Abstract
Purpose
To assess the occurrence rate of retinal detachment (RD) after small gauge vitrectomy for idiopathic epiretinal membrane (ERM).
Patients and methods
Retrospective observational case series. The records of consecutive patients operated on for idiopathic ERM using small gauge pars plana vitrectomy between August 2012 and December 2014 with at least a 1-year follow-up were reviewed. All patients were contacted by phone to assess the occurrence of RD during the post-operative follow-up. The main outcome was the occurrence of RD. Patients who underwent surgery for senile cataract over the same period with at least a 1-year follow-up were also contacted by phone for comparison.
Results
Two hundred and sixteen eyes of 212 patients who had undergone ERM surgery were included, with a mean follow-up of 892±211 days (216–1238). RD occurred in two eyes (0.92%). Over the same period, two RD occurred in the 203 eyes (0.98%) of 157 patients operated on for senile cataract in our department.
Conclusions
The occurrence of RD after 25-gauge vitrectomy for idiopathic ERM was <1%. Using small gauge sutureless vitrectomy systems has improved the safety of ERM surgery, with a RD rate similar to that observed after cataract surgery.
Similar content being viewed by others
Introduction
Idiopathic epiretinal membrane (ERM) is the leading surgical complication of macular diseases in the elderly, with a prevalence between 28 and 53% from 63 to 85 years old.1 The contraction of the ERM at the inner retina surface is responsible for visual dysfunction.2 In clinical practice, the decision to perform surgery is usually driven by the level of visual acuity (VA) and the presence of metamorphopsia.3 The surgical management of ERM consists in performing vitrectomy and ERM peeling,4 providing a VA gain and decreasing metamorphopsia in most cases.5 The visual outcome is mainly related to the preoperative VA, suggesting that operating patients earlier would allow a better visual rehabilitation. Nevertheless, a score <20/50 Snellen is usually recommended,5, 6 as the benefit of surgery is mainly balanced by the threat of retinal detachment (RD) occurring after vitrectomy. RD is reported in 3% of cases operated on using 20-gauge vitrectomy for ERM.7, 8 Over the years, the improvement in vitrectomy systems has allowed developing a painless, time-saving surgical procedure and achieving a faster VA recovery.9 They have also helped to reduce the occurrence of RD after ERM surgery.7, 8, 10 The aim of this study was to assess the occurrence rate of RD after 25-gauge pars plana vitrectomy for idiopathic ERM. Meanwhile, we assessed the occurrence rate of RD after cataract surgery performed in our department over the study period for comparison.
Subjects and methods
The records of patients operated on for ERM in the department of Ophthalmology of Lariboisière Hospital between August 2012 and December 2014 were retrospectively reviewed. The inclusion period matched the systematic use of 25-gauge system for vitreoretinal procedures in our department. The study conduct complied with the tenets of the Declaration of Helsinki. The Ethics Committee of the French Society of Ophthalmology (IRB 00008855 Société Française d’Ophtalmologie IRB#1) approved this retrospective review of patient records. Patient consent was obtained. Patients operated on for idiopathic ERM or ERM secondary to peripheral break with at least a 1-year post-operative follow-up were included. Patients with secondary ERM such as macular pucker after RD, uveitis, high myopia, diabetic retinopathy, or another ischaemic retinopathy were excluded.
