Abstract
Obstructive sleep apnea (OSA) is a major modifiable risk factor of hypertension and hypertensive patients with OSA are at increased risk for cardiovascular diseases. A substantial number of studies have revealed that OSA and hypertension have synergistic effects on the cardiovascular system and, therefore, it is clinically important and relevant to increase our understanding of the pathophysiological interactions between OSA and hypertension. In our present review, after briefly reviewing the characteristics and pathophysiological effects of OSA, we focus on the current understanding of OSA-associated hypertension, the potential approaches for treatment of OSA and the effect of OSA treatment on hypertension management. We hope our present review will shed light for future studies that investigate effective therapeutic strategies to simultaneously improve the management of OSA and hypertension.
Similar content being viewed by others

Introduction
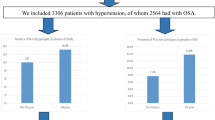
It is now well known that obstructive sleep apnea (OSA) is one of the common secondary causes of blood pressure (BP) elevation.1 Moreover, hypertensive patients with OSA are at increased risk of developing resistant hypertension2 and experiencing cardiovascular alterations and events3, 4, 5 compared with their hypertensive counterparts without OSA. Importantly, it has been reported that ~50% of OSA patients have hypertension6 and that ~30% of hypertensive patients are suffering from OSA.7 Therefore, it is essential to identify, diagnose and treat OSA, to effectively improve the control of hypertension and to reduce the incidence and prevalence of hypertension-associated cardiovascular events. In recent decades, population-based studies have demonstrated that OSA and hypertension impose great economic and health burdens on individual patients and society as a whole. Furthermore, there is accumulating evidence regarding the synergistic effects that OSA and hypertension exert on the cardiovascular system, owing to the large number of clinical and experimental studies. Therefore, we believe that it is clinically important to review the pathophysiological interactions between OSA and hypertension, to help us understand and manage these diseases effectively and efficiently.
In our present review, we focus on the following aspects. We first review the characteristics of OSA, then the general pathophysiological effects OSA has on cardiovascular systems and then illustrate the underlying mechanisms by which OSA contributes to the pathogenesis of arterial hypertension and other categories of OSA-associated hypertension. Finally, we present the potential approaches in managing OSA and the effects of OSA improvement in BP reduction.
Definition, diagnosis and risk factors of OSA
OSA occurs during nocturnal sleep and the diagnosis of OSA requires polysomnography to assess key variables such as arterial oxygen saturation, chest and abdomen respiratory movement, electroencephalogram findings and quantified air flow; all of these indices are subsequently used to determine the apnea–hypopnea index.8 In brief, the apnea–hypopnea index is the total number of episodes of apnea (complete blockade of airflow for >10 s) and hypopnea (>50% reduction in respiratory airflow accompanied by >3% reduction in arterial oxygen saturation for >10 s) per sleep hour; patients with OSA are classified into mild (5–15), moderate (15–30) and severe (>30) categories.8 In addition to the apnea–hypopnea index, typical clinical symptoms of OSA including daytime sleepiness and fatigue, frequent awakening during sleep, snoring, nocturia, reduced concentration and impaired memory are also important clues for clinical diagnosis.8 In recent decades, a substantial number of studies have identified multiple sensitive predictors that are useful to identify high-risk population. For example, patients with any anatomical abnormality of the upper airway (such as pharyngeal collapse due to macroglossia and adenotonsillar hypertrophy,9 or tongue displacement and pharynx narrowing due to retrognathia),10 which Asian and non-obese populations are predisposed to, can develop OSA. Second, epidemiological studies have shown that males are predisposed to OSA,11 and that the odds of developing OSA gradually increases with age and weight gain.12 Third, hereditary factors may also have a role in OSA development, as reported by Buxbaum et al.13 Last but not least, smoking, alcohol abuse, hormone depletion in postmenopausal women and nasal congestion due to allergic rhinitis are also considered to be significant risk factors for OSA.11 Owing to the high prevalence of OSA in the general population, it is crucial to prevent OSA development. We believe that designing a model to assess the risk of OSA in each individual would be helpful and future, large prospective studies are warranted to define the model’s variables and cutoff values. Thus, taking into account the common risk factors and the typical clinical manifestations of OSA (Figure 1) is important for the timely identification of the unrecognized OSA population and the proper use of polysomnography is helpful to accurately diagnose and evaluate the severity of OSA.
