Abstract
Purpose
To analyze the clinical pattern of ocular toxoplasmosis (OT) in a referral centre in Serbia.
Patients and methods
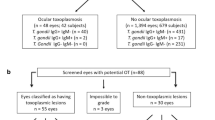
The medical records of consecutive patients admitted for OT to the single referral centre for uveitis in Serbia between 2006 and 2010 were retrospectively analyzed. OT was diagnosed on the basis of typical fundus lesions and positive serology for Toxoplasma.
Results
In a total of 457 uveitis patients, OT was the third leading cause, with 59 patients (12.9%). Most OT cases (73%) were monocular. An active primary retinal lesion was observed in 36% and recurrent OT in 64% patients. Localization of lesions was central/paracentral (44%), juxtapapillar (27%), peripheral (19%), and multifocal (10%). Other ocular manifestations of inflammation included vitritis (44%), anterior uveitis (19%), and retinal vasculitis (10%). Complications included choroidal neovascularization in two and exudative retinal detachment with cataract, glaucoma, and cystoid macular oedema in one patient each. The detection of Toxoplasma-specific IgM antibodies in a single patient indicates a low rate of OT concomitant with acute infection. After treatment, the mean best-corrected visual acuity (BCVA) increased significantly. However, 14 (24%) patients ended up legally blind in the affected eye, of which 2 (3%) with bilateral blindness, all with a very poor BCVA (0.047±0.055) at presentation. Visual impairment and treatment outcome were both associated with central localization of lesions (P<0.0001 and P=0.006, respectively).
Conclusion
OT is a significant cause of posterior uveitis in Serbia. Patients should be aware of the recurring nature of OT and react immediately if symptoms occur.
Similar content being viewed by others
Introduction
Toxoplasma gondii is a cosmopolitan protozoan parasite that has been estimated to infect one-third of the global population. Although generally mild and self-limiting in immunocompetent individuals, Toxoplasma infection may cause life-threatening disease in the fetus and in the immunosuppressed host. Historically, ocular disease was the first clinical entity to be associated with toxoplasmosis1 and has long been a well-known consequence of congenital infection.
Ocular toxoplasmosis (OT) most often presents as focal retinochoroiditis, which is considered to be triggered by the reactivation of dormant parasites in the retina.2 Lesions can occur anywhere in the fundus and may be vision-threatening if localized in the posterior pole. Toxoplasmosis is actually the most common cause of infectious posterior uveitis worldwide.2 Formerly considered to result mainly from congenital infection,3 OT has in the past decades been well established to occur both after congenital and acquired infection.1, 2, 4, 5, 6, 7 Indeed, a greater frequency of acquired than congenital infection in the origin of OT has been reported in several clinical series, both in Europe and in South America.4, 5, 6 However, it appears that congenital infections cause a more severe OT.6 The geographic differences in the epidemiology of OT reflect the genetic variability in the parasite strains occurring in the respective regions; that is, strains from South America, responsible for the often severe clinical course of toxoplasmosis on this continent, are often type-1, or recombinant, and generally divergent from those in Europe and North America where a vast majority of all isolates belongs to type-2.8, 9, 10, 11 In Serbia, the seroprevalence of toxoplasmosis is currently estimated at 30–35%12 and type-2 genospecies has been isolated.13
As fetal infection may only develop following maternal primary infection in pregnancy, congenital toxoplasmosis is a preventable disease; therefore, the incidence of OT of congenital origin may be expected to decrease in line with successful prevention strategies implemented in a particular milieu. However, acquired infection, which is often inapparent and therefore clinically unrecognized, and the recognition of its role in the origin of OT, is responsible for the currently increased interest in the study of OT.
Because the frequency and characteristics of OT have never been reported for Serbia, we conducted a study to analyze the clinical pattern of OT in a Serbian referral centre.
Patients and methods
A retrospective analysis of the medical records of consecutive patients admitted for OT to the Uveitis Department of the Institute for Eye Diseases in Belgrade between 01 January 2006 and 31 December 2010 was performed. This department is the single referral centre for uveitis in Serbia. All patients underwent complete ophthalmological examination, including clinical history, visual acuity (VA) assessment (measured by Snellen chart at 6 m and converted to decimal notation), applanation tonometry, slit lamp examination, and fundus examination with the three-mirror lens. In addition, fundus photography, fluorescein angiography, and optical coherence tomography were performed if clinically appropriate.
