Abstract
Purpose:
Genotype-driven research recruitment complicates traditional study roles and may leave those recruited worried about unwelcome surprises from their DNA. This study investigated the ways that individuals experience genotype-driven recruitment, and conceptualize their roles as research participants.
Methods:
Individual interviews were conducted with the participants of a genotype-driven study on cystic fibrosis. The eligibility criteria included the presence of one of two genetic variants. We interviewed 24 of these participants: 9 had cystic fibrosis and 15 had been selected from a biobank as “healthy volunteers.”
Results:
Participants with cystic fibrosis expressed no concerns about the eligibility criteria and saw themselves as part of a close-knit research community. However, biobank participants were unsure about why they had been selected and how they should think about themselves relative to the study. They sometimes reacted with anxiety to genetic information that they perceived to connect them with cystic fibrosis.
Conclusion:
Being recruited for a study on the basis of one’s genotype may raise uncertainties about the meaning and implications of the genotypic information. People without the disease under study may require especially clear and detailed explanations of what researchers already know about their genetic makeup, in terms of future risk for themselves or their children.
Genet Med 2012:14(12):983–989
Similar content being viewed by others
Introduction
Traditionally, clinical and observational research studies base eligibility criteria on phenotypic information. In studies with a case–control design, individuals who have the condition of interest are identified by phenotypic information as “cases,” and individuals who do not have the condition are recruited for purposes of comparison as “controls.” In contrast, studies that are “genotype-driven” start with genetic variants of interest and investigate whether those variants are associated with a phenotypic outcome such as a disease or other health-related condition. In genotype-driven studies, individuals who have the genetic variant of interest are recruited, but they may or may not have any phenotypic condition(s) suspected of being associated with that variant; indeed, a primary goal of the research may be to learn whether the potential gene–disease association is valid.1,2
Being recruited to participate in any study of a disease condition may be perplexing or even worrisome to individuals who do not have that condition.3 Genotype-driven recruitment adds complexity to this problem. Potential participants who have already been diagnosed with a known genetic condition often express enthusiasm for this kind of recruitment, as it generates hope for advances in treatment for their condition.4 However, “healthy volunteers” may be confused about why they were recruited and need more explanation about the purposes of the research. Thus, genotype-based recruitment complicates study roles which traditionally have been based on having or not having a particular disease or condition, and may leave many individuals uncertain and worried about unwelcome surprises from examination of their DNA.3,4,5
To investigate the ways that individuals experience genotype-driven recruitment and conceptualize their roles as research participants, we interviewed people with cystic fibrosis and “healthy volunteers” who participated in the same genotype-driven research study. Both groups were informed during the consent process that they had one of the two genetic variants under study (without specifying which of the two). Although they were given identical genetics-related information, in-depth interviews revealed that these two research populations, with very different personal and medical histories, experienced their research recruitment and participation in ways that diverged substantially.
Materials and Methods
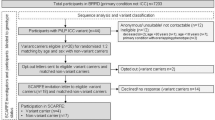
As part of a larger multisite study of genotype-driven research recruitment,6 interviews were conducted with individuals who participated in a genotype-driven study on cystic fibrosis (CF), specifically relating to the levels of the transforming growth factor β1 protein (TGFβ1) in the blood (hereafter referred to as the TGFβ1 study). Individuals were selected for the TGFβ1 study based on having particular genetic variants that had been shown to affect lung function in individuals with cystic fibrosis, and which were suspected to play a role in circulating blood levels of TGFβ1.7,8 The presence of these genetic variants was discovered through prior participation in genetic research ( Figure 1 ). Specifically, half of the TGFβ1 study participants, namely, the “CF participants,” had CF and had participated in an earlier study of genetic modifiers of CF, conducted by the same physician–researcher. The consent form for this earlier study had not mentioned the possibility that the subjects may be recontacted at a later date to participate in additional research.
The other half of the TGFβ1 participants, namely, the “biobank participants,” did not have CF, and were recruited from a biobank called the Environmental Polymorphisms Registry (EPR).9 The consent form for the EPR mentioned the possibility of recontact for additional studies as an integral component of initial participation: “… the DNA bank will be available to UNC [University of North Carolina] and NIEHS [National Institute of Environmental Health Sciences] researchers to look for certain differences in your DNA sequence. If one of these differences is found in your sample, a UNC or NIEHS scientist may contact you and ask you to participate in a future study of persons with the same DNA differences.”
