Abstract
Purpose
To determine the rate of progression of eyes with subclinical diabetic macular edema (DME) to clinically apparent DME or DME necessitating treatment during a 2-year period.
Methods
In all, 43 eyes from 39 study participants with subclinical DME, defined as absence of foveal center edema as determined with slit lamp biomicroscopy but a center point thickness (CPT) between 225 and 299 μm on time domain (Stratus, Carl Zeiss Meditec) optical coherence tomography (OCT) scan, were enrolled from 891 eyes of 582 subjects screened. Eyes were evaluated annually for up to 2 years for the primary outcome, which was an increase in OCT CPT of at least 50 μm from baseline and a CPT of at least 300 μm, or treatment for DME (performed at the discretion of the investigator).
Results
The cumulative probability of meeting an increase in OCT CPT of at least 50 μm from baseline and a CPT of at least 300 μm, or treatment for DME was 27% (95% confidence interval (CI): 14%, 38%) by 1 year and 38% (95% CI: 23%, 50%) by 2 years.
Conclusions
Although subclinical DME may be uncommon, this study suggests that between approximately one-quarter and one-half of eyes with subclinical DME will progress to more definite thickening or be judged to need treatment for DME within 2 years after its identification.
Similar content being viewed by others
Introduction
Diabetic macular edema (DME) is a common cause of visual loss in people with diabetes. Clinical diagnosis via ophthalmoscopy is supplemented frequently by imaging of the macula with optical coherence tomography (OCT). The role of OCT images in eyes with diabetic retinopathy, in which clinical examination does not identify DME, has not been determined. For example, it is unknown whether there is value in identifying subclinical DME that affects the fovea or center of the macula. Subclinical DME is being used in this paper to describe the situation in which macular thickening is present on quantitative indices of the center point obtained from OCT yet thickening of the center of the macula is not seen on clinical examination. This finding may be of increasing importance. As the utilization of OCT in patients with diabetic retinopathy increases, the identification of eyes with subclinical DME should become more frequent so that understanding its natural history may be of value in the management of this finding.
To provide information about the course of initially untreated subclinical center-involved DME, the Diabetic Retinopathy Clinical Research Network (DRCR.net) conducted an observational study in which eyes with subclinical center-involved DME were followed over a 2-year period with repeat clinical examinations and OCT assessments. Subclinical center-involved DME was defined as: (1) no edema involving the center of the fovea as determined by slit-lamp biomicroscopy without reference to whether an indirect lens or contact lens viewing system was used; (2) a center point thickness (CPT) measurement on Stratus OCT (Carl Zeiss Meditec, Dublin, CA, USA) of ≥225 μm and ≤299 μm. A CPT of ≥225 μm is more than 2 standard deviations greater than previously published normal values for this measurement in diabetic persons,1 and a CPT >299 μm would represent a value likely judged to be recognized as clinically apparent thickening.2 The primary study objective was to determine how often eyes with subclinical DME have an increase in OCT-measured CPT of at least 50 μm and a thickness of at least 300 μm (a measurement at which clinically apparent edema is almost always noted) or receive treatment for DME (at the discretion of the investigator) during a 2-year follow-up period.
Methods
Screening for this observational multi-center study was conducted by the DRCR.net at 33 clinical sites throughout the United States, of which 17 clinical sites enrolled eligible participants. The study adhered to the tenets of the Declaration of Helsinki. The protocol and Health Insurance Portability and Accountability Act compliant informed consent forms were approved by multiple institutional review boards. Each study participant gave written informed consent before participation in the study. The protocol is available on the DRCR.net website (www.drcr.net, date accessed on 8 June 2011). The key aspects of the protocol pertinent to this manuscript are summarized below.
