Abstract
Injured patients with lung contusion (LC) are at risk of developing bacterial pneumonia (PNA) followed by sepsis and death. A recent genome-wide association study (GWAS) showed FER gene expression positively correlating with survival rates among individuals with above conditions. We sought to determine whether electroporation (EP)-mediated delivery of FER gene could indeed improve survival, in a lethal model of combined LC and PNA. C57BL/6 mice sustained unilateral LC, which preceded a 500 Klebsiella colony forming unit (CFU) inoculation by 6 h. In-between these insults, human FER plasmid (pFER) was introduced into the lungs followed by eight EP pulses applied externally (10 ms at 200 V cm−1). Control groups included EP of empty vector (pcDNA3) or Na+/K+-ATPase genes (pPump) and no treatment (LC+PNA). We recorded survival, histology, lung mechanics, bronchial alveolar lavage (BAL) fluid, FER and inflammatory gene expression and bacteriology. The data show that 7-day survival was significantly improved by pFER compared with control groups. pFER increased BAL monocytes and activated antibacterial response genes (nitric oxide synthase (NOS), Fizz). pFER treatment showed decreased lung and blood Klebsiella counts reaching, in some cases, complete sterilization. In conclusion, FER gene delivery promoted survival in LC+PNA mice via recruitment of activated immune cells, improving efficiency of bacterial clearance within contused lung.
Similar content being viewed by others
Introduction
Trauma to the chest produces lung contusion (LC) injury, impairs lung function and accounts for a significant number of admissions to adult intensive care units. Findings from our laboratory have shown several immunological and physiological derangements in the lung following LC that increase the susceptibility of these patients to develop severe bacterial pneumonia (PNA).1, 2, 3, 4, 5 The combination of LC and PNA can lead to severe respiratory failure with need for endotracheal intubation and mechanical ventilation support. LC patients are at high risk for PNA, sequential sepsis and adult respiratory distress syndrome. Despite improvements in critical care, severe adult respiratory distress syndrome continues to be associated with significant (~40%) mortality.6, 7 Elderly patients are increasing in prevalence and are at an elevated risk for falls and subsequent complications from traumatic injury. In the injured elderly (>65 years of age), the presence of rib fractures from traumatic closed chest injury is associated with an odds ratio of dying of 1.98 (1.86–2.11, 95% CI). The odds ratio of mortality in the elderly increases dramatically to 5.24 (3.51–87.82, 95% Cl) when combined with the presence of PNA.8
Klebsiella is an important pathogen of the so-called ESKAPE organisms (Enterococcus faecium, Staphylococcus aureus/MRSA, Klebsiella pneumoniae, Acintenobacter baumannii, Pseudomonas aeruginosa and various Enterobacter species), all constitute the bulk of nosocomial infections worldwide and are particular associated with high mortality; thus, studying their pathogenicity and virulence in clinical relevant models of lung injury simulating susceptible populations is extremely important.2, 9, 10
A recent genome-wide association study (GWAS) from four independent cohorts showed that common variants of the FER gene were strongly associated with a reduced risk of death from sepsis due to PNA.11 The true functional significance of FER is highly controversial and the subject of great debate. FER is an evolutionary conserved, ubiquitously expressed, non-transmembrane receptor tyrosine kinase within the fes/fps family.12 It has been described in normal tissues to be a downstream integrator of membrane and cytosolic signaling pathways13, 14, 15 boasting a beneficial participation in cell survival, cytoskeleton re-arrangement, epithelial maintenance and leukocyte differentiation and chemotaxis. However, in several cancer models, FER has been implied to be involved in mechanisms of malignant cell transformation, tumoral invasion and metastatic potential.16, 17, 18, 19 FER overexpression is a negative predictor of survival in non-small cell lung cancer.20 This ambivalent characteristic suggests that FER is tightly regulated. Interestingly, its role in lung acute inflammatory states has never been extensively studied.
It has been proposed that transient genomic editing and manipulation of protein expression by gene therapy can potentially restore known altered aspects of lung biology that favor resolution of lung injury.21, 22, 23 However, in the injured lung, traditional viral techniques may worsen inflammation and could be neutralized by natural lung physical and immunological barriers that prevent such transfection.24 To circumvent these challenges, our laboratory has adopted in vivo electroporation (EP) as a simple, reproducible and inexpensive method of gene transfer. The possible events of in vivo EP have been elegantly described elsewhere.25, 26 In the lung, it confers advantages over other gene therapy techniques, among these the lack of inflammation, as well as the lack of integration into the chromosome making transgene expression transient and short-lived, ideal for the resolution of acute lung injury without concern for long-term effects or mutagenesis.21, 27 We have been successful in achieving high levels of expression in both naive and injured lungs by using in vivo EP.22, 27, 28, 29 Furthermore, we have shown that EP-mediated delivery of genes of the Na+/K+-ATPase pump, an important regulator of water and salt balance in the lung, was successful in reducing lung edema and inflammation after lipopolysaccharide or LC insults.
In this study, we examined the role of EP-mediated delivery of the FER gene in an acutely injured lung. We hypothesized that EP-mediated delivery of the FER gene would improve survival in our lethal murine model of trauma complicated by PNA. The data presented here indicate a favorable phenotypic induction with survival advantage given by EP-mediated delivery of FER gene, characterized by recruitment of inflammatory monocytes and upregulation of bactericidal response gene activity. This outcome yielded an improved capacity to clear the lung of bacteria and decrease subsequent inflammation. We describe a promising alternative strategy toward the resolution of acute lung injury and a complementary treatment to antibiotics for severe trauma-related secondary bacterial PNA.
Results
The following describes a transient 1- to 2-day increase in expression of human FER tyrosine-kinase gene introduced by EP-mediated gene transfer of a naked DNA plasmid encoding human FER (pSG5-FER) into injured mouse lungs.
FER gene delivery by EP increases FER transcription and FER protein expression in areas of contusion-damaged lungs
Initially, we sought to delineate whether EP-mediated delivery of FER gene would be successful at clearing bacteria in severely damaged lungs after unilateral LC injury followed by bacterial PNA. At 24 h, harvested right contused lung lobes (Figure 1d) were subjected to immunohistochemistry to reveal the expression of FER post EP of pSG5-FER and control plasmids encoding Na+/K+ ATPase or pcDNA3. In Figure 1, the immunofluorescent stained specimens depict overexpression of FER in bronchial airway epithelial cells, underlying bronchial stromal tissue (panel a) and in lung parenchyma cells (panel b) only in the pFER electroporated treatment group. Very minimal background expression could be seen in the electroporated Na+/K+-ATPase gene group, whereas all other control groups had no evident signal (data not shown). In bronchial alveolar lavage (BAL) fluid and total lung lysates, we performed real-time PCR (RT-PCR) assays showing increased transcription of human transgene FER at 24 h (Figure 1e). This expression correlated with western blot data showing increased total protein FER at 24 h within the FER electroporated group and increased phosphorylated isoform of FER at 72 h, confirming gene transfer (Figure 1f).