Genotype-driven recruitment process for the TGFβ1 study
CF participants were recruited for the TGFβ1 study in person during a clinic visit. Biobank participants were recruited via a letter from the principal investigator that outlined the goals of the study and explained generally that recipients were being recruited because of a variant in their DNA (without specifying the variant). The letter also noted that having the variant of interest “does not mean you have a disease and there is no known relationship between the sequence you have in your DNA and any disease process.”
Identical consent forms were used for the CF participants and the biobank participants. The consent form noted that the purpose of the study was “to determine if there are differences in the levels of a substance called TGFβ1 in cystic fibrosis patients who have different degrees of disease compared to TGFβ1 levels in people who do not have cystic fibrosis.” The consent form briefly explained the significance of the TGFβ1 protein, and stated, “Previous studies have shown that in cystic fibrosis genotypes called CC and TT are related to different levels of TGFβ1 and how severe the disease is.” It then outlined the selection criteria for study participants ( Box 1 ), informing them that they were being asked to join a follow-up study based on information obtained about their DNA, and informing them of the categorical genetic inclusion criteria used in determining their eligibility, namely, the presence of either the CC or the TT genotype.
Interview methodology
Our interview study was determined exempt by the Institutional Review Board of the Duke University Health System, the institution at which the larger multi-site study of genotype-driven recruitment was based. The institutional review board at The University of North Carolina at Chapel Hill (the site responsible for recruiting the participants and conducting interviews) agreed to rely on the Duke University Health System Institutional Review Board’s decision.
As described elsewhere,4 all interviews were conducted in person at a location of the respondent’s choosing, with the exception of one telephone interview. All interviews were recorded; before the start of the interview, the respondents were asked to provide their verbal consent to participate. The interviewees were asked to recall their experiences of both the original study (either the CF genetic modifiers study or joining the EPR biobank) and the follow-up study (the TGFβ1 study), and to provide their opinions regarding the return of individual genetic research results to participants, in the context of being contacted for a genotype-driven follow-up study ( Box 2 ).
During the first several interviews it became clear that the participants did not usually recall that the consent form for the TGFβ1 study described the genetic inclusion criteria for the study, and many did not understand that they were being recruited for the TGFβ1 study because a previous study had identified a variant of interest in their genotype. Given that several of the interview questions related to the participants’ experiences and opinions with respect to genotype-driven recruitment, an addendum was added to the interview protocol in which interviewers showed participants a copy of the TGFβ1 study consent form, specifically highlighting the passage that explained the genetic basis for their recruitment. Interviewees who did not recall anything about these criteria were asked to read the relevant passage from the form, discuss their reactions to it, and revisit some of the earlier interview topics with this information in mind. After the interview ended, the interviewer endeavored to answer any questions the respondent had about information learned in the course of the interview, and offered information on how to contact the TGFβ1 study’s PI with any further questions.
Qualitative analysis
All the interviews were transcribed, and the transcripts were imported into NVivo qualitative data analysis software.10 Through a collaborative process with the other two sites in the multisite study,6 a standard codebook was created. Additional codes, specific to the UNC site’s study, were also developed. The first two authors coded all 24 transcripts using the codebook. The first three transcripts were coded by both coders, and any discrepancies were resolved by consensus.11 Two additional transcripts (for a total of 20 percent of all transcripts) were coded by both coders during the coding process and discrepancies resolved by consensus, in order to ensure they continued to code in the same manner as they proceeded through the rest of the transcripts.
The first two authors then read every UNC site transcript closely and met to discuss each case in detail. They analyzed responses to interview questions concerning participants’ understandings of the eligibility criteria for recruitment to the TGFβ1 study, and their experiences relating to joining and participating in the TGFβ1 study. In addition, they examined all segments of text in which a code called “informed participation” had been applied. This code was used whenever respondents discussed their understanding of what was involved in participating in either the original research (the CF genetic modifiers study or the EPR biobank) or the TGFβ1 follow-up study, and also why they were eligible for the TGFβ1 study. Finally, the first two authors examined all text from the interview addendum, in which some of the interviewees had been asked to read and respond to the genetic inclusion criteria in the follow-up study consent form. Using these data, they compiled response matrices to compare each participant’s statements concerning genotype-driven recruitment and their experiences of study participation. In the analysis, the participants were identified by study number; all personal names used for identification in the text of this article are pseudonyms.