Eligible study participants were at least 18 years old with type 1 or type 2 diabetes, had best corrected Electronic-Early Treatment Diabetic Retinopathy Study (E-ETDRS Visual Acuity Test)3 visual acuity letter score ≥74 (approximate Snellen equivalent of 20/32 or better), a normal central macular thickness on stereoscopic fundus examination, OCT-measured CPT 225 to 299 μm confirmed by a reading center, no DME for which treatment was anticipated, and mild nonproliferative diabetic retinopathy (ETDRS level 35) or worse on clinical examination. Initially, the OCT CPT eligibility criterion was 200 to 299 μm, but was changed to CPT 225 to 299 μm when 225 μm was determined to be ∼2 SD above the mean CPT for people with diabetes and minimal or no diabetic retinopathy.1 Only eyes meeting the revised eligibility criteria were included in the analyses. Other details of the protocol, including exclusion criteria, are available on-line at www.drcr.net. A study participant could have two study eyes in the trial only if both were eligible at the time of study entry.
From a companion study,1 four eyes identified with subclinical DME but a retinopathy level better than 35 at the reading center also were analyzed with this cohort, because at least mild nonproliferative diabetic retinopathy was detected by the enrolling investigator on clinical examination.
Study eyes were to be followed for 2 years or until the primary outcome was met. At baseline, 1 year, and 2 years, the following testing was performed using DRCR.net standard procedures (www.drcr.net accessed on 21 December 2009) in the following sequence: (1) measurement of best corrected E-ETDRS Visual Acuity Test3 visual acuity letter score; (2) clinical assessment for the presence of center-involved DME using slit lamp biomicroscopy; (3) OCT fast macular map scans centered on the fovea (Stratus OCT Zeiss 3.0 or higher); and (4) stereoscopic fundus photographs (seven standard fields using 30 degree film camera systems at baseline and three fields at 12 and 24 months). Hemoglobin A1c measurements within the prior 3 months and blood pressure measurements also were obtained at baseline. If DME progressed so that the investigator judged that treatment was indicated before the 2-year visit, then testing as planned for the 1 and 2-year study visits was to be performed before any treatment for DME was given. Fundus photographs and OCT scans were sent to the Reading Center. Grading was completed using standard procedures that included correcting measurements of OCT CPT manually if values offered by the software were based on an incorrect boundary line placement by the software algorithms.
Statistical methods
The primary outcome was the cumulative probability of eyes that met either of the following criteria: (1) an increase in OCT CPT of at least 50 μm and a CPT of at least 300 μm at either the 1 or 2-year visits or (2) treatment for DME before 2 years (eyes treated at 2 years were not counted as having met the primary outcome). An effective sample size of ∼200 study eyes (enrollment of 220 allowing for 10% incomplete follow-up) was planned so that the half-width of a 2-sided 95% confidence interval (CI) on the proportion of eyes meeting the primary outcome criteria would be less than 0.05, assuming an outcome proportion of 15%. Recruitment was slower than planned, and enrollment was halted after 14 months of recruitment in the absence of knowledge of the outcome data.
The cumulative probability of eyes meeting criteria for the primary outcome and a 95% CI were computed. The marginal Cox proportional hazards model for clustered data was used for all analyses in order to account for study participants with two study eyes.4 Study participants who were lost to follow-up before meeting the primary outcome were censored at their last visits. SAS software version 9.1 (SAS Institute, Cary, NC, USA) was used for all analyses.
Results
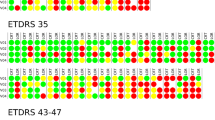
Between January 2006 and May 2007, 891 eyes among 582 study participants were screened for subclinical macular edema. Of the 891 eyes screened, 43 eyes (4.8%) of 39 participants had OCT CPT between 225 and 299 μm and retinopathy level ≥35 as graded on fundus photos or on clinical exam (Figure 1). Of the 848 eyes not eligible for follow-up, 601 (67%) eyes had at least mild-NPDR (ETDRS level 35) on color fundus photographs, clinical examination or both. Baseline characteristics of the enrolled study participants and study eyes are summarized in Table 1. Follow-up was complete (primary outcome criteria met or 2-year follow-up completed without meeting criteria for primary outcome) for 37 (86%) of the 43 eyes.