The surgical technique for ERM management was a 25-gauge transconjunctival pars plana vitrectomy. All the surgeons of the department performed the vitrectomy using a similar technique. Constellation Vision system with a 25+ Ultravit high-speed vitrectomy probe (Alcon, Fort Worth, TX, USA) was used, with 5000 cuts per minute and a maximal aspiration rate of 450 mm Hg. The 25-gauge trocars were introduced at 3.5 or 4 mm from the limbus with a 45° oblique tunnel-shaped incision into the sclera. Core vitrectomy was performed. When the posterior vitreous cortex was still attached to the optic disc or to the retina, its detachment was induced by applying a strong aspiration with the vitrectomy probe in front of the optic disc. The ERM was peeled after a 1-min staining with Membrane-Blue Dual (DORC, Zuidland, Netherlands) using a 25-gauge+ Grieshaber endgrasping forceps (Alcon Grieshaber AG, Scaffhausen, Switzerland). Integrity of the whole peripheral retina was verified by a careful examination under scleral indentation. When a retinal break was observed, it was treated either with cryotherapy or endolaser photocoagulation. Peripheral vitrectomy under scleral indentation was performed if tamponade was decided. Ablation of the trocars was then performed. Unclosed sclerotomies were closed using 8.0 absorbable sutures. A post-operative follow-up examination was performed at day 1, 7, and 1 month. Combined cataract surgery was performed when lens opacification was considered impairing VA or intraoperative visibility.
The records of patients operated on for cataract in the department with at least a 1-year follow-up were also reviewed. All situations that led to early onset of lens opacification were excluded: diabetic and other metabolic cataracts, congenital cataract, glucocorticoid-induced cataract, post-uveitis, high myopia, and post-vitrectomy cataract. Phacoemulsification surgery was standardised for all patients with a 2.4-mm clear corneal incision, bimanual surgery, and intra-camerular injection of 0.5 mg of cefuroxime (Aprokam) at the end of surgery. Follow-up examinations were performed on the same day as the surgery and at 1 month. All patients were given post-operative instructions to consult in emergency in case of pain, redness, floaters, phosphenes, visual field amputation, or vision loss.
The main outcome was the occurrence of a post-operative RD. This information was collected by two means: the occurrence of RD was reported in patient record or the patient was contacted by phone and questioned regarding the following: (1) the need for re-operation, (2) the result of the last post-operative control, (3) his feeling about his current vision. If the answers were directed towards re-intervention or vision loss, the question ‘Did you experience a retinal detachment?’ was explicitly raised. If the patient had not been re-operated, the post-operative control was unremarkable or the patient was satisfied with his vision, it was considered that the patient did not experience a RD. Patients who could not be contacted by phone were excluded as the main outcome data were missing. In cases with RD, the time to occurrence after the first surgery was noted. The following data were also recovered from patient records and surgery reports: age, gender, preexisting posterior vitreous detachment (PVD) or its induction during vitrectomy, occurrence of intraoperative complications, including capsular rupture or retinal breaks and YAG capsulotomy.
Statistical analysis was performed using NCSS software (East Kaysville, UT, USA). Descriptive statistics and non-parametric Mann–Whitney U-tests were used to compare patient characteristics. A relative risk was calculated for the correlation between RD, intraoperative induction of PVD, and intraoperative retinal breaks. A Kaplan–Meier curve was used to illustrate the occurrence of RD during the follow-up.
Results
The records of 353 patients operated on for ERM were reviewed. Eighty patients were excluded because of secondary ERM and 61 patients were lost to follow-up. A flow chart illustrates patient inclusion in Figure 1. Two hundred and sixteen eyes of 212 patients who had undergone idiopathic ERM peeling and 203 eyes of 157 patients who had undergone cataract surgery were finally included. Patient characteristics are presented in Table 1.
PVD was complete in 164 eyes (77.3%) and was induced during surgery in 49 eyes (22.6%). Retinal breaks occurred during surgery in 18 eyes (8.3%) but no intraoperatively induced PVD resulted in a post-operative RD. Intraoperative retinal breaks were treated intraoperatively with endolaser photocoagulation (11/18 eyes) or cryotherapy (7/18 eyes). A RD occurred in two eyes (0.92%). The intraoperative induction of PVD was not associated with the occurrence of retinal break (RR=0.94) but was associated with the occurrence of RD (RR=3.33).
Three hundred and sixty-eight cataract surgery procedures performed over the same period were reviewed, 97 were excluded because of secondary cataract and 68 patients were lost to follow-up (Figure 1). Patient characteristics are presented in Table 1. RD occurred in two cases (0.98%). The occurrence of RD during the follow-up is illustrated by a Kaplan–Meier survival curve in Figure 2. The characteristics of patients who experienced a RD are detailed in Table 2.