Expression of FER after EP-mediated gene transfer of PSG5-FER plasmid in murine model of LC injury and PNA. FER expression localization by immunohistochemistry on frozen sections of right lung lobe: (a) airway; (b) alveoli; (c) FER expression in the Na+/K+-ATPase gene electroporated group in similar injury conditions; (d) aspect of lungs at 24-h time point after unilateral (right-sided) contusion followed by administration at LC+PNA group; (e) Western blot; (f) Quantitative RT-PCR (N=10 mice per group). Statistical analysis performed by one-way ANOVA followed by Tukey's multiple comparison test; *P<0.01.
EP-mediated delivery of FER gene decreases injury and inflammation following combined LC and PNA
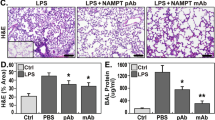
Histological analysis
We performed assessment of the distinct area of injury distributed among the right contused lung lobes in animals at 24 h (Figures 2b, d, e and f). Histological evaluation of these contused areas showed extensive hemorrhage, infiltration of inflammatory cells with pulmonary consolidation, proteinaceous exudate, decreased airspaces and edema. After LC, infiltrative cells are predominantly mononuclear in nature and neutrophils are very low in number (panel b). In contrast, when bacteria are inoculated into the lungs, neutrophils are rapidly recruited (panel c). The inflammatory response is vastly amplified in the combined LC+PNA model of injury (panel d). Thus, the deleterious effects of LC injury and bacterial PNA appear to be summative as measured with the American Thoracic Society Lung Injury Scoring System.30 After EP of either Na+/K+ ATPase or FER gene, we observed a relative reduction of tissue inflammation characteristics present in the parenchyma as compared with LC+PNA animals (Figures 2e and f).
Lung histology. Hematoxylin and Eosin-stained lung sections at 24 h after 500 CFU Klebsiella pneumoniae administration and/or 30 h post LC injury. (a) Uninjured-Naive; (b) LC only; (c) PNA only; (d) LC plus PNA; (e) LC plus EP of the Na+/K+-ATPase gene followed by PNA; (f) LC plus EP of FER gene followed by PNA; (g) American Thoracic Society Lung Injury Score; (h) Inflammatory cell infiltrate per high power field (× 100). Microphotographs were obtained from contusion portion of right mouse lung. Right lung lobes in Uninjured-Naive and PNA-only groups were also used for comparison. Significant inflammation characterized by inflammatory cell infiltrate, intra-alveolar hyaline membrane (proteinaceous deposit), cellular debris and interstitial septal edema was found and separate components were used to score severity of lung injury blindly. Inflammatory response was mitigated in the FER-treated group, less so in the Na+/K+-ATPase group. Bar represents 50 μm (× 20). N=3 mice per group. Statistical analysis performed by one-way ANOVA followed by Tukey's multiple comparison test; 5 fields per lobe.
Alveolar-capillary integrity
At the 24-h time point, ELISAs measuring the levels of albumin in BAL were elevated in all groups compared with the naive controls (Figure 3), indicating different degrees of severity from lung permeability injury and alveolar-capillary disruption. LC injury with ensuing PNA had the highest level of permeability injury as compared with PNA exposure alone. In animals with these combined injury insults, treatment with EP-mediated delivery of Na+/K+-ATPase gene was able to show a significant reduction of BAL albumin levels at 24 h after injury, consistent with our previously reported data in lipopolysaccharide-only and LC-only injury models.28, 29 Importantly, FER gene delivery was also able to show this positive effect in reducing the degree of permeability injury as compared with controls.
Levels of albumin present in BAL fluid as a measure of lung permeability injury 24 h after administration of 500 CFU Klebsiella pneumoniae and 30 h after LC. N=6–8 mice per group. Statistical analysis performed by one-way ANOVA against naive (bracket ***P<0.0001) and post hoc Tukey's multiple comparison test. *P<0.05.
Pressure–volume curves
EP-mediated delivery of both FER and Na+/K+-ATPase genes showed favorable responses in quasi-static pressure–volume (P–V) curves (Figures 4a and b) generated over 4000 data points with the SCIREQ Flexivent ventilator. This indicates better compliance and higher inflatable volume at Pressure-30 (TLC-30) than the LC+PNA control (Figures 4c and d) in the assessed time points. For the LC+PNA-only control group, the large separation found between the inspiratory and expiratory limbs of the curve signified a larger driving pressure needed to open areas of atelectatic lung, making these lungs, in theory, more susceptible to atelectrauma.31 Both gene therapy treatments, either Na+/K+-ATPase (to reduce edema) or FER (to reduce inflammation), showed smoother and parallel curves indicating much more harmonic ventilation.
P–V curves after established combined injury of LC and PNA. (a) P–V curves at 24 h. (b) P–V curves at 72 h. (c) Total lung capacity (TLC) at 30 cm H2O pressure at 24 h after PNA. (d) TLC at 30 cm H2O pressure at 72 h. Using a SCIREQ FlexVent (Montreal, Canada) quasi-static P–V curves with a maximal inflation to 30 cm H2O were generated from over 4000 data points. Bottom half of each loop represents the inspiratory portion of a P–V curve perturbation maneuver. Top half represents the expiratory portion of each graph. LC+PNA reduces overall compliance requiring higher pressures to open the same amount of lung units than other groups. Representative curve from uninjured group for same age cohort animals. Both the Na+/K+-ATPase and FER gene delivery were effective in improving lung mechanics at 24 and 72 h as compared with control. N=6–8 mice per group. Analysis of results for the Naive, LC-only, LC+PNA, LC+pPump+PNA and LC+pFER+PNA groups was performed using one-way ANOVA (P<0.001).