Flowchart for eyes (study participants) screened, enrolled, and followed-up. *The protocol originally allowed eyes with an OCT CPT of 200 to 299 μm to be enrolled; however, the protocol was changed to only include eyes with a CPT of 225 to 299 μm. This change decreased the number of eyes eligible from 104 to 48. An additional five eyes with minimal or no diabetic retinopathy as determined by grading of fundus photographs and by the enrolling investigator on clinical examination were excluded from analysis, resulting in 43 eligible eyes.
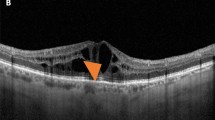
Among the 43 eyes, 16 eyes met the primary outcome definition, including 7 eyes with OCT CPT increase of at least 50 μm from baseline and a measurement of at least 300 μm at an annual visit and 9 other eyes that received treatment for DME before 2 years (3 of the 9 eyes were treated before obtaining follow-up visual acuity or OCT data) (Table 2, Figure 2). Of the 16 eyes that met the primary outcome, 12 (75%) eyes met the outcome by 1 year (Table 2). As shown in Figure 3, the 1-year cumulative probability of the primary outcome was 27% (95% CI: 14%, 38%) and the 2-year cumulative probability was 38% (95% CI: 23%, 50%). When the eyes lost to follow-up were not censored and instead included in the denominator for estimating the proportion of eyes meeting the primary outcome at 2 years, the estimated proportion and 95% CI was 38% (95% CI 23%, 50%).
Change in OCT CPT from baseline to the 2-year visit or last visit according to baseline thickness stratified by primary outcome status. Primary outcome definition: (1) OCT CPT increase of 50 μm from baseline to a thickness of at least 300 μm; or (2) treatment for DME prior to the 2-year visit. A total of eight eyes are missing OCT data: five eyes are missing all follow-up data; three eyes had a follow-up visit but an OCT was not performed before treatment. One study participant did not have a 2-year visit and data from the 1-year visit is used.
Cumulative probability and 95% CI of meeting the primary outcome by the 2-year follow-up visit. Primary outcome definition: (1) OCT CPT increase of 50 μm from baseline to a thickness of at least 300 μm at 1 year or 2-year visit; or (2) treatment for DME before the 2-year visit. Marginal Cox proportional hazards model for clustered data to account for study participants with 2 study eyes; 6 of the 44 eyes are censored due to missing follow-up data (5 eyes have no follow-up data and 1 eye only has a 1-year visit). ‡The number of eyes in follow-up at the start of the interval that had not previously met the definition for primary outcome. †The number of eyes meeting the definition for primary outcome during the subsequent 12-month period. §The number of eyes censored at the start of the interval.
The mean visual acuity at the time an eye reached the primary outcome was very good (∼20/25), with a mean change in visual acuity of -1 letter (Table 2). However, at the time of the primary outcome, 38% (95% CI 8%, 69%) of the 13 eyes with visual acuity data (3 eyes were treated before obtaining visual acuity and are missing data) had a visual acuity letter score of ≥5 letters lower than the baseline score, while 23% (95% CI 3%, 50%) had a visual acuity letter score ≥5 letters better than the baseline score.
Although the sample size was likely not sufficient to identify small differences in subgroups, there did not appear to be substantial differences in the cumulative probability of eyes meeting criteria for the primary outcome among the following planned baseline subgroups: gender, spherical equivalent, diabetic retinopathy severity level, OCT CPT, OCT retinal volume, number of thickened OCT subfields, and cystoid abnormalities on OCT. Among the four eyes from the companion study, that had subclinical DME at baseline and at least mild nonproliferative diabetic retinopathy detected by the enrolling investigator on clinical examination, but either no retinopathy or minimal diabetic retinopathy based on Reading Center assessment of fundus photographs, none progressed to the primary outcome by 2 years.