Pathophysiological effects of OSA on the cardiovascular system
OSA confers pathophysiological effects on the cardiovascular system through a variety of mechanisms (Figure 2). Fundamentally, periodic hypercapnia and hypoxemia due to apnea–hypopnea episodes causes sympathetic nerve activation and serum catecholamine elevation,14, 15 both of which subsequently increase heart rate and BP. In addition, the frequent arousals and sleep deprivation due to periodic asphyxia also result in sympathetic nerve activation16 and contribute to tachycardia and hypertension. Over time, these hemodynamic changes ultimately lead to left ventricular hypertrophy and heart failure.17 Second, it has been reported that hypoxemia promotes oxidative stress, systemic inflammation and endothelium dysfunction,18, 19 all of which can contribute to the development of atherosclerotic cardiovascular diseases. Third, to counteract the narrowing pharynx, negative intra-thoracic pressure is generated and it increases the mechanical stress on the ventricles and atria.20 Over time, cardiac remodeling, including left ventricle hypertrophy and left atrial enlargement, occurs and these maladaptive changes can manifest ultimately as overt cardiovascular diseases such as diastolic heart failure and atrial fibrillation.20, 21 Last but not least, other pathophysiological effects including impaired baroreflex sensitivity and the continuous activation of the renin–angiotensin–aldosterone axis also contribute to OSA-associated cardiovascular disorders.16 Collectively, the accumulated clinical data strongly support the notion that OSA has a central role in the pathogenesis of cardiovascular disease; it is clinically important to effectively control OSA, to reduce the adverse effects OSA imparts on the cardiovascular system.
Pathophysiological mechanisms of OSA on hypertension
The relationship between OSA and hypertension has been extensively investigated2, 22, 23, 24 and there is compelling evidence to indicate that there is a dose–effect relationship25, 26, 27 between the severity of in the OSA and degree of the BP elevation. The pathophysiological mechanisms by which OSA contributes to BP elevation are multi-factorial. On the one hand, hypoxemia induced by OSA causes systemic inflammation and oxidative stress, which result in increased endothelin-1 generation and decreased nitric oxide production in endothelial cells, increased arterial peripheral resistance and BP elevation.28, 29 On the other hand, the periodic hypoxemia, frequent arousals and sleep deprivation all cause sympathetic nerve activation that leads to increased cardiac output and peripheral vessel constriction, and thereby promotes BP elevation.30 It has been reported that patients with OSA have a higher prevalence of isolated diastolic hypertension31 and the underlying mechanism might be due to the tachycardia and shortening of cardiac diastole. Third, it has been reported that in comparison with subjects without OSA, subjects with OSA have significantly increased renin generation induced by efferent renal sympathetic nerve activation and this effect leads to elevations in plasma angiotensin-II and aldosterone. Together, these effects cause BP elevation by means of vasoconstriction and sodium–water retention, respectively. Furthermore, it has been reported that primary hyperaldosteronism is highly prevalent in subjects with OSA; therefore, it is important to screen for primary hyperaldosteronism in patients with OSA. Research has demonstrated that patients with both OSA and primary hyperaldosteronism are more likely to develop drug-resistant hypertension. Last but not least, it has been demonstrated that the sleep deprivation from OSA is associated with endothelial dysfunction and arterial stiffness,32 both of which initiate and accelerate the development of hypertension. The proposed mechanisms by which OSA causes hypertension are listed in Figure 3. Collectively, the pathophysiological effects of OSA on hypertension are multi-factorial and they are due to the high prevalence of OSA in hypertensive subjects. We believe that improving OSA should result in profound benefits in hypertension management.