Results
Study participants
We interviewed 9 CF participants and 15 biobank participants ( Table 1 ). All 24 interviewees self-reported as White and non-Hispanic, reflecting the racial and ethnic composition of the TGFβ1 study population. The respondents were generally well educated, particularly the biobank participants. Because the biobank’s original recruitment base included regional universities and research-related entities, several biobank participants had significant experience working in scientific research. Three of the biobank participants, but none of the CF participants, recalled (before being shown the consent form during the interview) that they received information about genetic inclusion criteria during their recruitment for the TGFβ1 study.
Understanding eligibility criteria
All the CF participants reported that they had been recruited frequently for studies because of their disease condition; in contrast, biobank participants’ recruitment to the TGFβ1 study was predicated only on a single previous biospecimen contribution to the EPR. The participants’ understandings about why they had been chosen for a follow-up study depended heavily on these two very different routes to eligibility.
Undergoing CF treatment at a major research center comes with many opportunities to participate in research. For most of the CF participants we interviewed, merely the fact that they had CF was a sufficient explanation for being recruited to the TGFβ1 study. Danny, a CF participant, did not recall why he was recruited for this particular study but said, “Typically, I just figure it’s because of cystic fibrosis.” A few CF participants already knew that their CF genotype was uncommon in some way, and assumed that this genotype was of particular interest to the researchers. One of these, Jodi, said that she had “one of the worst CF mutations,” but was remarkably healthy, which made her “kind of weird.” Another, Alex, noted that he was not surprised to be recruited for a study, because his unusual CF genotype made him “an atypical mutant.” Previous willingness to take part in research was also seen as a likely explanation for recruitment: Patti presumed that her frequent participation in other CF studies was an important factor, “because they know that I’m always going to say yes.” Patti was usually the first to be recruited for a study, she joked, “because I’m a research slut.”
Biobank participants attributed their recruitment to a variety of reasons. Some believed their selection from the biobank was “more or less random,” as Bob put it: “There wasn’t anything that I felt I was being singled out because of.” Others, including Lauren, guessed they were being matched on demographic characteristics: “Perhaps I just happened to fit into the age and the gender and the race and the body type that they needed.” Many, like Kenneth, remembered or suspected that researchers had looked at their blood or DNA and found “something of interest.” For Kenneth it seemed like fun to be a “guinea pig” for the follow-up study, although in the interview he wrestled briefly with how to describe himself. Asked to describe his feelings about being recruited for research based on his biobank contribution, Kenneth responded, “Glad to be of help. Just kind of fun to be, you know—oh, gosh, you know, a guinea pig.” This term, though used jokingly, may have reflected an underlying sense that his DNA was being used in ways he did not fully understand, and that were not likely to benefit him. Amanda recalled, “My impression was, everyone was contacted for the initial blood [biobank enrollment], and then it’s more like a subgroup that stands out from that.” What it might mean to be recruited for the TGFβ1 study as part of this “subgroup,” however, was less clear for Amanda: “Was there something bad, and that’s why you’re being contacted, or is it a good thing that you fell in that one group? So I thought, why not continue with it and find out?”
“We could cure CF”: CF participants’ perceptions of their research role
CF participants generally spoke about their roles in studies as usually involving giving biological samples, a frequent activity for them both as patients and as research participants. “Whenever they ask you for something they usually want blood work,” Henry noted. Amber did not mind being approached with an invitation to participate in a research study while she was at a clinical appointment. She said, “It’s a very convenient time to discuss medical-type things.” When Danny was asked whether he expected to be recruited for a follow-up study, he replied simply, “It’s never out of the question.” Henry mused, “you never know” when researchers will request participation in a follow-up study. “If they do, that’s fine. If they don’t, that’s fine.” It appeared that overlapping clinical and research contexts contributed to CF participants’ seemingly nonchalant reactions to being recruited for the TGFβ1 study.
Several CF participants explained that they were usually willing to participate in studies because they felt that they were contributing to a good cause—and they enjoyed receiving the small monetary compensation. Patti summed up her reaction to the follow-up contact as a “multiwin” situation:
“First of all, selfishly, I’m at clinic anyway. I get a little money. It’s nice just to have a little extra. It’s like finding some money on the road. … It increases knowledge of CF for the researchers to be used to find a cure. It was convenient. … I mean, how could you say no? It’s a little “stick,” [and] some questions.”
