Abstract
Objective
Elevated intraocular pressure (IOP) contributes to the progression of visual defects such as glaucoma. This study determined whether metabolic syndrome (MetS) and cardiovascular risk factors are associated with IOP in South Korean men.
Methods
We analyzed data on 4875 men who participated in the Korean National Health and Nutrition Examination Survey 2008–2010. We recorded the values for age, weight, height, body mass index (BMI), waist circumference (WC), systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose (FBG), insulin, homeostasis model assessment of estimated insulin resistance (HOMA-IR), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), non-HDL-C (NHDL-C), and TG/HDL-C, as well as sociodemographic factors. IOP was measured using Goldmann applanation tonometry.
Results
Weight, BMI, WC, SBP, DBP, FBG, insulin, HOMA-IR, TC, LDL-C, TG, NHDL-C, TG/HDL-C, and the prevalence of MetS differed significantly among the three groups with IOP (P<0.05). Mean IOP was higher in subjects who were obese and had hypertension, diabetes mellitus, MetS, abdominal obesity, high TG, high FBG, or high BP compared with normal subjects (P<0.005). Analysis using Pearson’s correlation coefficient showed that all cardiometabolic risk factors were significantly associated with IOP (P<0.005), with the exception of WC and HDL-C. A multivariate linear regression analysis showed that IOP was positively correlated with BMI, SBP, DBP, FBG, HOMA-IR, TC, LDL-C, TG, NHDL-C, and TG/HDL-C after adjusting for all covariates (all P<0.05).
Conclusions
Cardiometabolic risk factors, including the components of MetS, are associated with increased IOP.
Similar content being viewed by others
Introduction
Glaucoma is an ophthalmological disease characterized by optic nerve injury, which can result in loss of vision.1 The well-known risk factors for glaucoma include African ethnicity, family history of glaucoma, severe myopia, and high intraocular pressure (IOP).1, 2 Of these risk factors, high IOP is one of the strongest risk factors for glaucoma, and therefore, reducing IOP may delay the development of primary open-angle glaucoma.3, 4
Metabolic syndrome (MetS) is a collection of risk factors that increases the chance of an individual developing cardiovascular disease and diabetes mellitus (DM).5, 6 Insulin resistance is an original conceptualization of MetS and is a risk factor for the development of metabolic abnormalities, such as hypertension (HTN), obesity, impaired glucose tolerance, dyslipidemia, elevated triglyceride (TG) and low high-density lipoprotein cholesterol (HDL-C).7, 8 These metabolic abnormalities are also components of MetS as defined in the Adult treatment panel (ATP) III guidelines of the 2001 National Cholesterol Education Program (NCEP) and 2005 American Heart Association/National Heart Lung and Blood Institute (AHA/NHLBI) guidelines.9, 10 MetS affects a large number of people worldwide, and the global prevalence of MetS has increased over the recent years.11 In particular, the prevalence of MetS has been increasing in South Korean men. In 1998, 13.7% of South Korean men had MetS, but by 2005, this proportion had increased to 32.9% according to the 2005 Korea National Health and Nutrition Examination Survey (KNHANES).12
Many cross-sectional and longitudinal studies have identified a relationship between cardiometabolic risk factors and IOP. Studies based on Caucasian populations13, 14 and Asian populations15, 16, 17 have found that high IOP was associated with cardiometabolic risk factors including MetS. Some Korean studies have also found a positive relationship between IOP and cardiometabolic risk factors, including waist circumference (WC), body mass index (BMI), fasting blood glucose (FBG), and blood pressure.18, 19 However, there are some controversies surrounding these associations, and so far, no study has been performed on the entire Korean male population. The aforementioned recent Korean studies were only performed in postmenopausal women and some community populations who underwent general health examinations at rural health promotion centers.18, 19, 20 Therefore, we aimed to examine the relationship between IOP and cardiovascular risk factors, including MetS, in the entire population of Korean men who participated in the KNHANES.
