practice. Arch Dis Child 2003; 88: 302.
Group of China Obesity Task Force. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Zhonghua Liu Xing Bing Xue Za Zhi 2004; 25: 97–102.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Ma, C., Lu, Q., Wang, R. et al. A new modified blood pressure-to-height ratio simplifies the screening of hypertension in Han Chinese children. Hypertens Res 39, 893–898 (2016). https://doi.org/10.1038/hr.2016.89
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.89
Keywords
This article is cited by
-
Home blood pressure monitoring in pediatric hypertension: the US perspective and a plan for action
Hypertension Research (2018)
-
Performance of modified blood pressure-to-height ratio for identifying hypertension in Chinese and American children
Journal of Human Hypertension (2018)
-
Epidemiology of hypertension and survey protocols: how to count counts
Hypertension Research (2017)
-
A new modified blood pressure-to-height ratio also simplifies the identification of high blood pressure in American children
Hypertension Research (2017)