OT was diagnosed on the basis of clinical findings in the fundus and positive serology for Toxoplasma. Active OT was defined as the presence of an active whitish focal retinochoroidal lesion in either eye; if no associated pigmented retinochoroidal scars were present in either eye, it was considered primary OT and conversely, if there was a scar in either eye, OT was considered recurrent (termed satellite if localized at the borders of the scars). In patients with two or more episodes, the last episode of active OT was the one analyzed.
Detection of IgG and IgM antibodies specific for T. gondii was performed using an ELISA test (Enzygnost Toxoplasmosis IgG and Enzygnost Toxoplasmosis IgM tests, Siemens Healthcare Diagnostics, Marburg, Germany) according to the manufacturer's instructions. The test for IgG antibody was quantitative and the results were expressed in IU/ml, whereas the one for IgM antibody was qualitative.
The study has followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Clinical Centre of Serbia.
Data were analyzed using SPSS 15.0 (SPSS Inc., Chicago, IL, USA). Methods used included Student's t-test for comparison of numerical variables and χ2 or Fischer's exact test (as appropriate) for categorical variables. The level of statistical significance was 0.05.
Results
A total of 457 patients were admitted for uveitis during the study period, in whom OT was diagnosed in 59 (12.9%) patients. OT was the third leading cause of uveitis after anterior serofibrinous uveitis (n=131, 28.7%) and retinal vasculitis (n=75, 16.4%). Of all the uveitis patients, above one-half (53%) had posterior uveitis (n=243). Of these, OT accounted for 24.3% and was the second most common cause after retinal vasculitis. Importantly, OT was the most common cause of infectious uveitis.
Toxoplasma-specific IgG antibodies were detected in all patients, at a mean concentration of 96.4±15.8 IU/ml, ranging from 10–350 IU/ml. Specific IgM antibody was detected in a single patient, who was thus considered as acute infection.
Baseline demographic and clinical characteristics of patients with OT are shown in Table 1. The annual number of OT cases was 12, 10, 10, 11, and 16, respectively, for the period 2006–2010. Most (76%) patients were admitted for OT only once; among the 14 who were admitted twice or more, the mean follow-up (±SD) was 4.2±2.8 years (ranging from 1 to 9 years).
Female patients were slightly predominant (58%). Patients were relatively young (mean 34.9±16.6 years), with 76% younger than 45 years.
Of the 59 cases of OT, 43 (73%) were monocular and 16 (27%) binocular. In all the binocular cases, active OT was present in one eye and old scars were observed in the other. The eye with active OT was used to classify the localization of retinochoroidal lesions. In the analysis of the lesion localization, juxtapapillar lesions were considered central if within the vascular arcades and peripheral if outside, and similarly, multifocal lesions were considered central if at least one lesion was within the vascular arcades and peripheral if all foci were out of the vascular arcades.
According to medical history data, the current OT episode was the first one the patients were aware of in 42% and a recurrence in 58%. However, on clinical examination, active primary retinal lesions were observed in 36% and one or more satellite lesions in 64%. Although patients with primary OT were older (38.0±20.2 years) than those with recurrent OT (33.2±14.3), this difference was not significant (P=0.291).
In addition to the OT-defining lesions, the clinical presentation quite frequently included other manifestations of ocular inflammation. In contrast, complications were rare (Table 1).
Treatment was initiated immediately after diagnosis and included systemic Clindamycin 20–30 mg/kg for 3 weeks and/or a combination of pyrimethamine 2 × 25 mg 4–8 weeks with sulfadiazine 50–75 mg/kg and folic acid (leucovorin) 5 mg/day.
Best-corrected VA (BCVA) was the main parameter of the visual function. At admission, BCVA>0.3 was observed in 35 patients (Table 2) and ≤0.3 (moderate and severe visual impairment) in 24 patients, of which BCVA was ≤0.1 (0.04±0.03) in as many as 21. At the end of treatment, BCVA was improved in all; in those with initial BCVA>0.3, vision improved to almost normal levels and was obviously significantly (P<0.0001) better than in those with initial BCVA≤0.3. However, the improvement in these latter (P=0.006), as well as in those with initial BCVA≤0.1 (0.24±0.32; P=0.01), was clinically meaningful in only 10 patients, whereas 14 (24%) remained legally blind in the affected eye (Table 3). Of these, there were 2 (3%) cases of bilateral blindness (defined as BCVA of the better eye ≤0.1), whereas unilateral legal blindness (BCVA of the affected eye ≤0.1.) was observed in 12 (20%) patients. Patients who ended up with unilateral or bilateral blindness had extremely poor BCVA (0.047±0.055) at admission, which did not improve with treatment (P=0.808). Both moderate and severe visual impairment at admission and poor treatment outcome depended on the lesion localization (P<0.0001 and P=0.006, respectively), occurring only in case of lesions within the vascular arcades, whereas other ocular inflammation manifestations had no effect.