Materials and methods
Study population
We enrolled men aged 20 or older whose IOP was measured in the KNHANES (the target population of which was all households and people across Korea). The study period of KNHANES was between 2008 and 2010. Exclusion criteria in this study were: the presence of thyroid disease, gastric cancer, hepatocellular cancer, colorectal cancer, breast cancer, lung cancer, chronic hepatitis B and C or liver cirrhosis; fasting for less than 8 h prior to blood sampling; renal failure; pulmonary or extrapulmonary tuberculosis; no data for the majority of past history; currently taking pharmacological treatments for HTN, diabetes, or dyslipidemia; ophthalmological diseases such as pterygium or strabismus; and currently being treated for glaucoma. In total, 4875 men were enrolled in the study.
Measurements
KNHANES is a nationwide cross-sectional survey conducted in Korea that uses stratified, multi-stage, clustered probability sampling to select a representative sample of the non-institutionalized civilian population of Korea. The survey consists of a health interview and a health examination. The survey collects data via face-to-face interviews in households and by direct standardized physical examinations conducted in specially equipped mobile examination centers.
Systolic blood pressure (SBP) and diastolic blood pressure (DBP) for each participant was measured three times at 5-min intervals using a standard mercury sphygmomanometer (Baumanometer, WA Baum Co. Inc., Copiague, NY, USA). The average of the second and third measurements was recorded as the final blood pressure measurement. Anthropometric data, including height, body weight, and WC were measured according to the standardized guidelines. Height (cm) was measured using mobile anthropometers (SECA 225, SECA Deutschland, Hamburg, Germany) with subjects in a standing position and the head and hips touching a wall. Body weight (kg) was measured using mobile scales (GL-6000-20, CASKOREA, Seoul, Korea) with the subject dressed in a light gown without shoes. Using a fiberglass tape measure (SECA 200, SECA Deutschland), WC was measured to the nearest tenth of a centimeter without compression of the soft tissue, along the middle horizontal line between the inferior margin of the last rib and the iliac crest. BMI was calculated by dividing body weight by height squared (kg/m2). FBG, TC, low-density lipoprotein cholesterol (LDL-C), HDL-C, and TG were measured using an autoanalyzer (ADVIA 1650, Bayer, Tarrytown, NY, USA) after a fasting period of at least 8 h. The coefficient of variation of the assays for insulin was 1.2%. Insulin resistance was calculated using the HOMA-IR using the following formula: fasting insulin (μU/ml) × fasting glucose (mg/dl)/405.21
Subjects were divided into three groups according to the smoking status; (1) non-smokers: those who never smoked or had smoked <100 cigarettes in their whole life, (2) ex-smokers: those who had smoked in the past but had stopped smoking, and (3) current smokers: those who were currently smoking and had smoked ≥100 cigarettes in their whole life. Subjects who drank <3 glasses a day (15∼30 g/day) were classified as mild to moderate drinkers, and subjects who drank ≥3 glasses a day (≥30 g/day) were classified as heavy drinkers. Physical activity was defined using the international physical activity questionnaire (IPAQ).22 Subjects were divided into three physical activity groups according to IPAQ criteria; sedentary (<600 metabolic equivalents (METs)/week), minimally active (600–3000 METs/week), and health-enhancing physical activity (>3000 METs/week).
Ophthalmological examinations were done using a slit-lamp (Haag-Streit model BQ-900; Haag-Streit AG, Koeniz, Switzerland) and performed by the study ophthalmologists. IOP was measured with a Goldmann applanation tonometer, and we used the mean value of two IOPs in our calculations. We divided subjects into three groups according to their IOPs: Tertile 1 (IOP<12.5 mm Hg), Tertile 2 (12.5≤IOP≤15.0 mm Hg), and Tertile 3 (15.0 mm Hg<IOP).