BAL fluid cytology
LC, PNA and combo LC+PNA conditions resulted in the production of a significant inflammatory response discernable by changes in cellular subpopulations in BAL. At 24 h, in LC-only conditions, analysis of cytospin slides stained with Diff-Quik revealed significant recruitment of macrophages and sparse recruitment of neutrophils. Seventy-two hours after the same condition (LC only), the majority of cells appear as apoptotic macrophages, indicating the resolution of trauma-related sterile inflammation (Figures 5b and g). In contrast, mice challenged both with LC+PNA demonstrated equal recruitment of macrophages and neutrophils in BAL within 24 h post PNA challenge (Figure 5c). The response was continued at 72 h (Figure 5h), illustrating the non-resolution of inflammation. For animals receiving EP-mediated delivery of Na+/K+ ATPase genes under similar combined injury conditions, we found an elevated number of macrophages in BAL and almost a complete absence of neutrophils (Figure 5d). This neutropenic response to LC+PNA was persistent in the Na+/K+ ATPase group at 72 h with significant ghost cells (dead necrotic cells) present in BAL (Figure 5i). The EP-mediated delivery of FER gene was distinguishable from all other groups in showing a greatly boosted immune response, with equally recruited and relatively larger numbers of macrophages and neutrophils at 24 h post PNA challenge (Figure 5e). This response, however, is not lasting and by 72 h post PNA, the FER electroporated group shows a return of the BAL cellular populations to almost baseline pre-injury characteristics with much lower number of macrophages and absence of neutrophils, suggesting resolved infection and inflammation (Figure 5j).
Flow cytometry
Flow-cytometry experiments (Figure 6) confirmed the observations from our cytospin slides. Our data suggest that EP of FER gene delivery stimulated a multi-lineage cellular response in BAL, with a predominance in the number of inflammatory monocytes (GR-1+; F4/80+) at all time points. As for assessing for neutrophils (GR-1+; F4/80-), the EP of Na+/K+-ATPase-treated group showed a noticeable reduction in their numbers at both 24 and 72 h, whereas the FER-treated group had an initial peak at 24 h which rapidly dropped by 72 h. In regards to macrophages (GR-1−; F4/80+), no differences were seen in the first 24 h among groups; however, these were significantly increased in LC+PNA group at 72 h.
Flow-cytometric analysis of BAL cells shows that FER gene therapy works by enhancing the lung immune system. Cell counts and types of cells present in equal volumes of BAL fluid as identified using flow cytometry. Samples were collected at 24 and 72 h after administration of Klebsiella. N=5 mice per group, 1 00 000 cells per sample. Analysis of results for the LC+PNA, LC+pFER+PNA and LC+pPump+PNA groups was performed using one-way ANOVA followed by Tukey’s multiple comparison test. *P<0.05 post hoc test.
EP-mediated gene delivery of FER was associated with increased survival following combined LC and PNA
Survival curve data
PNA induced by Klebsiella pneumoniae (500 colony forming units (CFUs)) post LC dramatically increased mortality. None of the animals died from LC alone (data not shown). The EP of FER plasmid resulted in 90% 7- day survival, which was significantly different (P=0.004, log-rank test) from all other groups: LC+PNA group (20% survival; P<0.003); LC+Na+/K+-ATPase pump genes EP-treated group+PNA (0% survival; P<0.001) (Figure 7a). To assess that the survival benefit was not related to the EP of a non-specific plasmid DNA, two additional groups were EP-treated. One group was delivered with an empty plasmid DNA and another one was delivered with a reporter gene (luciferase) plasmid DNA under same injury conditions. However, neither of these groups had increased survival outcomes after LC and PNA injury (Figure 7b).
Survival curve data. (a) EP of FER significantly enhanced (P=0.004, log-rank test) survival in the settings of LC and PNA. Survival after LC followed by 500 CFU Klebsiella pneumoniae created 6 h after chest injury. LC+PNA: LC and PNA; LC+pPump+PNA: LC followed by EP-mediated delivery of genes for the Na+/K+-ATPase pump followed by PNA; LC+pFER+PNA: LC followed by EP-mediated delivery of human FER gene followed by PNA. (b) EP of empty plasmid or luciferase plasmid was out of survival benefit. N=10 mice per group. Significance placed in graph. Log-rank (Mantel–Cox) test.
FER gene therapy significantly reduced Klebsiella pneumoniae counts in blood circulation and lungs
Whole blood and lung tissue were assayed for the formation CFUs of Klebsiella pneumoniae normalized to 1 ml of blood and total lung tissue, respectively (Figure 8). Not surprisingly, in the LC+PNA group bacterial counts had a 1-log increase between 24 and 72 h, especially in blood, confirming continued uncontrolled multiplication of organisms and suggesting probable death due to invasion and sepsis at later time points. EP of FER was very effective in suppressing bacteria from reaching blood circulation at all time points. Only 3 out of 18 animals revealed a positive culture in any of time points assessed. While the EP of Na+/K+ ATPase was able to contain bacterial blood invasion at 24 h, this effect was lost at 72 h. At 24 h post PNA delivery, EP-mediated transfer of both Na+/K+ ATPase and FER genes showed capacity to inhibit bacterial growth in the lung; however, only FER was capable of a statistically significant decrease in CFUs. Importantly, FER was able to completely clear infection of several animals at 72 h.
Whole blood and lung tissue culture to quantify bacterial CFUs assay. EP of FER significantly suppressed bacteria in the lung and in circulation. EP of Na+/K+-ATPase was also efficient in suppressing bacteremia but was time limited only for 24 h. Meanwhile, FER-treated animals continue to avoid major bacteremia at 72 h and cleared bacteria from 6 out of 11 animals. N=10–11 mice per group. (circle) LC+PNA; (triangle) LC+EP-pPump+ PNA; (square) LC+EP-pFER+PNA; bar indicates median for each group. Statistical analysis performed by one-way ANOVA and post hoc Tukey's multiple comparison test.
EP-mediated delivery of FER induces expression of antibacterial response genes in BAL and lung cells
Noting the increase in recruitment of inflammatory monocytes upon FER EP, we set out to perform RT-PCR. We found that EP-mediated delivery of FER showed a significantly enhanced expression of Nos-2, Fizz1 and interleukin 1 beta (IL-1β) in BAL cells (Figure 9a) known genes to be critical in the fight against bacterial infection in the lung. Additionally, we looked at the expression of these genes within washout lung parenchymal tissue and found that Nos-2, IL-1β and TNF-α expression was significantly higher in the FER group (Figure 9b), suggesting that these activation effects were also present in interstitial macrophages and other inflammatory cells distributed within lung tissue and thus primed to create a second barrier of protection against bacterial invasion.