In the ERM group, RD occurred in two male patients, respectively, 8 days and 5 weeks after vitrectomy. One had a preexisting PVD and in the other patient, PVD was induced intraoperatively. None of them presented intraoperative retinal breaks. One had undergone combined surgery and the other was phakic. After cataract surgery, RD also occurred in two male patients, respectively, 12 and 18 months after an uncomplicated procedure. None of these patients presented posterior capsular opening during surgery and neither had undergone YAG capsulotomy after surgery.
Discussion
The recent improvements in vitrectomy systems have helped to reduce the occurrence of RD after vitrectomy for ERM from about 3% using 20-gauge vitrectomy7, 8 to about 1% using the 25-gauge systems.10, 11 In our series of 216 eyes operated on for idiopathic ERM using 25-gauge vitrectomy with the latest improvements and followed for at least 1 year, the occurrence rate of RD was even lower, at 0.92%, and decreased compared to a formerly published series from our department in which a 20-gauge system was used.7 We focused on idiopathic ERM because, for various reasons, the rate of RD is very different and much higher in secondary ERM (about 7%) than in idiopathic ERM.4, 12
RD is an important element in the risk/benefit ratio of ERM surgery. Regarding the two other main complications, endophthalmitis is rare and cataract is considered an earlier appearance of an inevitable surgery.13, 14 The occurrence of RD after vitrectomy is due to intraoperative or post-operative retinal breaks. Intraoperative retinal breaks may result from different mechanisms: traction over the vitreous base during the insertion of instruments, incarceration of the vitreous fibres in an open sclerotomy, or brutal aspiration during shaving. According to Tan et al,15 the first two mechanisms result in sclerotomy-related retinal breaks. In their study, using trocars protected the vitreous base during instrument insertion compared to 20-gauge trocar-less vitrectomy. In addition, using a cannulated system helped to reduce the occurrence of intraoperative retinal breaks, from 17.4% using a 20-gauge system to 5.1% using a cannulated 25-gauge system.15, 16 Nowadays, surgeons also limit instrument inputs and outputs as much as possible. Using valves on trocars also limits intraoperative incarcerations. Vitrectomy fluidics is still improving with higher cutting rates and lower flow surges due to smaller gauges, acting as a passive flow control. A better surgical setting has enhanced flow stability and minimised vitreous turbulences, especially when the vitrectomy probe passes from the vitreous to the balanced salt solution or a dense vitreous base.17 All together miniaturising and improving vitrectomy systems reduce retinal traction and thereby the risk of iatrogenic retinal breaks.18, 19 In this study, using a 25-gauge system, we found a rate of 8.3% of intraoperative retinal breaks at the end of vitrectomy that could be even overestimated, as any suspicious appearance was considered as an opening and treated. Any preexisting opening discovered during the surgery was also treated to limit post-operative RD risks. More recently, a 27-gauge vitrectomy system with a higher cutting rate (up to 7500 cuts per minute) has shown its feasibility and safety, and has also been used in ERM surgery.20 However, the rate of iatrogenic retinal breaks using the 27-gauge system (9.6%) was similar to the rate reported after 25-gauge vitrectomy in our study as well as in others (Mura: 1.8%, Chung: 6.9%, and Tan: 13.9%).10, 16, 21
Most ERM are associated with a preexisting PVD. In our series, PVD was complete in 78% of eyes with idiopathic ERM, in accordance with the published series of ERM.22 However, another mechanism of intraoperative retinal breaks is the intraoperative induction of PVD.10, 16 Sandali et al23 have shown that retinal breaks were significantly associated with the induction of PVD, regardless of the system miniaturisation. In one of the two cases of RD appeared after ERM surgery, a PVD was initially absent and induced intraoperatively. No retinal tear was found in this case: the opening could have been missed or a new retinal break could have appeared postoperatively.