Discussion
Globally, there are wide variations in the distribution of OT among all uveitis cases, with the smallest percentage of OT observed in Japan (0.7%)14 and the highest in South America (39.8%).15 Europe, North Africa, and USA range between these two extremes (2.9–14%).16, 17, 18, 19, 20, 21 Thus, the data presented here from a Serbian referral centre showing OT in 12.9% of all patients admitted for uveitis, and in 24.3% of those with posterior uveitis, fit within those for Europe.
In our series, primary OT was observed in one-third and recurrent disease in two-thirds of all patients. Primary OT at first presentation has been reported at rates of 28–42.5%.5, 6, 22, 23 The greater frequency of recurrent disease may be accounted for by old peripheral lesions that go unnoticed by the patient; this is also supported by our clinical findings of a combination of active lesions and old retinochoroidal scars at a greater frequency than the patients were aware of.
Patient age is one of the several host factors that are believed to influence the severity of OT, and OT tends to be more severe at the extremes of age.24 Patients with OT are generally young adults, and in our study group, 76% of the patients were younger than 45 years. Similar results were found in other studies,5, 18, 22, 23, 25 for instance, Bosch-Driessen et al5 showed that the mean age at first presentation of OT was 29.5 years and that patients with primary ocular lesions were significantly older than those with combinations of active lesions and old scars. Also, Garweg et al25 reported that the mean age at the first occurrence of OT was 23.9 years and patients with only one episode were older at first manifestation than those with two episodes (29.6 and 17.9 years, respectively). However, in our series, although patients with active primary OT were older than patients with recurrent OT, the difference was not significant.
Even greater age differences have been reported according to the origin of OT; that is, in the study of Delair et al,6 patients with OT of congenital origin were only 9.1 (±8.8) and those with acquired origin 21.7 (±12.6) years old. We were not able to distinguish between congenital and acquired origin of OT, but detection of Toxoplasma-specific IgM antibodies in a single patient would indicate ophthalmic manifestations coinciding with acute infection in 5% among patients with primary OT. The proportion of OT concomitant with acute toxoplasmosis based on the detection of serological markers of acute infection (specific IgM/IgA antibodies) has varied in different reports from 0% in a series in Turkey26 to 11% in the Netherlands.5
At a rate of 73%, monocular presentation was clearly predominant and was within the range (64.3–86.4%) reported in other studies.18, 22, 23
Localization of retinal lesions was predominantly within the vascular arcades, whereas peripheral lesions and those multifocal outside the vascular arcades were less common. This resulted in an end-of-treatment unilateral legal blindness in 24% patients, all of which had central lesions. Predominance of OT lesions within the vascular arcades has been commonly observed,5, 18, 22, 23 for instance, of up to 84.2% of unilateral and 75% of bilateral cases in Italy,18 in a tertiary setting like ours where patients without visual impairment are infrequent, and of 73% in a Colombian cohort study.22 In contrast, in a population-based study in Brazil, peripheral lesions predominated (58.5%).27 However, with regard to visual outcome, unilateral legal blindness occurred in as many as 37.8% patients in the Colombian study.22 This is substantially higher than the results reported in Europe; the rate of 24% that we found was virtually the same as the one reported by Bosch-Driessen et al,5 whereas Scherrer et al28 found moderate to severe impairment (VA <0.3 or 0.05, respectively) in 27.5% of cases, which correlated with the central localization of lesions. These opposing results obviously reflect the general differences in the clinical evolution and severity of Toxoplasma infection in South America vs Europe and USA due to the above-mentioned differences in the respective parasite genotypes.