Expression of key genes, involved in antibacterial immune response, is enhanced after EP-mediated delivery of FER gene in BAL cells and lung parenchyma tissue. RT-PCR TaqMan indicates that FER gene therapy produces a boost in nitric oxide synthase 2 (NOS-2) and similar genes (Fizz1, IL-1β and IL-6) at 24 h indicating a potentiated immune system to fight infection. N=3–10 mice per group. Statistical analysis performed by one-way ANOVA.
Overexpression of FER did not induce fibrosis or epithelial mesenchymal transformation in the lung
Mice with LC and PNA and who had EP-mediated delivery of FER gene surviving over 7 days were killed, and their lungs were subjected to Masson’s Trichrome staining (Figure 10). All areas of the lung were assessed. On the basis of our model, the right lung (subject to contusion) still had mild evidence of inflammation; however, there was no evidence of excess fibrosis or collagen deposition as compared with bleomycin control. EP delivery of human FER gene and its expression did not linger nor did it induce mesenchymal transformation or a fibrosis type of recovery in these treated lungs.
Masson’s Trichrome staining does not show excess fibrosis or mesenchymal epithelial transformation in lungs of FER-treated survivors. Areas representative in the graphs are right LC with PNA (compare with Figure 1d) and surviving after treatment with EP-mediated delivery of FER gene. Bleomycin a known induction agent for pulmonary fibrosis was used as a positive control after harvesting animal at 8 days post insult. N=3 mice per group.
Discussion
The use of FER EP therapy was effective in containing bacterial infection within the lung and resulted in prevention of bacteremia following LC injury. Moreover, a single application of FER was able to boost host immune response counteracting known deleterious effect of LC injury and PNA.2, 5 Unfortunately, the alternative Na+/K+ ATPase gene delivery therapy, previously reported to be beneficial in reducing lung edema and inflammation in the settings of sterile models of LC and lipopolysaccharide injury,28, 29 was not protective against secondary Klebsiella pneumonia. On the basis of BAL cytospin and flow-cytometry experiments, our findings suggest that the overexpression of Na+/K+ ATPase induces an excessive inhibition of neutrophilic recruitment, impeding bacterial clearance. In consequence, as bacteria multiply they will overwhelm lung barriers allowing bloodstream invasion and animals will die from sepsis as seen in the survival experiments.
Following LC, there are several pathological features that increase the susceptibility of the lung to PNA and affect severity. LC injury produces an area of epithelial disruption causing alveolar hemorrhage, which constitutes an excellent culture media for bacteria.2, 32 The presence of a protein-rich exudate interferes with surfactant lipids, changing surface-tension properties within alveoli and thus inhibiting immune protective effects. The loss of integrity of the epithelial barrier permits the invasion of microorganisms into the bloodstream causing bacteremia and sepsis. Our laboratory has previously reported that LC injury also forges a depletion of alveolar macrophages and is an important feature in potentiating the vulnerability of lungs to fulminant infection.2, 5 Therefore, the development of short-lasting gene therapy to counter this phenomena and boost the host’s a balanced response against bacterial PNA is of therapeutic interest.33, 34, 35
EP is an effective technological platform for introducing genes into both intact and diseased lung
EP technology has been around for almost 40 years with the first report of single cell EP in 1982.36 However, it is only recently that is has been considered for clinical application. As mentioned in comprehensive review by Mir,26 there are not only technological hurdles present to be solved with smart biomedical engineering but it also requires a significant change in heart and acceptance in medical society. In regards to lung EP, we have recently demonstrated that external chest EP achieves high expression levels of newly introduced genes in the lung, comparable to other leading viral vector techniques.27 Using reporter gene assays, we have demonstrated extensive expression throughout many pulmonary cells (alveolar epithelia, bronchial epithelia, bronchial/vascular smooth muscle).22 One of the greatest advantages of EP over viruses is that it does not increase inflammation levels in the surrounding tissues. A second advantage is that its activity is only limited to the area of electrical field, thus avoiding potential systemic effects derived from vector dissemination. Studies from the laboratory of David Dean have demonstrated the applicability of this method of gene delivery in large animal models such as swine.37 The amount of energy used has been calculated in 0.2 J kg−1, much less than defibrillators in hospital practice.38 Our preliminary data have also shown that EP can effectively introduce therapeutic gene(s) not only into the intact, but also the injured lung.27, 28, 29 This opens the possibility of EP-mediated gene transfer to be translated into clinical applications.
FER gene expression improved survival from death related to LC complicated by PNA
Our results support the recent GWAS that points to enhanced expression of common variants FER gene and reduced the risk of death by 44% from sepsis due to PNA.11 Although no particular mechanism was described in this population study, it was suggested that FER could been implied in the regulation of host defense mechanisms along with preservation of epithelial and endothelial barrier function, which could explain many of its protective effects.12, 39, 40, 41, 42, 43, 44, 45
In our experimental model, we found that innate defense mechanisms were indeed enhanced with EP-mediated delivery of FER gene. This was not found in the similarly EP-delivered Na+/K+-ATPase gene group, implying gene specificity and that it is not a side effect of EP pulses and/or the presence of foreign DNA (a known stimulator of TLR-8). The overexpression of FER showed a rapid recruitment of inflammatory monocytes at 24 h. Additionally, Nos-2 and FIZZ1, genes important for white blood cells’ bactericidal activity, were increased after single EP treatment of FER.
The role of FER gene in normal lung biology and its function during acute inflammatory lung states has not been studied in detail. Fps/Fes and FER are the only known members of a distinct subfamily of the non-receptor protein-tyrosine kinases. These proteins have autocatalytic properties that induce phosphorylation of their own SH-2 domains, as well as similar domains belonging to other membrane bound tyrosine kinases.13, 15, 18, 46, 47 Many studies indicate that these kinases have roles in regulating inside-out signaling that accompany receptor-ligand, cell-matrix and epithelial-immune cell interactions in the gut,42 which are probably of equal importance in lung epithelia. Using a kinase-deficient transgenic model, significant but non-lethal intestinal epithelial disruption and exaggerated neutrophilia were found after insult.42, 45, 48, 49 Other authors have observed that members of this family are important in myeloid cell recruitment and differentiation.14, 41, 49
We recognize several limitations to our study that need to be pointed out. First, we have yet to identify the actual downstream effectors of FER expression in this particular model lung injury and gene transfer. Future experiments involving transgenic kinase-deficient mice and adoptive cell transfer are planned that will allow to further ascertain the mechanisms of FER-induced host response in this model. Second, we have yet to know whether these protective effects can be expanded to other bacterial species, especially of the ESKAPE spectrum. This therapy will need to be empirically tested against these organisms in this murine model as well as other larger animal models of lung injury.