Intraoperative retinal breaks may be detected by a careful examination of the peripheral retina under scleral depression at the end of surgery.10, 15 The upgrade of microscope definition, endo-illumination quality, and visualisation systems has increased the quality of intraoperative visualisation and therefore the detection of peripheral retinal breaks. However, even with these improvements, a retinal break may be missed during the careful examination of the peripheral retina or appear after the control. The small size of trocars does not completely prevent from vitreous incarceration that may lead to retinal tears during or even a long time after surgery. Indeed, retinal breaks may in theory also result from changes and contraction of the remaining vitreous and the vitreous base with a vitreous incarceration. Finally in our series, vitrectomy was usually limited to core vitrectomy. The positive or negative effect of extensive vitrectomy on RD rate remains controversial.24
We also assessed the rate of RD occurring after cataract surgery in our department over the same period, as it is the most common surgical procedure performed in patients of same age. While the risk of RD is usually not enough emphasised when informing the patient on the risks of cataract surgery, this risk was similar to the risk of RD after vitrectomy. The rate of RD observed after cataract surgery in this series was of 0.98% with at least a 1-year follow-up. This rate in the cataract group is consistent with the incidence rate of RD of 0.9% reported in larger series of patients with a longer follow-up of 4 years.25 It should be noted that the overall incidence of RD around the age of 70 is much lower, varying from 0.01 to 0.05% per year.26 After cataract surgery, the risk of RD increases in a nearly linear manner over time, pointing out its relationship with the onset of PVD and also explaining why the rate of RD after cataract surgery has not changed despite the improvement in phacoemulsification technique. Cataract surgery indeed seems to accelerate PVD onset as it occurred in 30–78% of cases after a 3-year follow-up and was associated with retinal breaks in 6% of eyes in previous studies.27, 28
The rate of RD after vitrectomy for idiopathic ERM was not higher than that observed after cataract surgery and could not explain the difference in patient information or consideration in the risk/benefit ratio calculation. However, this is not only due to historically higher levels of RD after vitrectomy but also to the time to RD occurrence. Indeed, the early occurrence of RD after vitrectomy explains that RD has always been easily attributed to ERM surgery. In our series, RD occurred 8 days and 5 weeks after surgery, as the time to occurrence reported in other studies.11 This short time to onset also suggests that the first weeks and months of follow-up are more critical regarding the risk of RD after ERM surgery. In contrast, as it depends on PVD onset, the occurrence of RD after cataract surgery varies widely among reported series, from 1 month to 50 months.25, 28 The time to occurrence was of 12 and 18 months in our series. This late occurrence may lead to underestimation of this complication in cataract surgery.
Our study has some limitations, including its retrospective design. The sample size of 200 patients who had undergone vitrectomy for idiopathic ERM is significant, but remains small considering the low incidence of RD. Still, our results are consistent with the recent literature and our patients were followed for more than 1 year. Moreover, our study was conducted in a single centre where this surgical procedure is standardised and very similar from one surgeon to another, removing the bias related to an interindividual variation. We considered important to report the rate of RD after 25-gauge vitrectomy using modern systems for ERM to update patient information. We did not aim to directly compare the RD rate after vitrectomy for ERM and after cataract surgery, as patients were not matched. However, the rate of RD after cataract surgery, the most commonly performed eye surgery, in the same surgical setting and measured using the same methodology, keeps the rate of RD after vitrectomy in perspective.
In summary, the rate of RD occurring after 25-gauge vitrectomy for idiopathic ERM was <1%, similar to that observed after cataract surgery. It is of value for reassuring patients on the fact that undergoing vitrectomy for ERM is nowadays as safe as undergoing cataract surgery. This is also important to properly assess the risk/benefit ratio of ERM surgery in patients complaining about, although moderate, visual loss.

References
Meuer SM, Myers CE, Klein BEK, Swift MK, Huang Y, Gangaputra S et al. The epidemiology of vitreoretinal interface abnormalities as detected by spectral-domain optical coherence tomography: the beaver dam eye study. Ophthalmology 2015; 122: 787–795.