The Korean Ministry of Health and Welfare approved the study protocol and it is approved by the institutional review board of the Korean Center for Disease Control and Prevention. All subjects provided a written informed consent.
Definition of MetS
MetS was defined according to the ATP III guidelines of the 2001 NCEP and guidelines from the 2005 AHA/NHLBI. The WC criteria were modified for the Asian study population.10, 23 Subjects who met more than three of the following criteria were considered to have MetS: (1) WC>90 cm, (2) serum TG≥150 mg/dl, (3) serum HDL-C<40 mg/dl, (4) blood pressure≥130/85 mm Hg or taking anti-hypertensive drugs, and (5) FBG levels≥100 mg/dl or taking anti-hyperglycemic drugs.
Definition of dyslipidemia
We defined dyslipidemia according to the criteria of the NCEP-ATP III.9 Dyslipidemia was defined on the basis of the presence of one or more of the following: (1) TC≥240 mg/dl, (2) HDL-C<40 mg/dl, (3) LDL-C≥160 mg/dl, (4) TG≥200 mg/dl, and (5) use of one or more anti-dyslipidemic drugs. We also calculated other surrogate parameters for dyslipidemia; non-HDL-C (NHDL-C) and TG/HDL-C. NHDL-C was calculated as TC minus HDL-C and we defined a high NHDL-C level as ≥160 mg/dl.24 High TG/HDL-C was defined as more than 3.8, as this has been shown to be correlated with cardiovascular disease.25
Statistical analysis
In order to analyze the baseline characteristics of the study participants, we divided our study participants into tertiles for mean IOP and compared the mean values of cardiometabolic risk factors among the three groups using the χ2-test and one-way analysis of variance. We compared the mean IOP of subjects with and without cardiometabolic diseases and the component of MetS using a χ2-test (Figure 1). To identify the correlations between IOP and cardiometabolic risk factors, we performed a Pearson’s correlation analysis. We performed multivariate linear regression to compare the relationship between the cardiometabolic risk factors and IOP, after adjusting for age, BMI, alcohol consumption, smoking history, and regular exercise. All statistical tests were two-tailed and a P-value of <0.05 was considered to be statistically significant. Statistical analysis was performed using the SAS software package version (9.2) for Windows (SAS Institute, Cary, NC, USA).
(a) Comparison of mean IOP between subjects with and without major cardiometabolic diseases. DM, diabetes mellitus; MetS, metabolic syndrome. *P-values were obtained using the χ2-test and were <0.001. (b) Comparison of mean IOP between subjects with and without MetS components. BP, blood pressure; FBG, fasting blood glucose; HDL-C, high-density lipoprotein cholesterol; TG, triglyceride. *P-values were obtained by χ2-test and were <0.001.
Results
We classified subjects into tertiles on the basis of their average IOP values. The average IOP increased with age but the relationship between IOP and age was not significant (P=0.755). In terms of anthropometric measurements, weight, BMI, WC, SBP, and DBP differed significantly among three IOP groups (P<0.001). All biochemical markers except HDL-C and the prevalence of MetS differed significantly among three IOP groups (P<0.05 and P<0.001, respectively). The mean values of SBP, DBP, FBG, insulin, HOMA-IR, TC, LDL-C, TG, NHDL-C, TG/HDL-C, and MetS were lowest in Tertile 1 (Table 1).
We compared the average IOP in the group with major cardiometabolic diseases (Figure 1a) and the average IOP in the group with components of MetS (Figure 1b) with that of the normal group. The group with obesity, HTN, DM, and MetS had significantly higher average IOP (P<0.005); however, the group with dyslipidemia had lower IOP although the association was not significant (P=0.182) (Figure 1). Participants with abdominal obesity, high BP, high TG, and high FBG had significantly higher IOP than that of the normal group (P<0.005). However, there was no significant difference between the group with low HDL-C and the normal group (P=0.594) (Figure 1).