Knowing the reported association as a negative predictive marker for cancer survival in non-small cell lung cancer and addressing any other safety concerns we performed histological analysis of 10-day survivors after FER treatment. We did not find any major dysplastic, fibrotic or mesenchymal transformation features in electroporated lungs. Our RT-PCR and western blot data also showed a very limited, short-lived expression of FER, which is ideal in our disease model of critical illness. These observations, in combination with findings from other investigators showing that gene expression driven by viral promoters (like SV40 such as in this case) is deactivated rapidly,21, 50, 51 should not prohibit the use of FER gene delivery for fear of malignant transformation. As plasmid DNA rarely integrates unassisted into the host chromosome, concerns for mutagenesis and activation of other oncogenes should be minimal.
In summary, the transient increase of FER expression was advantageous in successfully clearing bacterial PNA complicating LC. The FER-treated mice displayed 90% survival compared <20% survival among control groups, thus supporting the findings from the GWAS of the beneficial role of FER expression in sepsis and PNA.
Materials and methods
Animals
Male C57BL/6 wild-type mice (Harlan, Indianapolis, IN, USA) were used in all experiments. Mice were housed under specific pathogen-free conditions and were allowed a 1-week acclimation period to their new surroundings before being used in experiments. All experiments were performed in accordance with National Institutes of Health guidelines for care and use of animals. Approval for of all experimental protocols was obtained from the University of Michigan Committee on Use and Care of Animals (UCUCA) and the Institutional Biosafety Committee (IBC).
LC injury
We followed modified methods as described by Hoth et al.52 At time minus 6 h, a unilateral blunt LC injury was induced using an electric cortical contusion impactor apparatus.23, 35 Procedural details for the closed chest LC injury model have been described extensively in previous publications from our laboratory.2, 3, 29, 35, 53 All animals received buprenorphine immediately after contusion to avoid post-treatment discomfort. Mice were then allowed to recover spontaneously.
Recombinant plasmid DNA
pSG5-FER (human FER tyrosine kinase) plasmid was purchased from Addgene (Cambridge, MA, USA) and propagated in E. coli. Plasmids were then harvested using QIAGEN Giga-prep kits (Valencia, CA, USA)54 as per manufacturer’s instructions. Original pSG5-FER plasmid was a gift from Nora Heisterkamp deposited in Addgene DNA repository (Addgene plasmid # 30191).54 The plasmid contains an insert that encodes human FER (hFER), which is a non-receptor tyrosine kinase located on human chromosome 5q21 (Gene ID 2241; HPRD 01491; NM_005246). Two separate plasmids containing the α and β subunits of the Na+/K+-ATPase were a gift from David A Dean (University of Rochester, NY) and were harvested in a similar manner as described above. A luciferase reporter gene plasmid (Promega, Madison, WI, USA) was used as a control for effects of EP process over results, containing similar promoter sequence of the FER plasmid (SV40). Similarly, an empty plasmid (pcDNA3) was used for same purposes in survival curve experiments.
All plasmids of DNA were stored in 10 mm Tris–1 mM EDTA buffer (pH 8.0) at −20 °C until the day of gene delivery. Protocols for the use of recombinant DNA technology required prior approval from the University of Michigan Institutional Biosafety Committee (IBC).
EP-mediated delivery of genes into mouse lungs
EP-mediated gene transfer was performed on the same day of injury, in-between LC and deep oral delivery of bacteria. We modified methodology as described by Dean et al.27 and Machado-Aranda et al.23 Briefly, 150 μg of DNA suspended in 100 mm NaCl was delivered to the lungs via hypopharyngeal drop in anesthetized animals. After several regular breaths, metal plated electrodes were placed under each forelimb assuring contact with an electroconductive gel. Using a BTX Harvard Apparatus ECM 830 generator (Holliston, MA, USA), eight square wave EP 200 V cm−1 pulses of 10 ms duration and 1 s apart were given. Animals were allowed to recover while kept under BSL2 containment.
Induction of secondary bacterial PNA
Six hours after LC injury and lung EP, we administered Klebsiella pneumoniae, strain 43816, serotype 2 (American Type Culture Collection, Manassas, VA, USA). We followed our previously reported methodology of combined LC and PNA, which produces consistent and significant (>80% at 7 days).2, 55, 56 Appropriate serial dilutions were subsequently performed to achieve a concentration of 500 CFUs of bacteria per 30 μl of inoculum, which corresponds to LD50 for C57/Bl6 mice using this particular strain of Klebsiella. Administration of 30 μl of bacterial suspension was performed via deep oral injection into the trachea under isoflurane anesthesia. Animals were allowed to recover spontaneously and transported back to BSL2 housing where animal health and survival data were recorded every 8 h.
Lung mechanics measurements and BAL collection
Based on luciferase reporter gene assays (data not shown) and in parallel to survival curve generation experiments, we selected two time points, one before (24 h) and one after (72 h) after the peak of maximal expression (48 h) of luciferase under similar injury conditions. At these time points, mice were killed and a tracheal cut down was performed. A blunt metal tube was inserted gently into the trachea and connected to the circuit of a FlexiVENT ventilator (Montreal, QC, Canada) and ex vivo ventilation was initiated as described in Mutlu et al.28 A quasi-static P–V curve was obtained after an initial recruitment maneuver to a pressure of 30 cm H2O and recorded three times during a 15 min ventilation course. Immediately afterwards, the lungs were lavaged with 1.5 ml of sterile phosphate-buffered saline (PBS) using several 1 ml syringes. BAL fluid was centrifuged at 400 g for 8 min. Following centrifugation, supernatant was separated from precipitated cells, and stored frozen at −80 °C until use. Spun down cells were resuspended in appropriate buffer and used either in flow cytometry assay or for quick staining.
Quantitative bacterial culture assessments
Blood culture
In separate experiments, at similar time points as above, animals were killed according to UCUCA Approved Protocol. Blood was obtained via cardiac puncture using a sterile 18-gauge needle. To measure bacteria titers in blood, 100 μl of undiluted blood was plated onto 5% sheep blood agar plates (Thermo Fisher Scientific, Remel Products, Lenexa, KS, USA). Plates were incubated overnight at 37 °C and CFUs per ml of blood were counted after 16 h.