Ocular symptoms of inflammation did not differ, in type or in rate, from previous reports.22, 26 However, the rate of vitritis was lower than generally reported,22, 26, 29, 30 which may suggest that the level of vitreous haze was not always reliably recorded, particularly if low.
Complications of OT were not very marked. The 1.7% of cataract was similar to the findings of Balasundaram et al30 and Tugal-Tutkun et al,26 but considerably lower than the 13% reported by Bosch-Driessen et al;5 the comparatively high rate of complications in the latter series is presumably due to the longer follow-up. Interestingly, although raised IOP is often associated with an OT episode23, 29, 30 glaucoma as a complication is rare; that is, in the study of Tugal-Tutkun et al., although an IOP rise was seen in 8% patients during active OT, there was no case of glaucoma as a complication,26 nor was it seen in the series of Balasundaram et al.30 In our series, one case was complicated by glaucoma secondary to OT.
In conclusion, OT was found to be a common cause of posterior uveitis in patients in Serbia. Given its vision-threatening potential, patients with OT should be aware of the recurring nature of their disease and react immediately in case of visual symptoms. In addition, because of the recently recognized significance of acquired toxoplasmosis in the origin of OT, public health campaigns to increase general public awareness of this infection are needed. Further research should focus on distinguishing between congenital and acquired infections in the origin of OT.

References
Weiss LM, Dubey JP . Toxoplasmosis: A history of clinical observations. Int J Parasitol 2009; 39: 895–901.
Holland GN . Ocular toxoplasmosis: a global reassessment. Part I: epidemiology and course of disease. Am J Ophthalmol 2003; 136: 973–988.
Hogan MJ, Kimura SJ, O’Connor GR . Ocular toxoplasmosis. Arch Ophthalmol 1964; 72: 592–600.
Glasner PD, Silveira C, Kruszon-Moran D, Martins MC, Burnier JM, Silveira S et al. An unusually high prevalence of ocular toxoplasmosis in southern Brazil. Am J Ophthalmol 1992; 114: 136–144.
Bosch-Driessen LE, Berendschot TT, Ongkosuwito JV, Rothova A . Ocular toxoplasmosis: clinical features and prognosis of 154 patients. Ophthalmology 2002; 109: 869–878.
Delair E, Monnet D, Grabar S, Dupouy-Camet J, Yera H, Brezin AP . Respective roles of acquired and congenital infections in presumed ocular toxoplasmosis. Am J Ophthalmol 2008; 146: 851–855.
Talabani H, Mergey T, Yera H, Delair E, Brezin AP, Langsley G et al. Factors of occurrence of ocular toxoplasmosis. A review. Parasite 2010; 17: 177–182.
Vallochi AL, Muccioli C, Martins MC, Silveira C, Belfort Jr R, Rizzo LV . The genotype of Toxoplasma gondii strains causing ocular toxoplasmosis in humans in Brazil. Am J Ophthalmol 2005; 139: 350–351.
Khan A, Jordan C, Muccioli C, Vallochi AL, Rizzo LV, Belfort Jr R et al. Genetic divergence of Toxoplasma gondii strains associated with ocular toxoplasmosis, Brazil. Emerg Infect Dis 2006; 12: 942–949.
Dubey JP, Velmurugan GV, Chockalingam A, Pena HF, de Oliveira LN, Leifer CA et al. Genetic diversity of Toxoplasma gondii isolates from chickens from Brazil. Vet Parasitol 2008; 157: 299–305.
Dardé ML . Toxoplasma gondii, ‘new’ genotypes and virulence. Parasite 2008; 15: 366–371.
Bobić B, Nikolić A, Klun I, Vujanić M, Djurković-Djaković O . Undercooked meat consumption remains the major risk factor for Toxoplasma infection in Serbia. Parassitologia 2007; 49: 227–230.
Djurković-Djaković O, Klun I, Khan A, Nikolić A, Knežević-Ušaj S, Bobić B et al. A human origin type II strain of Toxoplasma gondii causing severe encephalitis in mice. Microbes Infect 2006; 8: 2206–2212.
Kitamei H, Kitaichi N, Namba K, Kotake S, Goda C, Kitamura M et al. Clinical features of intraocular inflammation in Hokkaido, Japan. Acta Ophthalmol 2009; 87: 424–428.
de-la-Torre A, Lopez-Castillo CA, Rueda JC, Mantilla RD, Gomez-Marin JE, Anaya JM . Clinical patterns of uveitis in two ophthalmology centres in Bogota, Colombia. Clin Experiment Ophthalmol 2009; 37: 458–466.