In order to assess the relationship between IOP and cardiometabolic risk factors, R2 was calculated in Table 2. With the exception of WC and HDL-C, all cardiometabolic risk factors were significantly associated with IOP (P<0.005). Of the cardiometabolic risk factors, the R2 of DBP and IOP was the highest and the second highest was the R2 of SBP and IOP (R2=0.0158 and 0.0148, respectively).
Multivariate linear regression analysis showed that IOP was positively correlated with BMI, SBP, DBP, FBG, HOMA-IR, TC, HDL-C, LDL-C, TG, NHDL-C, and TG/HDL-C in Model 1 (all P<0.05). After adjusting for all covariates (model 2), there were also significantly positive correlations between IOP and BMI, SBP, DBP, FBG, HOMA-IR, TC, HDL-C, LDL-C, TG, NHDL-C, and TG/HDL-C (all P<0.05) (Table 3).
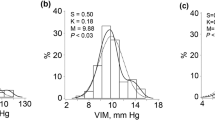
As the effect sizes of the various parameters of cardiometabolic risk factors were different, they were not isometrically comparable. Therefore, we converted the raw measurements to z-scores, or standardized scores. These scores express the distance from the mean for the measurement, allowing us to place cardiometabolic risk factors together on the same graph according to their tertile of IOP (Figure 2). DBP was the strongest explanatory variable in the relationship between IOP and cardiometabolic risk factors. Other parameters including BMI, SBP, FBG, insulin, HOMA-IR, TC, LDL-C, TG, and NHDL-C, and TG/HDL-C were also strong explanatory factors, while WC and HDL-C were not.
Standardized score of means of various cardiometabolic risk factors according to the tertile group of mean IOP. BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; FBG, fasting blood glucose; HOMA-IR, homeostasis model assessment of insulin resistance; TC, total cholesterol, HDL-C, high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol; TG, triglyceride; NHDL-C, non-HDL-C. *P-values were obtained by χ2-test and were <0.05.
Discussion
In this study, mean IOP was elevated in South Korean men with obesity, HTN, DM, MetS, abdominal obesity, and high TG, FBG, and BP. Of the cardiometabolic risk factors, IOP was positively correlated with BMI, SBP, DBP, FBG, HOMA-IR, TC, TG, LDL-C, HDL-C, NHDL-C, and TG/HDL-C.
The positive relationship between SBP and IOP has been well established in some studies.15, 17, 18, 20, 26, 27, 28, 29, 30, 31 In the Rotterdam study, SBP and HTN were shown to be associated with IOP in 4187 Caucasian subjects.27 In a study of a Latino population of 5958 subjects, a positive correlation was found to exist between SBP and IOP.29 Positive correlations between SBP and IOP were also found in two Korean studies.20, 31 In the relationship between IOP and DBP, many studies showed inconclusive relationship.26, 27, 28, 29, 30 In a community, there was no association between IOP and DBP among Korean men, but there was a positive association among Korean women.30 But, DBP showed the strongest association with increased IOP in this study. The hypothetical mechanism for this relationship is that the elevated blood pressure increases ciliary arterial blood pressure and ultrafiltration pressure of aqueous humor,26 and also increases corticosteroid levels and sympathetic tone, particularly in hypertensive subjects.32 Further studies are needed to explain these inconsistent results.