Total lung tissue culture
Additionally, the thoracic cavity was opened and right ventricle and trachea were cannulated, and lungs were flushed of blood via right heart with 2 ml of ice-cold PBS. Both lungs were removed and homogenized in 1 ml of ice-cold PBS. Serial 10-fold dilutions were made then made in the same buffer and 100 μl volumes of homogenate were plated on 5% blood agar plates. Plates were incubated overnight at 37 °C and CFU per total lung tissue was counted after 16 h. If no colonies were present, then culture plates were kept for additional 48 h in the incubator to confirm no growth of delayed organisms.
Cytospins BAL cell staining
Cytospins were performed by loading 100 μl from spun down BAL into each cuvette and spinning against glass slides at 350 g for 5 min. Slides were fixed with Diff-Quik (Baxter, Detroit, MI, USA) based on Wright-Giemsa stain for microscopic examination.
Flow cytometry
Flow-cytometric analysis of 1 00 000 cells per sample was performed using a BD LSR II Flow Cytometer (BD Biosciences) following protocol as described in Dolgachev et al.56 and using the following antibodies Gr-1-PE, CD11c-APC-Cy7, F4/80-AF488, CD11b-PE-Cy7 and CD206-APC (BioLegend and BD Biosciences, San Jose, CA, USA). Obtained data were plotted and analyzed using the FlowJo software (Tree Star, Inc., Ashland, OR, USA).
Western blot analysis
For FER expression determination, whole-lung extracts were run on 12.5% SDS-polyacrylamide gels, with detailed protocol for sample processing as described in our previous publications.4, 53, 57, 58 Polyvinylidene difluoride membranes were probed sequentially with rabbit anti-FER or anti-phospho-FER (1:2000); followed by horseradish peroxidase-conjugated anti-rabbit IgG antibodies (1:3000) (AbCAM, Cambridge, MA, USA). We used actin as a loading control using mouse anti-actin (1:100) (AbCAM) followed by secondary as described above. Proteins were visualized by chemiluminiscense (Super Signal West Pico chemiluminescent substrate, Pierce, Rockford, IL, USA) using a Kodak photo imager.
Real-time PCR
In parallel experiments, from control and experimental group animals under same injury conditions, treatments and time points as described above, after euthanasia the chest cavity was opened. Cannulating the heart, lung circulation was perfused blood free with ice-cold PBS before their removal from chest cavity. RNA was isolated from the upper right lobes of lung using TRIzol (Ambion, Invitrogen, Carlsbad, CA, USA) and from BAL cells using Qiashredder columns (QIAGEN) as per manufacturer's instructions. Levels of mRNA for FIZZ1, Arginase 1, nitric oxide synthase 2 (inducible) (NOS-2), interferon gamma (IFN-γ), IL-1β and IL-10 were assessed using quantitative PCR analysis (TaqMan) with predeveloped primers and probe sets (Applied Biosystems, Carlsbad, CA, USA). Quantification of the genes of interest was normalized to GAPDH and expressed as fold increases over the negative control for each treatment at each time point.
Histopathological examination and Masson’s trichrome staining
At 24-h post insult, lungs of individual mice were fixed in 4% formaldehyde solution, and then 4-μm thick sections were cut, stained with hematoxylin and eosin and examined by light microscopy. Slides (four for each group) were sent to be analyzed blindly by our resident pathologist measuring parameters to achieve a composite Lung Injury Score, as stated in the consensus document from the American Thoracic Society.30 Representative pictures were taken at × 600 magnification using Tx2 Nikon microscope (Nikon Instruments Inc., Melville, NY, USA). Long-term survivors (10 days) were killed and lung were extracted and processed as above and following methods described elsewhere59 for Masson’s Trichrome staining. Pulmonary fibrosis was induced by single introduction of 2.5 U kg−1 of bleomycin intratracheally at animals and animals killed at comparable time point of long-term survivors.
In parallel experiments, right lungs of mice from electroporated and control groups were obtained at 24-h post PNA and 4-μm frozen sections were stained using α-FER (Abcam, cat#AB191060) and secondary α-rabbit-Alexa-594 (Invitrogen-Molecular Probes) following manufacturer instructions to demonstrate localization of expression after EP.
Statistical methods
All statistical analysis and graphs were performed using GraphPad Prism 5.0 software (GraphPad Software, La Jolla, CA, USA). Results are presented as mean values±the s.e.m. unless otherwise noted. Continuous variables were analyzed using an unpaired two-tailed Student’s t-test. Multiple groups were compared by one-way ANOVA with Tukey’s multiple comparison test used for post hoc analysis or two-way ANOVA with Bonferroni posttests. Survival curves were generated using the Kaplan–Meier method. The log-rank (Mantel–Cox) Test was used to compare the survival data between experimental groups. Statistical significance was defined as a P-value of <0.05.
References
Raghavendran K, Davidson BA, Woytash JA, Helinski JD, Marschke CJ, Manderscheid PA et al. The evolution of isolated bilateral lung contusion from blunt chest trauma in rats: cellular and cytokine responses. Shock 2005; 24: 132–138.
Dolgachev VA, Yu B, Reinke JM, Raghavendran K, Hemmila MR . Host susceptibility to gram-negative pneumonia after lung contusion. J Trauma Acute Care Surg 2012; 72: 614–622; discussion 22-23.
Machado-Aranda D, Wang Z, Yu B, Suresh MV, Notter RH, Raghavendran K . Increased phospholipase A2 and lyso-phosphatidylcholine levels are associated with surfactant dysfunction in lung contusion injury in mice. Surgery 2013; 153: 25–35.
Suresh MV, Ramakrishnan SK, Thomas B, Machado-Aranda D, Bi Y, Talarico N et al. Activation of hypoxia-inducible factor-1alpha in type 2 alveolar epithelial cell is a major driver of acute inflammation following lung contusion. Crit Care Med 2014; 42: e642–e653.
Machado-Aranda D, V Suresh M, Yu B, Dolgachev V, Hemmila MR, Raghavendran K . Alveolar macrophage depletion increases the severity of acute inflammation following nonlethal unilateral lung contusion in mice. J Trauma Acute Care Surg 2014; 76: 982–990.
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M et al. Incidence and outcomes of acute lung injury. N Engl J Med 2005; 353: 1685–1693.
Villar J, Sulemanji D, Kacmarek RM . The acute respiratory distress syndrome: incidence and mortality, has it changed? Curr Opin Crit Care 2014; 20: 3–9.