For Patti, as for most CF participants, the TGFβ1 study did not particularly stand out; it was one contact among many with the CF clinic—during which there was a possibility of receiving, along with their clinical treatment, “a little extra.” Because of the relationships that CF participants frequently form over years of interaction with physician–researchers, they often feel that they are part of a “team” that is working to help the CF community. “We need to let these old men in Chapel Hill retire!” Patti said, laughing. “Wouldn’t it be cool if we could cure CF? … And then they could just retire and enjoy life, knowing they did what they set out to do.”
Control, random, normal? Biobank participants’ perceptions of their research role
Not surprisingly, biobank participants did not share CF participants’ sense that they were part of a clinical/research community, although all of them stated they were glad to be of help to the follow-up study. Their understandings of their role in the TGFβ1 study ranged from being a fairly insignificant part of a large group to being a person with a uniquely helpful and interesting genetic variant. For example, Brent, recognizing researchers’ need for large sample sizes, saw himself as one among many who assisted in meeting that need: “The more samples you have, the higher the power; the higher the power, the more likely that what you find is true.” At the other end of the spectrum were biobank participants who understood that “they had identified something interesting and [wanted] to follow up on it,” as Steve put it. Another biobank participant, Scott, even found it “exciting” to hear that “I had something that somebody was interested in researching.” Remembering receiving his recruitment letter, Scott recalled it was “almost like I won the lottery.”
Whether they felt unique or incidental to the TGFβ1 study, however, biobank participants’ most common self-description was as a “control”—a concrete-sounding term that nevertheless meant very different things to different participants. To several, being a “control” meant that they were “normal” or “healthy.” Brent, who said that he had been recruited as part of the “normal individual cohort,” explained that, to him, this phrase meant: “You were randomly selected to be a participant of the normal because you didn’t fulfill any clinical criteria to make you part of a clinical treatment group.” Others, like Anne, presumed either that their selection from the biobank had been made at random, or that they were demographically or phenotypically matched with a CF participant. Anne surmised, “I probably mirrored people who have CF but [I] didn’t have it, and so I—that’s why they wanted to use a control.” In contrast, Steve expressed confusion as to his status in the study, because being a control meant to him that he did not have the genetic variant of interest: “Was I part of the control group, or did I have that particular trait? And I was curious, and it would have been interesting to know.” Kathryn, who had received CF carrier screening as part of her recent prenatal care, recalled of her recruitment letter, “I think it said I was a control who didn’t have the cystic fibrosis gene, and that was not a surprise to me because I already had been recently screened for that and knew.” For Kathryn, as for several biobank participants, having the genetic variant of interest for a cystic fibrosis study was equivalent to having “the cystic fibrosis gene”—either having the disease or being a carrier for the disease.
It was this association that primarily troubled the biobank participants who expressed concern about their recruitment for a CF study. Confident that she was a control without “the cystic fibrosis gene,” Kathryn was pleased to be recruited for the TGFβ1 study for both “the money and the chance to keep contributing to an ongoing research study.” Those who were not as sure about their status as participants, however, frequently noted that their recruitment caused some anxiety. For example, Brian’s reaction to his recruitment letter was mixed: he was “kind of excited” to be contacted, yet he was unsure of the implications. He called the phone number given in the letter, seeking more information about his selection. Although Brian did decide to participate, he did not feel fully reassured from speaking with study personnel on that call. He was particularly worried, he recalled, because he and his wife were planning to conceive, “and we had decided beforehand not to get amniocentesis or any genetic testing done on the fetus. So not having any genetic problems in her family or mine, I was wondering why they’d contacted me about cystic fibrosis.” Bill expressed similar concerns because of his infant daughter; he recalled being assured over the phone that his recruitment did not mean he was a carrier of cystic fibrosis, but this was only after reading the recruitment letter and “initially getting a little anxious.” Having already made their decision and participated in the TGFβ1 study, however, some biobank participants with anxieties downplayed their concerns during the interview, even as they were articulating them. James, for example, mentioned and then immediately dismissed his worries:
“Probably the title sort of surprised me, but then I don’t know whether I was the control or the subject group. So again that’s probably the only thing that was a little—I won’t say surprising, but unnerving, we’ll say. Not—it wasn’t super unnerving, it was just different. … So it just—again, it’s just an emotional thing. It’s not something.”