Different categories of hypertension related to OSA
A substantial number of epidemiological studies have revealed that there are special categories of hypertension related to OSA; the most common and clinically relevant categories are resistant hypertension, nocturnal hypertension and masked hypertension.33, 34
OSA and resistant hypertension
Resistant hypertension, which is defined as BP that remains higher than 140/90 mm Hg despite treatment with three different classes of anti-hypertensive medicines (including diuretics) at their optimal doses, is a common secondary effect of OSA.35, 36 For example, Calhoun et al.37 observed that 90% of male patients and 77% of female patients with resistant hypertension had OSA. In another clinical study conducted by Ruttanaumpawan et al.,38 they reported that OSA was associated with an increased risk of resistant hypertension, with an adjusted odds ratio of 1.025 (95% confidence interval of 1.002–1.049). Furthermore, two cross-sectional studies revealed that there was dose–effect relationship between the severity of OSA and the magnitude of BP increase, as well as the number of anti-hypertensive medicines used to manage hypertension.39, 40 In recent times, a clinical study revealed that clinically significant OSA was independently associated with concentric hypertrophy in patients with resistant hypertension,41 which suggests that OSA might accelerate the adverse cardiovascular remodeling in subjects with resistant hypertension.
A substantial number of mechanisms contribute to OSA-related resistant hypertension. In addition to the aforementioned pathophysiological effects of OSA that can lead to BP elevation, primary hyperaldosteronism is also believed to be responsible for these phenomena.33 It has been reported that primary hyperaldosteronism is highly prevalent in patients with concomitant OSA and resistant hypertension, as evidenced by the finding that both the urine and plasma levels of aldosterone were significantly higher in this population.42, 43 On the one hand, sodium and water retention caused by hyperaldosteronism can lead to volume overload and BP elevation.43 On the other hand, parapharyngeal edema induced by fluid retention could exacerbate OSA and thereby promote further BP elevation.44, 45 Previous studies have suggested that this vicious cycle can be interrupted by treatment with aldosterone antagonists and continuous positive airway pressure (CPAP) therapy.46, 47 Nonetheless, randomized controlled clinical trials are still needed to provide solid evidence that these therapeutic modalities help improve BP control in subjects with resistant hypertension. Furthermore, it is also clinically important to examine the cardiovascular benefits of these therapies.
OSA and nocturnal hypertension
According to the circadian patterns of BP, high BP could be broadly classified into two categories: dipping and non-dipping. Briefly, a dipping pattern is when there is more than a 10% decrease in nighttime BP compared with daytime BP. By contrast, nocturnal hypertension is present when there is less than a 10% of reduction (non-dipping) in BP at night or when the nighttime BP is higher (riser) than during the day. A number of previous studies have revealed that nocturnal hypertension imposed greater adverse effects on the cardiovascular system than daytime hypertension.48, 49 It has been reported that the prevalence of nocturnal hypertension is substantially higher in subjects with OSA. For example, Loredo et al.50 reported that ~84% of patients with OSA in their study experienced nocturnal hypertension. Data from the Wisconsin Sleep Cohort Study indicated that there was a dose–effect relationship between the severity of OSA and the risk of nighttime BP elevation.51 The main mechanism contributing to nighttime BP elevation is the sympathetic overactivation caused by hypoxemia, frequent arousals and sleep deprivation. Treatment of OSA with CPAP therapy reversed the nighttime BP elevation.46 It is clinically important to screening for OSA in patients with non-dipping or difficult-to-treat hypertension.
OSA and masked hypertension
Masked hypertension is the term used to describe the condition when the BP measured in the office is within the target range but the BP assessed at home or by 24-h ambulatory BP monitoring is above the normal range. An epidemiological study conducted by Baguet et al.52 revealed that the incidence of masked hypertension in subjects with newly diagnosed OSA was nearly 30%. Another study revealed that among 61 male participants who were identified as normotensive by a clinic BP evaluation, one-third had masked hypertension and the patients with OSA had a higher incidence of masked hypertension than those without OSA.53 These data suggest a potential association between OSA and masked hypertension; however, large, prospective studies are needed to corroborate these findings and to help physician identify those patients who are at increased risk of incident masked hypertension. Moreover, experimental and clinical studies are needed to elucidate the mechanisms.