Battle CE, Hutchings H, Evans PA . Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury 2012; 43: 8–17.
Taylor AP . Serious putty. The Scientist 2016; 2016: 15–16.
Hidron AI, Edwards JR, Patel J, Horan TC, Sievert DM, Pollock DA et al. NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006-2007. Infect Control Hosp Epidemiol 2008; 29: 996–1011.
Rautanen A, Mills TC, Gordon AC, Hutton P, Steffens M, Nuamah R et al. Genome-wide association study of survival from sepsis due to pneumonia: an observational cohort study. Lancet Respir Med 2015; 3: 53–60.
Hao QL, Ferris DK, White G, Heisterkamp N, Groffen J . Nuclear and cytoplasmic location of the FER tyrosine kinase. Mol Cell Biol 1991; 11: 1180–1183.
Senis YA, Sangrar W, Zirngibl RA, Craig AW, Lee DH, Greer PA . Fps/Fes and Fer non-receptor protein-tyrosine kinases regulate collagen- and ADP-induced platelet aggregation. J Thromb Haemost 2003; 1: 1062–1070.
Sangrar W, Gao Y, Bates B, Zirngibl R, Greer PA . Activated Fps/Fes tyrosine kinase regulates erythroid differentiation and survival. Exp Hematol 2004; 32: 935–945.
Sangrar W, Gao Y, Scott M, Truesdell P, Greer PA . Fer-mediated cortactin phosphorylation is associated with efficient fibroblast migration and is dependent on reactive oxygen species generation during integrin-mediated cell adhesion. Mol Cell Biol 2007; 27: 6140–6152.
Kwok E, Everingham S, Zhang S, Greer PA, Allingham JS, Craig AW . FES kinase promotes mast cell recruitment to mammary tumors via the stem cell factor/KIT receptor signaling axis. Mol Cancer Res 2012; 10: 881–891.
Ahn J, Truesdell P, Meens J, Kadish C, Yang X, Boag AH et al. Fer protein-tyrosine kinase promotes lung adenocarcinoma cell invasion and tumor metastasis. Mol Cancer Res 2013; 11: 952–963.
Sangrar W, Shi C, Mullins G, LeBrun D, Ingalls B, Greer PA . Amplified Ras-MAPK signal states correlate with accelerated EGFR internalization, cytostasis and delayed HER2 tumor onset in Fer-deficient model systems. Oncogene 2015; 34: 4109–4117.
Rocha J, Zouanat FZ, Zoubeidi A, Hamel L, Benidir T, Scarlata E et al. The Fer tyrosine kinase acts as a downstream interleukin-6 effector of androgen receptor activation in prostate cancer. Mol Cell Endocrinol 2013; 381: 140–149.
Kawakami M, Morita S, Sunohara M, Amano Y, Ishikawa R, Watanabe K et al. FER overexpression is associated with poor postoperative prognosis and cancer-cell survival in non-small cell lung cancer. Int J Clin Exp Pathol 2013; 6: 598–612.
Lin X, Dean DA . Gene therapy for ALI/ARDS. Crit Care Clin 2011; 27: 705–718.
Machado-Aranda D, Adir Y, Young JL, Briva A, Budinger GR, Yeldandi AV et al. Gene transfer of the Na+,K+-ATPase beta1 subunit using electroporation increases lung liquid clearance. Am J Respir Crit Care Med 2005; 171: 204–211.
Machado-Aranda DA, Suresh MV, Yu B, Raghavendran K . Electroporation-mediated in vivo gene delivery of the Na(+)/K(+)-ATPase pump reduced lung injury in a mouse model of lung contusion. J Trauma Acute Care Surg 2012; 72: 32–39; discussion 9–40.
Weiss DJ . Delivery of gene transfer vectors to lung: obstacles and the role of adjunct techniques for airway administration. Mol Ther 2002; 6: 148–152.
Somiari S, Glasspool-Malone J, Drabick JJ, Gilbert RA, Heller R, Jaroszeski MJ et al. Theory and in vivo application of electroporative gene delivery. Mol Ther 2000; 2: 178–187.
Mir LM . Electroporation-based gene therapy: recent evolution in the mechanism description and technology developments. Methods Mol Biol 2014; 1121: 3–23.
Dean DA, Machado-Aranda D, Blair-Parks K, Yeldandi AV, Young JL . Electroporation as a method for high-level nonviral gene transfer to the lung. Gene Ther 2003; 10: 1608–1615.
Mutlu GM, Machado-Aranda D, Norton JE, Bellmeyer A, Urich D, Zhou R et al. Electroporation-mediated gene transfer of the Na+,K+ -ATPase rescues endotoxin-induced lung injury. Am J Respir Crit Care Med 2007; 176: 582–590.
Machado-Aranda DA, Suresh MV, Yu B, Raghavendran K . Electroporation-mediated in vivo gene delivery of the Na+/K+-ATPase pump reduced lung injury in a mouse model of lung contusion. J Trauma Acute Care Surg 2012; 72: 32–39; discussion 9–40.
Matute-Bello G, Downey G, Moore BB, Groshong SD, Matthay MA, Slutsky AS et al. An official American Thoracic Society workshop report: features and measurements of experimental acute lung injury in animals. Am J Respir Cell Mol Biol 2011; 44: 725–738.
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015; 372: 747–755.
Raghavendran K, Notter RH, Davidson BA, Helinski JD, Kunkel SL, Knight PR . Lung contusion: inflammatory mechanisms and interaction with other injuries. Shock 2009; 32: 122–130.
Zisman DA, Kunkel SL, Strieter RM, Tsai WC, Bucknell K, Wilkowski J et al. MCP-1 protects mice in lethal endotoxemia. J Clin Invest 1997; 99: 2832–2836.
Raghavendran K, Davidson BA, Mullan BA, Hutson AD, Russo TA, Manderscheid PA et al. Acid and particulate-induced aspiration lung injury in mice: importance of MCP-1. Am J Physiol Lung Cell Mol Physiol 2005; 289: L134–L143.
Suresh MV, Yu B, Machado-Aranda D, Bender MD, Ochoa-Frongia L, Helinski JD et al. Role of macrophage chemoattractant protein 1 in acute inflammation following lung contusion. Am J Respir Cell Mol Biol 2012; 46: 797–806.
Neumann E, Schaefer-Ridder M, Wang Y, Hofschneider PH . Gene transfer into mouse lyoma cells by electroporation in high electric fields. EMBO J 1982; 1: 841–845.