These self-understanding of one’s status as a research participant can also change over time; like Bill, several biobank participants who were initially troubled about their recruitment decided later that there was no cause for worry. On the other hand, some who were not initially worried found that anxieties developed later. Heather recalled feeling reassured after talking with a researcher; yet later she began to wonder “if there’s something freaky going on with my genes.” For a few, our interview questions about their participation raised some concerns. Julia, at the end of her interview, asked the interviewer to remind her of the specifics of the biobank and TGFβ1 study, wondering, “Was that a bigger deal than what I thought at the time?” Feeling reassured by the interviewer’s response, she decided, “I felt fine with it then. I feel fine with it now.”
Discussion
This study of two very different groups of participants in genotype-driven research brings to light the importance of the self-perceptions of research participants, a topic that has rarely been addressed but that may be particularly important in genotype-driven research that relies upon repeated participation of volunteer subjects. CF participants and biobank participants differed markedly, both in their understandings of why they were chosen for the TGFβ1 study and in their self-perceptions as participants in that study. CF participants, unlike biobank participants, were frequently asked to participate in research, often had long-standing relationships with the physician–researchers, and spoke of themselves as part of a research community with a clear goal. In contrast, biobank participants were usually less sure about why they had been selected and how they should think of themselves in relationship to the study.
These differences played into the divergent reactions of the two groups when they were recruited on the basis of information about their DNA. CF participants, whose condition was being managed by the same clinic that was conducting the research, often noted that new information offered the promise of even better care.4 However, some biobank participants reacted with anxiety to genetic information that connected them in some way with cystic fibrosis, even during our interview many months later. This finding underscores the concept that informed consent is not a one-time event; instead, it is an evolving process in which participants’ understanding of a study and of their own participation may change over time. Conley and colleagues describe this concept as the “discursive process” of informed consent.12 Our interview questions reminded some participants of concerns they had experienced during recruitment, and led others to reconsider whether they “should” have had concerns during recruitment. In response, several participants reassured themselves during the interview that their concerns were not serious and that they had indeed made the right decision.
Genotype-driven recruitment differs from traditional phenotype-driven recruitment in ways that may matter a great deal to participants. In the case of a condition like CF, the genetic basis for the disease is well-known, and many patients with CF have received their individual genetic results from clinical testing. CF patient–participants expressed no concerns about being recruited for further studies to investigate the genetic underpinnings of the disease. Indeed, research participation, for them, was seen as an important part of their membership in that disease community. Patients with CF differed from other populations in our multisite study (which also included adult patients with epilepsy and families of pediatric patients with autism or diabetes) in their attitudes toward genetic research and individual genetic research results.5,6,13 These differences, which probably at least partly reflect the particular experience of having CF rather than some other condition, indicate that further study should be carried out before generalizing from the experiences of this patient population.
On the other hand, people who do not have the disease under study may fear or suspect that being recruited for a genetics-related study about that disease has personal implications for them—or for their children. Unlike recruitment based on phenotypic traits, of which potential participants are likely to be aware, genotype-driven recruitment is premised on individual genetic information generated in the context of research; it is therefore highly unlikely that the person would have prior knowledge of this information. If this genetic information relates to a disease condition with which that person has not been diagnosed, then this new knowledge may raise a host of uncertainties about its possible meaning, in addition to personal doubts about that person’s connection to that condition. As previous research has pointed out, anxieties about what may be hidden in one’s genes may occur both for “healthy volunteers’’ in research and for people who have a disease condition, especially if little is known about the genetic basis of that condition.3,4,5 We note that, due to the design of the original studies, our interviewees were racially and ethnically homogeneous, and were very highly educated relative to the general US population. These characteristics, along with the small scale of this qualitative study, limit the extent to which its results may be generalized, and point to the need for further study of this topic.
On the basis of our data, we suggest that, if participants have a clear sense of their role in a study and why they have been recruited, they may have a more positive experience of participating in that study; this suggestion bears further investigation. In particular, people without the disease condition under study may look for reassurance that they are a “control” or a “healthy volunteer,” and for clear and detailed explanations of what researchers already know about the genetic variant they carry, in terms of future risk for themselves or their children. At the same time, it is important that the process of communicating this information be carefully designed so as to avoid disclosing genetic information to participants who do not want to be told. At the end of our multisite study, we convened a workshop with multiple stakeholders, including some study participants, to develop recommendations for ethical approaches to genotype-driven research recruitment. The recommendations of the workshop are currently under review for publication.