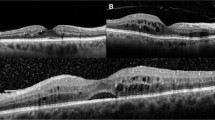
With respect to morphological changes over time, vitreoretinal interface abnormality, and subretinal fluid were graded on OCT by a central reading center. Of the 13 eyes, which met the primary outcome and had an OCT at the time that the eye met the primary outcome, 0 had subretinal fluid detected at the outcome visit, while 2 had a definite vitreoretinal interface abnormality present at the primary outcome visit. Of the 20 eyes, which did not meet the primary outcome with a follow-up OCT at the study participant's final visit, 5 had definite vitreoretinal interface abnormality present at that final visit.
Discussion
Subclinical DME as defined in this study was identified uncommonly. Accrual of additional study participants was discontinued when only 43 eligible eyes among 39 study participants were detected over 14 months of screening 891 eyes among 582 participants. Approximately 38% of eyes with this finding had increased thickening of at least 50 μm and a CPT of at least 300 μm at an annual visit or treatment for DME by 2 years. Most eyes that progressed to this endpoint did so within 1 year of follow-up. Over one-third of these eyes lost five or more letters from baseline when reaching this primary outcome, likely a true change in function as all of these eyes started with excellent visual acuity.
The percentage of eyes in this study that progressed to having DME, as defined in this study, was greater than the ∼25% of eyes without DME involving or threatening the center of the macula who progressed to clinically significant DME at 3 years in the ETDRS study.5 However, clinically significant DME in the ETDRS study was assessed through fundus photographs, which are different from OCT measurements, which may be more sensitive to detect foveal thickening. Furthermore, the ETDRS included eyes treated immediately with focal/grid photocoagulation or deferral of focal/grid photocoagulation. In the present study it was assumed that those eyes that were treated for DME before 2 years but did not have documentation of progression to clinical DME on OCT, as defined in this study, would have progressed by OCT by the 2-year visit. Of note, 8 of 21 eyes that did not meet the primary outcome had decreased by more than 50 μm during follow-up, a greater decrease than might be expected by chance alone. As glycated hemoglobin, blood pressure, and other systemic factors were not evaluated during follow-up, it is unknown if changes in any of these features may have been associated with either worsening or improvements on OCT.
Although several publications in the literature have addressed the existence of subclinical DME,2, 6 only one previous retrospective study has described the natural course of such eyes.7 Browning and Fraser7 described a cohort (with subclinical DME defined as recognition of DME on clinical exam but not clinically significant DME, as defined by the ETDRS, or macular edema not detected on clinical exam but detected on OCT) that was evaluated during a median follow-up period of 14 months, with a range of 7 to 25 months. In this cohort 48 (31%) of 153 eyes progressed to clinically significant DME, as defined by the ETDRS, and evaluated by OCT central subfield mean thickness, an outcome similar to the prospective outcome identified in this DRCR.net study. Additional studies would be of value as these results are limited by the small number of eyes identified and followed with subclinical DME.
In conclusion, identifying subclinical DME involving the center of the macula may not be warranted routinely for most eyes without evidence of DME in the center of the macula on clinical examination or other factors, such as existence of extensive diabetic retinopathy, as subclinical DME appears to be relatively uncommon (43 (4.8%) of the 891 eyes screened were enrolled) in the cohort evaluated in this study. However, this study suggests that between approximately one-quarter and one-half of eyes with subclinical DME will progress to more definite thickening or be judged to need treatment for DME within 2 years after its identification. As this study identified only a limited number of eyes with subclinical DME that subsequently progressed to more definitively apparent DME, the number of eyes, which may have a meaningful decrease in visual acuity when progression occurs, is not precise (∼8–69%). Nevertheless, if subclinical DME is identified, for example, while obtaining an OCT in an eye for purposes other than routine monitoring, one should be aware of the likelihood that many of these eyes will progress to more definitive thickening of the center of the macula or be judged to need treatment for DME within a year after its identification.