Emr BM, Roy S, Kollisch-Singule M, Gatto LA, Barravecchia M, Lin X et al. Electroporation-mediated gene delivery of Na+,K+ -ATPase, and ENaC subunits to the lung attenuates acute respiratory distress syndrome in a two-hit porcine model. Shock 2015; 43: 16–23.
Dean DA, Ramanathan T, Machado D, Sundararajan R . Electrical impedance spectroscopy study of biological tissues. J Electrostat 2008; 66: 165–177.
Calautti E, Cabodi S, Stein PL, Hatzfeld M, Kedersha N, Paolo Dotto G . Tyrosine phosphorylation and src family kinases control keratinocyte cell-cell adhesion. J Cell Biol 1998; 141: 1449–1465.
Kim L, Wong TW . Growth factor-dependent phosphorylation of the actin-binding protein cortactin is mediated by the cytoplasmic tyrosine kinase FER. J Biol Chem 1998; 273: 23542–23548.
Kim J, Ogata Y, Feldman RA . Fes tyrosine kinase promotes survival and terminal granulocyte differentiation of factor-dependent myeloid progenitors (32D) and activates lineage-specific transcription factors. J Biol Chem 2003; 278: 14978–14984.
Qi W, Ebbert KV, Craig AW, Greer PA, McCafferty DM . Absence of Fer protein tyrosine kinase exacerbates endotoxin induced intestinal epithelial barrier dysfunction in vivo. Gut 2005; 54: 1091–1097.
Oh MA, Choi S, Lee MJ, Choi MC, Lee SA, Ko W et al. Specific tyrosine phosphorylation of focal adhesion kinase mediated by Fer tyrosine kinase in suspended hepatocytes. Biochim Biophys Acta 2009; 1793: 781–791.
Putzke AP, Rothman JH . Repression of Wnt signaling by a Fer-type nonreceptor tyrosine kinase. Proc Natl Acad Sci USA 2010; 107: 16154–16159.
Khajah M, Andonegui G, Chan R, Craig AW, Greer PA, McCafferty DM . Fer kinase limits neutrophil chemotaxis toward end target chemoattractants. J Immunol 2013; 190: 2208–2216.
Craig AW, Greer PA . Fer kinase is required for sustained p38 kinase activation and maximal chemotaxis of activated mast cells. Mol Cell Biol 2002; 22: 6363–6374.
Xu G, Craig AW, Greer P, Miller M, Anastasiadis PZ, Lilien J et al. Continuous association of cadherin with beta-catenin requires the non-receptor tyrosine-kinase Fer. J Cell Sci 2004; 117 (Pt 15): 3207–3219.
McCafferty DM, Craig AW, Senis YA, Greer PA . Absence of Fer protein-tyrosine kinase exacerbates leukocyte recruitment in response to endotoxin. J Immunol 2002; 168: 4930–4935.
Zirngibl RA, Senis Y, Greer PA . Enhanced endotoxin sensitivity in fps/fes-null mice with minimal defects in hematopoietic homeostasis. Mol Cell Biol 2002; 22: 2472–2486.
Vacik J, Dean BS, Zimmer WE, Dean DA . Cell-specific nuclear import of plasmid DNA. Gene Ther 1999; 6: 1006–1014.
Young JL, Dean DA . Electroporation-mediated gene delivery. Adv Genet 2015; 89: 49–88.
Hoth JJ, Hudson WP, Brownlee NA, Yoza BK, Hiltbold EM, Meredith JW et al. Toll-like receptor 2 participates in the response to lung injury in a murine model of pulmonary contusion. Shock 2007; 28: 447–452.
Suresh MV, Yu B, Machado-Aranda D, Bender MD, Ochoa-Frongia L, Helinski JD et al. Role of macrophage chemoattractant protein-1 in acute inflammation after lung contusion. Am J Respir Cell Mol Biol 2012; 46: 797–806.
Hao QL, Heisterkamp N, Groffen J . Isolation and sequence analysis of a novel human tyrosine kinase gene. Mol Cell Biol 1989; 9: 1587–1593.
Taddonio MA, Dolgachev V, Bosmann M, Ward PA, Su G, Wang SC et al. Influence of lipopolysaccharide-binding protein on pulmonary inflammation in gram-negative pneumonia. Shock 2015; 43: 612–619.
Dolgachev VA, Yu B, Sun L, Shanley TP, Raghavendran K, Hemmila MR . Interleukin 10 overexpression alters survival in the setting of gram-negative pneumonia following lung contusion. Shock 2014; 41: 301–310.
Dolgachev V, Thomas M, Berlin A, Lukacs NW . Stem cell factor-mediated activation pathways promote murine eosinophil CCL6 production and survival. J Leukoc Biol 2007; 81: 1111–1119.
Dolgachev V, Farooqui MS, Kulaeva OI, Tainsky MA, Nagy B, Hanada K et al. De novo ceramide accumulation due to inhibition of its conversion to complex sphingolipids in apoptotic photosensitized cells. J Biol Chem 2004; 279: 23238–23249.
Ding L, Dolgachev V, Wu Z, Liu T, Nakashima T, Wu Z et al. Essential role of stem cell factor-c-Kit signalling pathway in bleomycin-induced pulmonary fibrosis. J Pathol 2013; 230: 205–214.
Acknowledgements
We gratefully acknowledge the support of National Institutes of Health-R01HL102013 (KR). We thank Dr. JE Wilkinson (Department of Pathology/ULAM, University of Michigan Medical School) for the help with lung tissue histology scorings. We also thank Ms. Lane Kelley McCandless for her contribution in revising this manuscript.
Author contributions
VAD, RHG, MVS, BT, NT and DMA conducted experiments and wrote the manuscript. DMA, MRH, KR contributed to conceptual design, interpretation of data and critical review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dolgachev, V., Goldberg, R., Suresh, M. et al. Electroporation-mediated delivery of the FER gene in the resolution of trauma-related fatal pneumonia. Gene Ther 23, 785–796 (2016). https://doi.org/10.1038/gt.2016.58
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2016.58
This article is cited by
-
Electroporation-mediated delivery of FER gene enhances innate immune response and improves survival in a murine model of pneumonia
Gene Therapy (2018)
-
The FER rs4957796 TT genotype is associated with unfavorable 90-day survival in Caucasian patients with severe ARDS due to pneumonia
Scientific Reports (2017)