BMI has also been shown to be positively correlated with IOP in many studies.15, 16, 19, 29 A suggested mechanism for this relationship is that the increase of intraorbital fat tissues raises the episcleral venous pressure and blood viscosity, leading to a reduction in aqueous outflow and an increased IOP.26 Methodological cause has also been suggested that the increased IOP recorded in obese people is due to a transitory elevation resulting from breath holding and thoracic compression during Goldmann tonometry examination.33
Although there is no clear mechanism that explains the positive relationship between IOP and HOMA-IR and DM, many studies have revealed positive results.3, 13, 17, 20, 27, 28, 31, 34 In an epidemiological study, diabetes-related autonomic dysfunction and genetic factors are considered to be explanatory mechanisms.35 In addition, corneal stiffening has also been suggested as a factor that elevates IOP36 as a result of corneal collagen cross-links induced by glycation.37 Although we did not analyze central corneal thickness in this study, people with DM have been shown to have high central corneal thickness in previous studies.34, 38
The aforementioned findings suggest a possible linkage between MetS and IOP, since MetS is a state of insulin resistance represented by HOMA-IR. As in this study, MetS has been shown to be associated with high IOP in many previous studies.17, 20, 30, 31, 34 Some Korean studies have found a positive correlation between the number of components of MetS and IOP even after adjusting for BP and FBG.30, 31 Many mechanisms also influence the positive correlation between MetS and IOP, but the direct mechanism for this is currently unknown. Sympathetic hyperactivation,39 and aquaporins that are known to be related with insulin resistance40 are considered as potential pathophysiological mechanisms of the relationship between MetS and IOP.
Some studies, including this one, have indicated a positive correlation between lipid parameters and increased IOP.17, 20, 28, 30 Among lipid variables, TG has been shown to have an especially strong association with IOP, but results differ according to gender and study design.17, 20, 30 Unlike previous studies, we found a positive correlation between IOP and all lipid variables, including NHDL-C and TG/HDL-C, which are representative markers of small dense LDL-C. It may be assumed that South Korean men are prone to increased IOP when atherogenic dyslipidemia is present. These results may be explained by an increase in blood viscosity and a decrease in aqueous outflow,41 but further studies are needed to investigate the mechanisms behind the relationship between elevated IOP and dyslipidemia.
This study has several strengths. To the best of our knowledge, this study is the first to examine the relationship between IOP and cardiometabolic risk factors using a large, representative population of Korean men. Previous studies have been limited to particular regions. The other strength is that we used novel dyslipidemic parameters, such as TG/HDL-C and NHDL-C, which are related to atherogenic dyslipidemia, and showed a positive correlation between DBP and IOP in Korean men. Third, we adjusted for several variables such as age, BMI, alcohol consumption, smoking, and physical activity.
However, there are several limitations to the present study. First, this study is a cross-sectional study, so it is difficult to show a causal relationship or to analyze potential mechanisms. Second, we did not measure the central corneal thickness and corneal curvatures that are related to IOP. Third, we did not check the time of the day and the season of the year the IOP measurements were taken. Some studies showed seasonal and diurnal variations of IOP, and IOP was slightly high in winter seasons and in the morning.28, 42, 43
In conclusion, we found that risk factors for cardiovascular diseases, including components of MetS, appear to be associated with a rise in IOP in South Korean men. Further prospective studies are needed to assess whether or not improving cardiometabolic risk factors lowers the risk of IOP and glaucoma.

References
Sommer A . Intraocular pressure and glaucoma. Am J Ophthalmol 1989; 107 (2): 186–188.
Le A, Mukesh BN, McCarty CA, Taylor HR . Risk factors associated with the incidence of open-angle glaucoma: the visual impairment project. Invest Ophthalmol Vis Sci 2003; 44 (9): 3783–3789.
Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z . Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology 2007; 114 (11): 1965–1972.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA et al. The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120 (6): 714–720 discussion 829-30.
Braithwaite RS, Col NF, Wong JB . Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc 2003; 51 (3): 364–370.
Van Der Klift M, Pols HA, Geleijnse JM, Van Der Kuip DA, Hofman A, De Laet CE . Bone mineral density and mortality in elderly men and women: the Rotterdam Study. Bone 2002; 30 (4): 643–648.
Reaven GM . Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988; 37 (12): 1595–1607.
Dandona P, Aljada A, Chaudhuri A, Mohanty P, Garg R . Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation. Circulation 2005; 111 (11): 1448–1454.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285 (19): 2486–2497.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112 (17): 2735–2752.
Ford ES, Giles WH, Dietz WH . Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 2002; 287 (3): 356–359.
Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. The Third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005: Health Examination. Korea Centers for Disease Control and Prevention: Seoul, 2006; 2016–2020.
Carel RS, Korczyn AD, Rock M, Goya I . Association between ocular pressure and certain health parameters. Ophthalmology 1984; 91 (4): 311–314.
Schulzer M, Drance SM . Intraocular pressure, systemic blood pressure, and age: a correlational study. Br J Ophthalmol 1987; 71 (4): 245–249.
Fukuoka S, Aihara M, Iwase A, Araie M . Intraocular pressure in an ophthalmologically normal Japanese population. Acta Ophthalmol 2008; 86 (4): 434–439.
Tomoyose E, Higa A, Sakai H, Sawaguchi S, Iwase A, Tomidokoro A et al. Intraocular pressure and related systemic and ocular biometric factors in a population-based study in Japan: the Kumejima study. Am J Ophthalmol 2010; 150 (2): 279–286.
Chang YC, Lin JW, Wang LC, Chen HM, Hwang JJ, Chuang LM . Association of intraocular pressure with the metabolic syndrome and novel cardiometabolic risk factors. Eye 2010; 24 (6): 1037–1043.
Lee JK, Han YS, Lee JS, Kim YK . The relationship between intraocular pressure and age, hypertension and obesity index in ocular hypertensive patients. J Korean Ophthalmol Soc AID 2009; 50 (7): 1082–1087 KO.
Lee JK, Lee JS, Kim YK . The relationship between intraocular pressure and health parameters. J Korean Ophthalmol Soc AID. 103341/jkos2009501105 [doi] 2009; 50 (1): 105–112 KO.
Park BJ, Park JO, Kang HT, Lee YJ . Elevated intraocular pressure is associated with metabolic syndrome in postmenopausal women: the Korean National Health and Nutrition Examination Survey. Menopause 2013; 20 (7): 742–746.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28 (7): 412–419.
Hagstromer M, Oja P, Sjostrom M . The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr 2006; 9 (6): 755–762.
Alberti KG, Zimmet P, Shaw J . The metabolic syndrome-a new worldwide definition. Lancet 2005; 366 (9491): 1059–1062.
Park H, Kim K . Association of alcohol consumption with lipid profile in hypertensive men. Alcohol Alcohol 2012; 47 (3): 282–287.
Hanak V, Munoz J, Teague J, Stanley A Jr, Bittner V . Accuracy of the triglyceride to high-density lipoprotein cholesterol ratio for prediction of the low-density lipoprotein phenotype B. Am J Cardiol 2004; 94 (2): 219–222.
Bulpitt CJ, Hodes C, Everitt MG . Intraocular pressure and systemic blood pressure in the elderly. Br J Ophthalmol 1975; 59 (12): 717–720.
Dielemans I, Vingerling JR, Algra D, Hofman A, Grobbee DE, de Jong PT . Primary open-angle glaucoma, intraocular pressure, and systemic blood pressure in the general elderly population. The Rotterdam study. Ophthalmology 1995; 102 (1): 54–60.
Klein BE, Klein R, Linton KL . Intraocular pressure in an American community. The Beaver dam eye study. Invest Ophthalmol Vis Sci 1992; 33 (7): 2224–2228.
Memarzadeh F, Ying-Lai M, Azen SP, Varma R . Associations with intraocular pressure in Latinos: the Los Angeles Latino eye study. Am J Ophthalmol 2008; 146 (1): 69–76.
Park SS, Lee EH, Jargal G, Paek D, Cho SI . The distribution of intraocular pressure and its association with metabolic syndrome in a community. Journal of preventive medicine and public health=Yebang Uihakhoe chi 2010; 43 (2): 125–130.
Oh SW, Lee S, Park C, Kim DJ . Elevated intraocular pressure is associated with insulin resistance and metabolic syndrome. Diabetes Metab Res Rev 2005; 21 (5): 434–440.