Approaches for managing OSA-associated hypertension
In addition to anti-hypertensive drugs, there are some other highly effective non-pharmacologic modalities for treating OSA-associated hypertension. For example, effective control of the co-morbidities that contribute to OSA and hypertension, such as obesity, smoking and alcohol abuse, is considered to be the most cost-effective strategy.54, 55 Surgical correction of the anatomical abnormalities of the upper airway is also a highly effective and efficient method. In addition, the use of oral appliances and CPAP therapy can also decrease BP in hypertensive patients with OSA. Clinical studies have revealed that oral appliance therapy was not only beneficial for OSA improvement but also for BP reduction.56, 57 In a recent randomized trial, Andrén et al.58 evaluated 72 patients with OSA and hypertension, who were randomized to receive either 3 months of wearing an oral appliance with mandibular advancement or control treatment. The efficacy of the oral appliance treatment was ascribed to the improvement in hypoxemia and its associated adverse effects, and these benefits have also been confirmed in clinical studies of CPAP treatment on OSA and OSA-associated hypertension. For example, in a randomized controlled trial, CPAP treatment significantly reduced systolic BP (SBP) in subjects with OSA. Drager et al.59 revealed that in pre-hypertensive or hypertensive patients with OSA, CPAP treatment substantially reduced the daytime systolic blood and the nighttime SBP and diastolic BP, when compared with the control group. In a recent published meta-analysis,60 CPAP therapy was significantly associated with 24-h ambulatory SBP and diastolic BP (DBP) reduction. Moreover, CPAP seemed more beneficial for decreasing nocturnal SBP than for diurnal SBP, and patients with resistant hypertension seemed to benefit most from CPAP therapy. In brief, the benefits derived from CPAP treatment may be associated with amelioration of hypoxemia and decreased nocturnal sympathetic nervous activation, and the resulting improvements in arterial oxygen saturation could mitigate the systemic inflammation and oxidative stress. Moreover, reduced negative intra-thoracic pressure caused by the positive pressure ventilation could also result in beneficial hemodynamic changes. All of these favorable effects of CPAP treatment simultaneously improve hypertension control. However, adherence is the most critical prerequisite to obtain the benefits of CPAP treatment. A recent clinical study revealed that a singular pre-CPAP treatment cluster of three plasma microRNAs predicted the BP response to CPAP treatment in patients with resistant hypertension and OSA;61 in the future, precision medicine using microRNA measurement could help target CPAP therapy in hypertensive subjects with OSA. For physicians considering which anti-hypertensive drugs to prescribe, there is no solid evidence to support the use of one specific drug class over another. There is no solid evidence of apnea–hypopnea index improvement with the commonly used anti-hypertensive medicines, including angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, calcium channel blocker, diuretic, β-blocker and α-receptor antagonist. Nonetheless, in patients with hyperaldosteronism, aldosterone antagonists should be the first choice agents. Moreover, diuretics may have a greater role in BP control by improving parapharyngeal edema. Overall, it is recommended that physicians treat patients with OSA-associated hypertension with a combination of various therapeutic modalities.
Conclusion
It is clinically important to screen for OSA in hypertensive patients, especially those patients who exhibit predominant diastolic BP elevation, difficult to control BP and nocturnal BP elevation. Increasing our understanding of the interplay of the mechanisms of OSA and hypertension is critical for the effective management of OSA-associated hypertension. More studies, especially in precision medicine, are warranted to investigate effective therapeutic strategies to improve the management of OSA and hypertension.
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ . Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–1252.
Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, Amodeo C, Bortolotto LA, Krieger EM, Bradley TD, Lorenzi-Filho G . Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension 2011; 58: 811–817.
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Nieto FJ, O'Connor GT, Boland LL, Schwartz JE, Samet JM . Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 2001; 163: 19–25.
Munoz R, Duran-Cantolla J, Martinez-Vila E, Gallego J, Rubio R, Aizpuru F, De La Torre G . Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke 2006; 37: 2317–2321.
Prejbisz A, Florczak E, Pregowska-Chwala B, Klisiewicz A, Kusmierczyk-Droszcz B, Zielinski T, Makowiecka-Ciesla M, Kolodziejczyk-Kruk S, Sliwinski P, Januszewicz A . Relationship between obstructive sleep apnea and markers of cardiovascular alterations in never-treated hypertensive patients. Hypertens Res 2014; 37: 573–579.
Silverberg DS, Oksenberg A, Iaina A . Sleep-related breathing disorders as a major cause of essential hypertension: fact or fiction. Curr Opin Nephrol Hypertens 1998; 7: 353–357.
Fletcher EC, DeBehnke RD, Lovoi MS, Gorin AB . Undiagnosed sleep apnea in patients with essential hypertension. Ann Intern Med 1985; 103: 190–195.
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 1999; 22: 667–689.