Change history
14 June 2012
This article has been corrected since Advance Online Publication and an erratum is also printed in this issue
References
Bressler NM, Edwards AR, Antoszyk AN, Beck RW, Browning DJ, Ciardella AP et al. Retinal thickness on Stratus optical coherence tomography in people with diabetes and minimal or no diabetic retinopathy. Am J Ophthalmol 2008; 145: 894–901.
Brown JC, Solomon SD, Bressler SB, Schachat AP, DiBernardo C, Bressler NM . Detection of diabetic foveal edema: contact lens biomicroscopy compared with optical coherence tomography. Arch Ophthalmol 2004; 122: 330–335.
Beck RW, Moke PS, Turpin AH, Ferris III FL, SanGiovanni JP, Johnson CA et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol 2003; 135: 194–205.
Lee EW, Wei LJ, Amato DA . Cox-type regression analysis for large numbers of small groups of correlated failure time observations. In: Klein JP, Goel PK (eds). Survival Analysis: State of the Art. Kluwer Academic: Dordrecht, 1992, pp 237–247.
Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema: Early Treatment Diabetic Retinopathy Study report no. 4. Int Ophthalmol Clin 1987; 27: 265–272.
Browning DJ, McOwen MD, Bowen Jr RM, O’Marah TL . Comparison of the clinical diagnosis of diabetic macular edema with diagnosis by optical coherence tomography. Ophthalmology 2004; 111: 712–715.
Browning DJ, Fraser CM . The predictive value of patient and eye characteristics on the course of subclinical diabetic macular edema. Am J Ophthalmol 2008; 145: 149–154.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
The most recently published list of the Diabetic Retinopathy Clinical Research Network investigators and staff can be found at www.drcr.net.
Appendix
Appendix
The Diabetic Retinopathy Clinical Research Network Clinical Sites that participated on this protocol:
Sites are listed in order by the number of subjects enrolled into the study. The number of subjects enrolled is noted in parenthesis preceded by the site location and the site name. Personnel are listed as (I) for study investigator, (C) for coordinator, (V) for visual acuity tester, and (P) for photographer.
Baltimore, MD, Elman Retina Group, P.A.: (25) Michael J Elman (I), Michelle D Sloan (C), JoAnn Starr (C, V), Theresa M Butcher (C), Pamela V Singletary (V), Nancy Gore (V), Teresa Coffey (V), Giorya Andreani (P), Peter Sotirakos (P), and Terri Cain (P).
Boston, MA, Joslin Diabetes Center (7): George S Sharuk (I), Paul G Arrigg (I), Deborah K Schlossman (I), Timothy J Murtha (I), Jennifer K Sun (I), Sabera T Shah (I), Margaret E Stockman (C, P, V), Ann Kopple (C), and Robert W Cavicchi (P).
Lexington, KY, Retina Associates of Kentucky (6): Thomas W Stone (I), John W Kitchens (I), William J Wood (I), Michelle Buck (V), Jeanne Van Arsdall (V), Judith L Cruz (V), Edward A Slade (P), and Stephen T Blevins (P).
Charlotte, NC, Charlotte Eye, Ear, Nose and Throat Assoc., P.A. (4): David Browning (I), Andrew N Antoszyk (I), Danielle R Brooks (C, V), Jennifer V Helms (C, V), Angela K Price (C, V), Melissa K Cowen (C, V), Angella S Karow (V), Heather L Murphy (V), Michael D McOwen (P), Linda M Davis (P), Loraine M Clark (P), Uma M Balasubramaniam (P), Donna McClain (P), and Michele E Powers (P).
Denver, CO, Denver Health Medical Center (4): Jon M Braverman (I), Antonio P Ciardella (I), Leif S Ryman (C), Sasha I Montalvo (V), Janelle Dane Zapata (V), Rosemary C Rhodes (V), and Debbie M Brown (P).
Chicago, IL, Northwestern University Feinberg School of Medicine (3): Alice T Lyon (I), Manjot K Gill (I), Lori A Kaminski (C, V), Lori E Ackatz (C), Laima M O'Donnell (V), Jonathan Shankle (P), and Dawn M. Ryan (P).