Rodriguez A, Calonge M, Pedroza-Seres M, Akova YA, Messmer EM, D’Amico DJ et al. Referral patterns of uveitis in a tertiary eye care center. Arch Ophthalmol 1996; 114: 593–599.
Khairallah M, Yahia SB, Ladjimi A, Messaoud R, Zaouali S, Attia S et al. Pattern of uveitis in a referral centre in Tunisia, North Africa. Eye (Lond) 2007; 21: 33–39.
Accorinti M, Bruscolini A, Pirraglia MP, Liverani M, Caggiano C . Toxoplasmic retinochoroiditis in an Italian referral center. Eur J Ophthalmol 2009; 19: 824–830.
Jakob E, Reuland MS, Mackensen F, Harsch N, Fleckenstein M, Lorenz HM et al. Uveitis subtypes in a german interdisciplinary uveitis center--analysis of 1916 patients. J Rheumatol 2009; 36: 127–136.
Cimino L, Aldigeri R, Salvarani C, Zotti CA, Boiardi L, Parmeggiani M et al. The causes of uveitis in a referral centre of Northern Italy. Int Ophthalmol 2010; 30: 521–529.
Nguyen AM, Seve P, Le SJ, Gambrelle J, Fleury J, Broussolle C et al. Clinical and etiological aspects of uveitis: a retrospective study of 121 patients referred to a tertiary centre of ophthalmology. Rev Med Interne 2011; 32: 9–16.
de-la-Torre A, Lopez-Castillo CA, Gomez-Marin JE . Incidence and clinical characteristics in a Colombian cohort of ocular toxoplasmosis. Eye (Lond) 2009; 23: 1090–1093.
London NJ, Hovakimyan A, Cubillan LD, Siverio Jr CD, Cunningham Jr ET . Prevalence, clinical characteristics, and causes of vision loss in patients with ocular toxoplasmosis. Eur J Ophthalmol 2011; 21: 811–819.
Holland GN . Ocular toxoplasmosis: the influence of patient age. Mem Inst Oswaldo Cruz 2009; 104: 351–357.
Garweg JG, Scherrer JN, Halberstadt M . Recurrence characteristics in European patients with ocular toxoplasmosis. Br J Ophthalmol 2008; 92: 1253–1256.
Tugal-Tutkun I, Corum I, Otuk B, Urgancioglu M . Active ocular toxoplasmosis in Turkish patients: a report on 109 cases. Int Ophthalmol 2005; 26: 221–228.
Aleixo AL, Benchimol EI, Neves ES, Silva CS, Coura LC, Amendoeira MR . Frequency of lesions suggestive of ocular toxoplasmosis among a rural population in the State of Rio de Janeiro. Rev Soc Bras Med Trop 2009; 42: 165–169.
Scherrer J, Iliev ME, Halberstadt M, Kodjikian L, Garweg JG . Visual function in human ocular toxoplasmosis. Br J Ophthalmol 2007; 91: 233–236.
Dodds EM, Holland GN, Stanford MR, Yu F, Siu WO, Shah KH et al. Intraocular inflammation associated with ocular toxoplasmosis: relationships at initial examination. Am J Ophthalmol 2008; 146: 856–865.
Balasundaram MB, Andavar R, Palaniswamy M, Venkatapathy N . Outbreak of acquired ocular toxoplasmosis involving 248 patients. Arch Ophthalmol 2010; 128: 28–32.
Acknowledgements
This work was supported by a project (Grant no. III41019) from the Ministry of Education and Science of Serbia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kovačević-Pavićević, D., Radosavljević, A., Ilić, A. et al. Clinical pattern of ocular toxoplasmosis treated in a referral centre in Serbia. Eye 26, 723–728 (2012). https://doi.org/10.1038/eye.2012.20
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.20
Keywords
This article is cited by
-
Comparison between the areas of scarred and active toxoplasmic retinochoroiditis
Eye (2021)
-
Chorio-retinal toxoplasmosis: treatment outcomes, lesion evolution and long-term follow-up in a single tertiary center
International Ophthalmology (2020)
-
Assessment of ocular toxoplasmosis patients reported at a tertiary center in the northeast of Iran
International Ophthalmology (2018)