Fraser-Bell S, Guzowski M, Rochtchina E, Wang JJ, Mitchell P . Five-year cumulative incidence and progression of epiretinal membranes: the Blue Mountains Eye Study. Ophthalmology 2003; 110: 34–40.
Okamoto F, Okamoto Y, Hiraoka T, Oshika T . Effect of vitrectomy for epiretinal membrane on visual function and vision-related quality of life. Am J Ophthalmol 2009; 147 (5): 869–874 874.e1.
Margherio RR, Cox MS, Trese MT, Murphy PL, Johnson J, Minor LA . Removal of epimacular membranes. Ophthalmology 1985; 92: 1075–1083.
Song SJ, Kuriyan AE, Smiddy WE . Results and prognostic factors for visual improvement after pars plana vitrectomy for idiopathic epiretinal membrane. Retina 2015; 35: 866–872.
Dawson SR, Shunmugam M, Williamson TH . Visual acuity outcomes following surgery for idiopathic epiretinal membrane: an analysis of data from 2001 to 2011. Eye 2014; 28: 219–224.
Gaudric A, Cohen D . Surgery of idiopathic epimacular membranes. Prognostic factors. J Fr Ophtalmol 1992; 15: 657–668.
Guillaubey A, Malvitte L, Lafontaine PO, Hubert I, Bron A, Berrod JP et al. Incidence of retinal detachment after macular surgery: a retrospective study of 634 cases. Br J Ophthalmol 2007; 91: 1327–1330.
Kadonosono K, Yamakawa T, Uchio E, Yanagi Y, Tamaki Y, Araie M et al. Comparison of visual function after epiretinal membrane removal by 20-gauge and 25-gauge vitrectomy. Am J Ophthalmol 2006; 142: 513–515.
Mura M, Barca F, Dell’Omo R, Nasini F, Peiretti E . Iatrogenic retinal breaks in ultrahigh-speed 25-gauge vitrectomy: a prospective study of elective cases. Br J Ophthalmol 2016; 100 (10): 1383–1387.
Rizzo S, Belting C, Genovesi-Ebert F, Di Bartolo E . Incidence of retinal detachment after small-incision, sutureless pars plana vitrectomy compared with conventional 20-gauge vitrectomy in macular hole and epiretinal membrane surgery. Retina 2010; 30: 1065–1071.
Council MD, Shah GK, Lee HC, Sharma S . Visual outcomes and complications of epiretinal membrane removal secondary to rhegmatogenous retinal detachment. Ophthalmology 2005; 112: 1218–1221.
Jackson TL, Donachie PHJ, Sparrow JM, Johnston RL . United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: report 1; case mix, complications, and cataract. Eye 2013; 27: 644–651.
Dave VP, Pathengay A, Schwartz SG, Flynn HW Jr . Endophthalmitis following pars plana vitrectomy: a literature review of incidence, causative organisms, and treatment outcomes. Clin Ophthalmol 2014; 8: 2183–2188.
Tan HS, Lesnik Oberstein SY, Mura M, De Smet MD . Enhanced internal search for iatrogenic retinal breaks in 20-gauge macular surgery. Br J Ophthalmol 2010; 94: 1490–1492.
Tan HS, Mura M, De Smet MD . Iatrogenic retinal breaks in 25-gauge macular surgery. Am J Ophthalmol 2009; 148: 427–430.
Abulon DJ . Vitreous flow rates through dual pneumatic cutters: effects of duty cycle and cut rate. Clin Ophthalmol 2015; 9: 253–261.
Rizzo S, Genovesi-Ebert F, Belting C . Comparative study between a standard 25-gauge vitrectomy system and a new ultrahigh-speed 25-gauge system with duty cycle control in the treatment of various vitreoretinal diseases. Retina 2011; 31: 2007–2013.
Teixeira A, Chong LP, Matsuoka N, Arana L, Kerns R, Bhadri P et al. Vitreoretinal traction created by conventional cutters during vitrectomy. Ophthalmology 2010; 117: 1387–92.e2.