Ryan CM, Bradley TD . Pathogenesis of obstructive sleep apnea. J Appl Physiol (1985) 2005; 99: 2440–2450.
Li KK, Kushida C, Powell NB, Riley RW, Guilleminault C . Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope 2000; 110: 1689–1693.
Young T, Skatrud J, Peppard PE . Risk factors for obstructive sleep apnea in adults. JAMA 2004; 291: 2013–2016.
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J . Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000; 284: 3015–3021.
Buxbaum SG, Elston RC, Tishler PV, Redline S . Genetics of the apnea hypopnea index in Caucasians and African Americans: I. Segregation analysis. Genet Epidemiol 2002; 22: 243–253.
Parati G, Lombardi C, Hedner J, Bonsignore MR, Grote L, Tkacova R, Levy P, Riha R, Bassetti C, Narkiewicz K, Mancia G, McNicholas WT . Position paper on the management of patients with obstructive sleep apnea and hypertension: joint recommendations by the European Society of Hypertension, by the European Respiratory Society and by the members of European COST (COoperation in Scientific and Technological research) ACTION B26 on obstructive sleep apnea. J Hypertens 2012; 30: 633–646.
Somers VK, Dyken ME, Clary MP, Abboud FM . Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest 1995; 96: 1897–1904.
Konecny T, Kara T, Somers VK . Obstructive sleep apnea and hypertension: an update. Hypertension 2014; 63: 203–209.
Niroumand M, Kuperstein R, Sasson Z, Hanly PJ . Impact of obstructive sleep apnea on left ventricular mass and diastolic function. Am J Respir Crit Care Med 2001; 163: 1632–1636.
Kato M, Roberts-Thomson P, Phillips BG, Haynes WG, Winnicki M, Accurso V, Somers VK . Impairment of endothelium-dependent vasodilation of resistance vessels in patients with obstructive sleep apnea. Circulation 2000; 102: 2607–2610.
McNicholas WT . Obstructive sleep apnea and inflammation. Prog Cardiovasc Dis 2009; 51: 392–399.
Tkacova R, Rankin F, Fitzgerald FS, Floras JS, Bradley TD . Effects of continuous positive airway pressure on obstructive sleep apnea and left ventricular afterload in patients with heart failure. Circulation 1998; 98: 2269–2275.
Stoohs R, Guilleminault C . Cardiovascular changes associated with obstructive sleep apnea syndrome. J Appl Physiol (1985) 1992; 72: 583–589.
Worsnop CJ, Naughton MT, Barter CE, Morgan TO, Anderson AI, Pierce RJ . The prevalence of obstructive sleep apnea in hypertensives. Am J Respir Crit Care Med 1998; 157: 111–115.
Lavie P, Herer P, Hoffstein V . Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ 2000; 320: 479–482.
Bixler EO, Vgontzas AN, Lin HM, Ten HT, Leiby BE, Vela-Bueno A, Kales A . Association of hypertension and sleep-disordered breathing. Arch Intern Med 2000; 160: 2289–2295.
Duran J, Esnaola S, Rubio R, Iztueta A . Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med 2001; 163: 685–689.
Young T, Peppard P, Palta M, Hla KM, Finn L, Morgan B, Skatrud J . Population-based study of sleep-disordered breathing as a risk factor for hypertension. Arch Intern Med 1997; 157: 1746–1752.
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D'Agostino RB, Newman AB, Lebowitz MD, Pickering TG . Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 2000; 283: 1829–1836.
Garvey JF, Taylor CT, McNicholas WT . Cardiovascular disease in obstructive sleep apnoea syndrome: the role of intermittent hypoxia and inflammation. Eur Respir J 2009; 33: 1195–1205.
Atkeson A, Yeh SY, Malhotra A, Jelic S . Endothelial function in obstructive sleep apnea. Prog Cardiovasc Dis 2009; 51: 351–362.
Charkoudian N, Rabbitts JA . Sympathetic neural mechanisms in human cardiovascular health and disease. Mayo Clin Proc 2009; 84: 822–830.
Baguet JP, Hammer L, Levy P, Pierre H, Rossini E, Mouret S, Ormezzano O, Mallion JM, Pepin JL . Night-time and diastolic hypertension are common and underestimated conditions in newly diagnosed apnoeic patients. J Hypertens 2005; 23: 521–527.