Our data demonstrate that people tend to use whatever scientific understandings they have in their effort to understand why they have been recruited for a study. Their understandings may include notions of “controls,” “blinded studies,” and “experimental designs,” among others. It would therefore be helpful for researchers to try to anticipate the ideas that different categories of prospective participants may hold, and to counter inaccurate conceptions about research participation. Indeed, although a genotype-driven study such as this one has some features of a case–control study, in other aspects it may be characterized as a study of four “exposure groups” (having the CC genotype, having the TT genotype, and either having or not having CF). As genotype-driven studies increase in number and importance, they are likely to challenge accepted ways of thinking about biomedical research, for both scientists and participants. Such studies tend to focus more on finding and understanding genetic variants and their interactions with population risk factors than on the detection, characterization, or treatment of a particular disease; consequently, the implications of having a particular genetic variant may not be clear for any given participant. The importance of considering research participants’ understandings and interpretations of the reasons for their eligibility will only grow as recruitment for biobanks and genomic research, particularly recruitment of “healthy volunteers” continues to increase.
Disclosure
The authors declare no conflict of interest.
References
Beskow LM, Linney KN, Radtke RA, Heinzen EL, Goldstein DB . Ethical challenges in genotype-driven research recruitment. Genome Res 2010;20:705–709.
McGuire SE, McGuire AL . Don’t throw the baby out with the bathwater: enabling a bottom-up approach in genome-wide association studies. Genome Res 2008;18:1683–1685.
Beskow LM, Dean E . Informed consent for biorepositories: assessing prospective participants’ understanding and opinions. Cancer Epidemiol Biomarkers Prev 2008;17:1440–1451.
Cadigan RJ, Michie M, Henderson G, Davis AM, Beskow LM . The meaning of genetic research results: reflections from individuals with and without a known genetic disorder. J Empir Res Hum Res Ethics 2011; 6:30–40.
Namey EE, Beskow LM . Epilepsy patient-participants and genetic research results as “answers”. J Empir Res Hum Res Ethics 2011;6:21–29.
Beskow LM, Namey EE, Cadigan RJ, et al. Research participants’ perspectives on genotype-driven research recruitment. J Empir Res Hum Res Ethics 2011;6:3–20.
Cutting GR . Modifier genes in Mendelian disorders: the example of cystic fibrosis. Ann N Y Acad Sci 2010;1214:57–69.
Drumm ML, Konstan MW, Schluchter MD, et al.; Gene Modifier Study Group. Genetic modifiers of lung disease in cystic fibrosis. N Engl J Med 2005;353:1443–1453.
Chulada PC, Vahdat HL, Sharp RR, et al. The Environmental Polymorphisms Registry: a DNA resource to study genetic susceptibility loci. Hum Genet 2008;123:207–214.
NVivo qualitative data analysis software [computer program]. Version 8: QSR International Pty Ltd.; 2008.
Miles MB, Huberman AM . Qualitative Data Analysis: An Expanded Sourcebook. Sage: Thousand Oaks, CA, 1994.
Conley J, Cadigan RJ, Davis AM, et al. The discourse of DNA: Giving informed consent to genetic research. In: Conley J, (ed). The Travels of Texts in Lay-Legal Communication. Oxford University Press: London, in press.
Tabor HK, Brazg T, Crouch J, et al. Parent perspectives on pediatric genetic research and implications for genotype-driven research recruitment. J Empir Res Hum Res Ethics 2011;6:41–52.
Acknowledgements
The project described was supported by Award Number RC1HG005787 from the National Human Genome Research Institute (NHGRI). Support was also provided by P50 HG004488 from the NHGRI. The content is solely the responsibility of the authors and does not necessarily represent the official views of NHGRI or the National Institutes of Health. We thank Patricia Chulada, health scientist administrator from the National Institute of Environmental Health Sciences, and Michael Knowles, professor of Pulmonary Medicine in the UNC Department of Medicine and the UNC Cystic Fibrosis Treatment and Research Center, for their invaluable help associated with the Environmental Polymorphisms Registry and the TGFβ1 study. Many thanks also to the CF and biobank participants who agreed to be interviewed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Michie, M., Cadigan, R., Henderson, G. et al. Am I a control?: Genotype-driven research recruitment and self-understandings of study participants. Genet Med 14, 983–989 (2012). https://doi.org/10.1038/gim.2012.88
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2012.88
Keywords
This article is cited by
-
Participant perspective on the recall-by-genotype research approach: a mixed-method embedded study with participants of the CHRIS study
European Journal of Human Genetics (2023)
-
Genotype-driven recruitment: a strategy whose time has come?
BMC Medical Genomics (2013)