Gherghel D, Hosking SL, Orgul S . Autonomic nervous system, circadian rhythms, and primary open-angle glaucoma. Surv Ophthalmol 2004; 49 (5): 491–508.
dos Santos MG, Makk S, Berghold A, Eckhardt M, Haas A . Intraocular pressure difference in Goldmann applanation tonometry versus Perkins hand-held applanation tonometry in overweight patients. Ophthalmology 1998; 105 (12): 2260–2263.
Su DH, Wong TY, Wong WL, Saw SM, Tan DT, Shen SY et al. Diabetes, hyperglycemia, and central corneal thickness: the Singapore Malay eye study. Ophthalmology 2008; 115 (6): 964–8 e1.
Clark CV, Mapstone R . The prevalence of diabetes mellitus in the family history of patients with primary glaucoma. Doc Ophthalmol 1986; 62 (2): 161–163.
Krueger RR, Ramos-Esteban JC . How might corneal elasticity help us understand diabetes and intraocular pressure? J Refract Surg 2007; 23 (1): 85–88.
Sady C, Khosrof S, Nagaraj R . Advanced Maillard reaction and crosslinking of corneal collagen in diabetes. Biochem Biophys Res Commun 1995; 214 (3): 793–797.
European Glaucoma Prevention Study Pfeiffer N, Torri V, Miglior S, Zeyen T, Adamsons I et al. Central corneal thickness in the European glaucoma prevention study. Ophthalmology 2007; 114 (3): 454–459.
Mancia G, Bousquet P, Elghozi JL, Esler M, Grassi G, Julius S et al. The sympathetic nervous system and the metabolic syndrome. J Hypertens 2007; 25 (5): 909–920.
MacDougald OA, Burant CF . Obesity and metabolic perturbations after loss of aquaporin 7, the adipose glycerol transporter. Proc Natl Acad Sci USA 2005; 102 (31): 10759–10760.
Shiose Y, Kawase Y . A new approach to stratified normal intraocular pressure in a general population. Am J Ophthalmol 1986; 101 (6): 714–721.
Blumenthal M, Blumenthal R, Peritz E, Best M . Seasonal variation in intraocular pressure. Am J Ophthalmol 1970; 69 (4): 608–610.
Qureshi IA, Xiao RX, Yang BH, Zhang J, Xiang DW, Hui JL . Seasonal and diurnal variations of ocular pressure in ocular hypertensive subjects in Pakistan. Singapore Med J 1999; 40 (5): 345–348.
Acknowledgements
The authors thank the Korean Center for Disease Control and Prevention, which performed KNHANES.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author Contributions
Y-H K: concept and design, data collection, statistics, writing of the manuscript; S W J, S-M K: data collection, analysis, and draft; G-E N, S J B: data collection and critical revision; K D H, S-Y J: concept and design, statistics, critical revision; A R B, K-H C, Y S C: data collection and analysis; D-H K: concept and design, statistics, critical revision.
Rights and permissions
About this article
Cite this article
Kim, YH., Jung, S., Nam, GE. et al. High intraocular pressure is associated with cardiometabolic risk factors in South Korean men: Korean National Health and Nutrition Examination Survey, 2008–2010. Eye 28, 672–679 (2014). https://doi.org/10.1038/eye.2014.43
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.43
This article is cited by
-
Relationship between blood pressure and intraocular pressure in the JPHC-NEXT eye study
Scientific Reports (2022)
-
Triglycerides and Open Angle Glaucoma – A Meta-analysis with meta-regression
Scientific Reports (2017)
-
The association between intraocular pressure and different combination of metabolic syndrome components
BMC Ophthalmology (2016)
-
Topical ocular dexamethasone decreases intraocular pressure and body weight in rats
Journal of Negative Results in BioMedicine (2016)
-
Differential Association of Metabolic Risk Factors with Open Angle Glaucoma according to Obesity in a Korean Population
Scientific Reports (2016)