Lakeland, FL, Florida Retina Consultants (3): Scott M Friedman (I), Kelly A Blackmer (C), Jolleen S Key (C, P), Karen Sjoblom (V), Damanda A Fagan (V), Steve Carlton (P), and Allen McKinney (P).
Attleboro, MA, Southern New England Retina Associates (2): Magdalena G Krzystolik (I), Mary B Savell (C), Sandra Henriques (C, V), and Joanne E Bache (P).
Columbia, SC, Carolina Retina Center (2): Jeffrey G Gross (I), Amy M Flowers (C, V), Heidi K Lovit (V), and Randall L Price (P).
Seattle, WA, University of Washington Medical Center (2): James L Kinyoun (I), Susan A Rath (C, V), Brad C Clifton (P), and James D Leslie (P).
Slingerlands, NY, Retina Consultants, PLLC (2): Paul M Beer (I), Denise Garza (C), Eugenia Olmeda (C, V), Charisse Whitney (V), and Joe Fischer (P).
Baltimore, MD, Wilmer Eye Institute at Johns Hopkins (1): Sharon D Solomon (I), Susan Bressler (I), Mary Frey (C, V), Sandra West (C, V), Deborah Donohue (V), Janis Graul (P), and David Emmert (P).
Detroit, MI, Henry Ford Health System, Department of Ophthalmology and Eye Care Services (1): Paul Andrew Edwards (I), Sheila M Rock (C, V), Janet Murphy (C, V), Brian A Rusinek (P), and Tracy A Troszak (P).
Galveston, TX, University of Texas Medical Branch, Department of Ophthalmology and Visual Sciences (1): Garvin H Davis (I), Helen K Li (I), Happy Spillar (C), John M Bourg (V), Amber Crocker (P), and Craig N Kelso (P).
Kingsport, TN, Southeastern Retina Associates, P.C. (1): Howard L Cummings (I), Deanna Jo Long (C, P), Stacy Carpenter (V), and Julie P Berry (P).
Knoxville, TN, Southeastern Retina Associates, P.C. (1): Joseph M Googe (I), Christina T Higdon (C), Cecile Hunt (V), and Paul A Blais (P).
Milwaukee, WI, Medical College of Wisconsin (1): Judy E Kim (I), Dennis P Han (I),William J Wirostko (I), Dawn Alvarez (C, V), Jeanette Graf (C), Judy Flanders (V), Joseph R Beringer (P), and Dennis B Backes (P).
Palm Desert, CA, Southern California Desert Retina Consultants, M.C. (1): Clement K Chan (I), Kimberly S Walther (C), Sandra U Castillo (V), Kenneth M Huff (P), and Donna J Chesbrough (P).
Providence, RI, Retina Consultants (1): Caldwell W Smith (I), Robert H Janigian (I), Harold A Woodcome (I), Collin L DuCoty (C), Sylvia Varadian (C), Erika Banalewicz (V), Mark Hamel (P), and Alex L Nagle (P).
DRCR.net Coordinating Center: Jaeb Center for Health Research, Tampa, FL (staff as of 6/8/2011): Adam R Glassman (Director and Principal Investigator), Roy W Beck (Executive Director) Talat Almukhtar, Bambi J Arnold, Brian B Dale, Alyssa Baptista, Sharon R Constantine, Simone S Dupre, Allison R Edwards, Meagan L Huggins, Paula A Johnson, Lee Anne Lester, Brenda L Loggins, Emily B Malka, Shannon L McClellan, Michele Melia, Kellee M Miller, Pamela S Moke, Haijing Qin, Rosa Pritchard, Eureca Scott, and Cynthia R Stockdale.