Sunbul M, Kanar BG, Durmus E, Kivrak T, Sari I . Acute sleep deprivation is associated with increased arterial stiffness in healthy young adults. Sleep Breath 2014; 18: 215–220.
Pratt-Ubunama MN, Nishizaka MK, Boedefeld RL, Cofield SS, Harding SM, Calhoun DA . Plasma aldosterone is related to severity of obstructive sleep apnea in subjects with resistant hypertension. Chest 2007; 131: 453–459.
Shirasaki O, Yamashita S, Kawara S, Tagami K, Ishikawa J, Shimada K, Kario K . A new technique for detecting sleep apnea-related ‘midnight’ surge of blood pressure. Hypertens Res 2006; 29: 695–702.
Pimenta E, Calhoun DA . Resistant hypertension: incidence, prevalence, and prognosis. Circulation 2012; 125: 1594–1596.
Parati G, Ochoa JE, Bilo G, Mattaliano P, Salvi P, Kario K, Lombardi C . Obstructive sleep apnea syndrome as a cause of resistant hypertension. Hypertens Res 2014; 37: 601–613.
Calhoun DA, Nishizaka MK, Zaman MA, Harding SM . Aldosterone excretion among subjects with resistant hypertension and symptoms of sleep apnea. Chest 2004; 125: 112–117.
Ruttanaumpawan P, Nopmaneejumruslers C, Logan AG, Lazarescu A, Qian I, Bradley TD . Association between refractory hypertension and obstructive sleep apnea. J Hypertens 2009; 27: 1439–1445.
Lavie P, Hoffstein V . Sleep apnea syndrome: a possible contributing factor to resistant. Sleep 2001; 24: 721–725.
Grote L, Hedner J, Peter JH . Sleep-related breathing disorder is an independent risk factor for uncontrolled hypertension. J Hypertens 2000; 18: 679–685.
Dobrowolski P, Prejbisz A, Klisiewicz A, Florczak E, Rybicka J, Januszewicz A, Hoffman P . Determinants of concentric left ventricular hypertrophy in patients with resistant hypertension: RESIST-POL study. Hypertens Res 2015; 38: 545–550.
Gonzaga CC, Gaddam KK, Ahmed MI, Pimenta E, Thomas SJ, Harding SM, Oparil S, Cofield SS, Calhoun DA . Severity of obstructive sleep apnea is related to aldosterone status in subjects with resistant hypertension. J Clin Sleep Med 2010; 6: 363–368.
Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, Pimenta E, Aban I, Oparil S, Calhoun DA . Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med 2008; 168: 1159–1164.
Friedman O, Bradley TD, Logan AG . Influence of lower body positive pressure on upper airway cross-sectional area in drug-resistant hypertension. Hypertension 2013; 61: 240–245.
Friedman O, Bradley TD, Chan CT, Parkes R, Logan AG . Relationship between overnight rostral fluid shift and obstructive sleep apnea in drug-resistant hypertension. Hypertension 2010; 56: 1077–1082.
Martinez-Garcia MA, Capote F, Campos-Rodriguez F, Lloberes P, de Atauri MJD, Somoza M, Masa JF, Gonzalez M, Sacristan L, Barbe F, Duran-Cantolla J, Aizpuru F, Manas E, Barreiro B, Mosteiro M, Cebrian JJ, de la Pena M, Garcia-Rio F, Maimo A, Zapater J, Hernandez C, Grau SN, Montserrat JM . Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. JAMA 2013; 310: 2407–2415.
Gaddam K, Pimenta E, Thomas SJ, Cofield SS, Oparil S, Harding SM, Calhoun DA . Spironolactone reduces severity of obstructive sleep apnoea in patients with resistant hypertension: a preliminary report. J Hum Hypertens 2010; 24: 532–537.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K, Richart T, Ohkubo T, Kuznetsova T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Wang J, Sandoya E, O'Brien E, Staessen JA . Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet 2007; 370: 1219–1229.
Hoshide S, Kario K, Hoshide Y, Umeda Y, Hashimoto T, Kunii O, Ojima T, Shimada K . Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am J Hypertens 2003; 16: 434–438.
Loredo JS, Ancoli-Israel S, Dimsdale JE . Sleep quality and blood pressure dipping in obstructive sleep apnea. Am J Hypertens 2001; 14: 887–892.