Oshima Y, Wakabayashi T, Sato T, Ohji M, Tano Y . A 27-gauge instrument system for transconjunctival sutureless microincision vitrectomy surgery. Ophthalmology 2010; 117: 93–102.e2.
Chung SE, Kim K-H, Kang SW . Retinal breaks associated with the induction of posterior vitreous detachment. Am J Ophthalmol 2009; 147: 1012–1016.
Wiznia RA . Posterior vitreous detachment and idiopathic preretinal macular gliosis. Am J Ophthalmol 1986; 102: 196–198.
Sandali O, El Sanharawi M, Lecuen N, Barale PO, Bonnel S, Basli E et al. 25-, 23-, and 20-gauge vitrectomy in epiretinal membrane surgery: a comparative study of 553 cases. Graefes Arch Clin Exp Ophthalmol 2011; 249: 1811–1819.
Ibarra MS, Hermel M, Prenner JL, Hassan TS . Longer-term outcomes of transconjunctival sutureless 25-gauge vitrectomy. Am J Ophthalmol 2005; 139: 831–836.
Daien V, Le Pape A, Heve D, Carriere I, Villain M . Incidence, risk factors, and impact of age on retinal detachment after cataract surgery in France: a National Population Study. Ophthalmology 2015; 122 (11): 2179–2185.
Mitry D, Charteris DG, Fleck BW, Campbell H, Singh J . The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol 2010; 94: 678–684.
Hikichi T . Time course of development of posterior vitreous detachments after phacoemulsification surgery. Ophthalmology 2012; 119: 2102–2107.
Ripandelli G, Coppé AM, Parisi V, Olzi D, Scassa C, Chiaravalloti A et al. Posterior vitreous detachment and retinal detachment after cataract surgery. Ophthalmology 2007; 114: 692–697.
Acknowledgements
The Department of Ophthalmology of Lariboisière Hospital received an independent research grant from Novartis Pharma SAS.
Author contributions
JM-L, AD, and RT: design and conduct of the study. JM-L: data collection. EP, AD, and BD: data analysis and interpretation. JM-L, EP: writing of the manuscript. JM-L, EP, RT, and BD: critical review and final approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
EP: Novartis, Bayer, Allergan (travel expenses). RT: board membership (Alcon, Novartis, Allergan, Bausch&Lomb, Pfizer, Alimera, Bayer, FCI-Zeiss, Thrombogenics), consultancy (Alcon, Novartis, Allergan, Bausch&Lomb, Dorc, Takeda, FCI-zeiss, Thrombogenics). BD: consultancy (Novartis, Bayer), board membership (Novartis, Allergan). The remaining authors declare no conflict of interest.
Additional information
Meeting presentation: Poster 1102-A0273, Association for Research in Vision and Ophthalmology, Annual meeting 2016, Seattle, WA, USA.
Rights and permissions
About this article
Cite this article
Marie-Louise, J., Philippakis, E., Darugar, A. et al. Occurrence rate of retinal detachment after small gauge vitrectomy for idiopathic epiretinal membrane. Eye 31, 1259–1265 (2017). https://doi.org/10.1038/eye.2017.79
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.79
This article is cited by
-
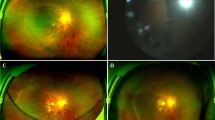
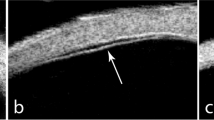
Accuracy of biomicroscopy, ultrasonography and spectral-domain OCT in detection of complete posterior vitreous detachment
BMC Ophthalmology (2023)
-
Prevalence and predictive factors for posterior vitreous attachment in eyes undergoing epiretinal membrane surgery
Eye (2022)
-
Characteristics of secondary epiretinal membrane due to peripheral break
Scientific Reports (2020)
-
The outcomes of subtotal vitrectomy in macular surgeries: a single surgeon case series
International Ophthalmology (2019)