Fundus Photograph Reading Center: University of Wisconsin-Madison, Madison, WI (staff as of 6/8/11): Matthew D Davis (Director Emeritus), Sapna Gangaputra (Co-Director), Ronald P Danis (Director and Principal Investigator), Larry Hubbard (Associate Director), James Reimers (Lead Color Photography Evaluator), Pamela Vargo (Lead Photographer), Ericka Moeller (Digital Imaging Specialist), Dawn Myers (Lead OCT Evaluator), Kristjan Burmeister (Project Manager), and Vonnie Gamma (Data Management).
DRCR.net Operations Center: Johns Hopkins University School of Medicine, Baltimore, MD (staff as of 6/8/2011): Neil M Bressler (Network Chair and Principal Investigator), Connie Lawson, Peggy R Orr, and Beth Wellman.
DRCR.net Vice Chairs: Susan B Bressler (2009–current), Scott Friedman (2009–current), Carl W Baker (2011-current), and Ingrid U Scott (2009–2010).
National Eye Institute: Eleanor Schron (2009–current), Donald F Everett (2003–2006, 2007–2009), and Päivi H Miskala (2006–2007).
Executive Committee: Raj K Maturi (2009–present; Chair 2010) Neil M Bressler (2006–present; Chair 2006–2008), Lloyd Paul Aiello (2002–present; Chair 2002–2005), Carl W Baker (2009–present), Roy W Beck (2002–present), Susan B Bressler (2009–present), Alexander J Brucker (2009–present), Kakarla V Chalam (2009–present) Ronald P Danis (2004–present), Matthew D Davis (2002–present), Michael J Elman (2006–present; Chair 2009), Frederick L Ferris III (2002–present), Scott Friedman (2007–present), Adam R Glassman (2005–present), Joseph Googe, Jr (2009–present), Eleanor Schron (2009–present), JoAnn Starr (2009–present), and Jennifer K Sun (2009–present). Prior Members: Andrew N Antoszyk (2009), Abdhish Bhavsar (2007–2008), David M Brown (2006–2007), David J Browning (2005–2006), Donald F Everett (2002–2009), Joan Fish (2008–2009), Andreas Lauer (2007–2008), Kim McLeod (2002–2006), Päivi H Miskala (2005–2007), Cynthia J Grinnell (2006–2007), and Ingrid U Scott (2009–2010).
Prior DRCR.net General Steering Committee Members: Neil M Bressler (Protocol Chair 2005–2008) David Browning (2005–2008), Alexander J Brucker (2005–2008), Steve Carlton (2006–2007), Emily Y Chew (2005–2008), Ronald P Danis (2003–2008), Julia A Haller (2005–2008), Lloyd Paul Aiello (2003–2008), Carl W Baker (2007–2008), Debra Paige Bunch (2007–2008), Donald F Everett (2006–2008), Frederick L Ferris III (2005–2008), Don S Fong (2003–2007), Adam R Glassman (2005–2008), Jeffrey G Gross (2006–2007), Helen K Li (2006–2007), Dennis M Marcus (2007–2008), Päivi Miskala (2005–2007), and Angela K Price (2005).
Rights and permissions
About this article
Cite this article
Diabetic Retinopathy Clinical Research Network., Bressler, N., Miller, K. et al. Observational study of subclinical diabetic macular edema. Eye 26, 833–840 (2012). https://doi.org/10.1038/eye.2012.53
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.53
Keywords
This article is cited by
-
Characterisation of progression of macular oedema in the initial stages of diabetic retinopathy: a 3-year longitudinal study
Eye (2023)
-
Comparative Efficacy, Durability and Safety of Faricimab in the Treatment of Diabetic Macular Edema: A Systematic Literature Review and Network Meta-Analysis
Advances in Therapy (2023)
-
Statement of the German Ophthalmological Society, the German Retina Society, and the Professional Association of Ophthalmologists in Germany on treatment of diabetic macular edema
Der Ophthalmologe (2021)
-
Risk factors for fellow eye treatment in protocol T
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
Optical coherence tomography analysis of patients with untreated diabetic macular edema
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)