Hla KM, Young T, Finn L, Peppard PE, Szklo-Coxe M, Stubbs M . Longitudinal association of sleep-disordered breathing and nondipping of nocturnal blood pressure in the Wisconsin Sleep Cohort Study. Sleep 2008; 31: 795–800.
Baguet JP, Levy P, Barone-Rochette G, Tamisier R, Pierre H, Peeters M, Mallion JM, Pepin JL . Masked hypertension in obstructive sleep apnea syndrome. J Hypertens 2008; 26: 885–892.
Drager LF, Diegues-Silva L, Diniz PM, Bortolotto LA, Pedrosa RP, Couto RB, Marcondes B, Giorgi DM, Lorenzi-Filho G, Krieger EM . Obstructive sleep apnea, masked hypertension, and arterial stiffness in men. Am J Hypertens 2010; 23: 249–254.
Rubinstein I, Colapinto N, Rotstein LE, Brown IG, Hoffstein V . Improvement in upper airway function after weight loss in patients with obstructive sleep apnea. Am Rev Respir Dis 1988; 138: 1192–1195.
Teschler H, Berthon-Jones M, Wessendorf T, Meyer HJ, Konietzko N . Influence of moderate alcohol consumption on obstructive sleep apnoea with and without AutoSet nasal CPAP therapy. Eur Respir J 1996; 9: 2371–2377.
Mehta A, Qian J, Petocz P, Darendeliler MA, Cistulli PA . A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med 2001; 163: 1457–1461.
Iftikhar IH, Hays ER, Iverson MA, Magalang UJ, Maas AK . Effect of oral appliances on blood pressure in obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med 2013; 9: 165–174.
Andren A, Hedberg P, Walker-Engstrom ML, Wahlen P, Tegelberg A . Effects of treatment with oral appliance on 24-h blood pressure in patients with obstructive sleep apnea and hypertension: a randomized clinical trial. Sleep Breath 2013; 17: 705–712.
Drager LF, Pedrosa RP, Diniz PM, Diegues-Silva L, Marcondes B, Couto RB, Giorgi DM, Krieger EM, Lorenzi-Filho G . The effects of continuous positive airway pressure on prehypertension and masked hypertension in men with severe obstructive sleep apnea. Hypertension 2011; 57: 549–555.
Hu X, Fan J, Chen S, Yin Y, Zrenner B . The role of continuous positive airway pressure in blood pressure control for patients with obstructive sleep apnea and hypertension: a meta-analysis of randomized controlled trials. J Clin Hypertens (Greenwich) 2015; 17: 215–222.
Sanchez-de-la-Torre M, Khalyfa A, Sanchez-de-la-Torre A, Martinez-Alonso M, Martinez-Garcia MA, Barcelo A, Lloberes P, Campos-Rodriguez F, Capote F, Diaz-de-Atauri MJ, Somoza M, Gonzalez M, Masa JF, Gozal D, Barbe F . Precision medicine in patients with resistant hypertension and obstructive sleep apnea: blood pressure response to continuous positive airway pressure treatment. J Am Coll Cardiol 2015; 66: 1023–1032.
Acknowledgements
This work was supported by grants from NSFC (81470571).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Cai, A., Wang, L. & Zhou, Y. Hypertension and obstructive sleep apnea. Hypertens Res 39, 391–395 (2016). https://doi.org/10.1038/hr.2016.11
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.11
Keywords
This article is cited by
-
The effects of obstructive sleep apnea on blood pressure variability and load in patients with hypertension
Sleep and Breathing (2024)
-
Chemogenetic inhibition of NTS astrocytes normalizes cardiac autonomic control and ameliorate hypertension during chronic intermittent hypoxia
Biological Research (2023)
-
Obstruktive Schlafapnoe und arterielle Hypertonie
Somnologie (2023)
-
Extracellular Vesicles Derived from Intermittent Hypoxia–Treated Red Blood Cells Impair Endothelial Function Through Regulating eNOS Phosphorylation and ET-1 Expression
Cardiovascular Drugs and Therapy (2021)
-
The additive effects of OSA and nondipping status on early markers of subclinical atherosclerosis in normotensive patients: a cross-sectional study
Hypertension Research (2019)