Abstract
Purpose
We evaluated the effects of intravitreal injection of bevacizumab (Avastin; Novartis, Basel, Switzerland) on blood pressure (BP) in the context of ocular vascular pathology.
Methods
This study retrospectively examined 135 consecutive patients treated with intravitreal injections of 1.25 mg bevacizumab for retinal vascular disease; there were 61 cases of diabetic retinopathy, 30 of retinal vein occlusion, 35 of choroidal neo-vascularization (CNV), and 9 of other retinal vascular diseases. BP was measured before injection and at 30 min, 1 day, 1 week, 3 weeks, and thereafter monthly over a 6-month period.
Results
In the CNV group, 30-min post-injection systolic values were significantly higher than baseline, and systolic and diastolic values after 1 day, 1 week, and 3 weeks were significantly lower than before injection. No other pressure measurement differed significantly from baseline values in the other groups.
Discussion
Intravitreal bevacizumab injection is safe in terms of its effect on BP, regardless of ocular pathology.
Similar content being viewed by others
Introduction
Bevacizumab (Avastin; Novartis, Basel, Switzerland) has shown efficacy in retinal vascular diseases, such as diabetic retinopathy (DR), retinal vascular occlusion (RVO), and choroidal neo-vascularization (CNV).1, 2, 3, 4 The pathologic mechanisms of these diseases differ in detail, but many studies have indicated that vascular endothelial growth factor (VEGF) has an important function in ocular neo-vascularization.5, 6 Data have been obtained implicating VEGF in the pathologic vascular growth seen in DR, retinal vein occlusion, iris neo-vascularization, and age-related macular degeneration (AMD).7, 8, 9, 10, 11
Although the specific mechanism is unknown, VEGF inhibition is known to induce hypertension- and hypertension-related systemic complications in patients. Intravitreal bevacizumab injection was introduced to avoid such systemic complications; however, ocular adverse reactions have been observed, including transiently elevated intraocular pressure (IOP) and endophthalmitis.12, 13 Systemic side effects were associated with the intravitreal injection of bevacizumab such as rise in blood pressure (BP), cerebrovascular accidents, myocardial infarction, transient ischemic attacks, and deep vein thrombosis.12, 13 A recent study found that bevacizumab treatment caused endothelial dysfunction and reduced the number of microvessels; these closely associated effects could be responsible for the increase in BP.14 We postulated that intravitreal bevacizumab injection might differentially influence BP, depending on the type of ocular pathology present, which might reflect differences in systemic disease and/or in the age of the affected patient populations.
Thus, this study retrospectively examined BP changes after intravitreal bevacizumab injection in patients with DR, RVO, CNV, and other retinal vascular disorders.
Materials and methods
Patients treated with intravitreal bevacizumab injection from May 2007 to February 2008 were included. We obtained informed consent for the administration of intravitreal bevacizumab injection from all participants, after giving them detailed information about the potential risks and benefits of the procedure, and the off-label nature of the treatment. Patients with known hypertension consulted with the staff in our department of cardiology, to verify their BP status before injection, and those with a history of cerebrovascular attack consulted with the staff in neurology. Exclusion criteria were as follows: patients using anti-glaucomatic agents, those earlier treated with vitrectomy, those with poorly controlled hypertension after consultation with a cardiologist, and those who did not complete their final follow-up. Patients with intravitreal injection of triamcinolone within earlier 4 months were excluded too. The study was approved by the local institutional review board. All procedures conformed to the Declaration of Helsinki for research involving human subjects.
The procedure was performed aseptically in an operating room. Lidocaine (4%) was administered topically for local anaesthesia, and 1.25 mg of bevacizumab was injected at the inferior temporal sclera (3.5 mm from the limbus) into the vitreous cavity, using a 30-gauge needle. The fundus was examined using an indirect ophthalmoscope to confirm the perfusion of the optic nerve head, and each patient was instructed to take an oral antibiotic (cefdinir), and to apply a topical antibiotic (levofloxacin) for 1 week post-operatively.
The patients were asked to rest in a comfortable sitting position for at least 5 min before measuring their systolic and diastolic BP before injection, and again at 30 min and 1 h after injection, using a BP-203RV III monitor (OMRON Healthcare Co. Ltd, Tokyo, Japan). Follow-up examinations were performed 1 day, 1 week, 3 weeks, 1 month, and then every month until 6 month-post-injection to measure BP in the same manner. Slit lamp and fundus examinations were performed at each visit.
To minimize the effect of diurnal variation on BP, baseline measurements were taken 1–2 h before the procedure, and the intravitreal bevacizumab injection and follow-up examinations were performed in the afternoon (1500 and 1700 hours).
Statistical analyses were performed using SPSS (Windows version 13.0, SPSS Inc., Chicago, IL, USA). One-way ANOVA was used to examine any differences in baseline characteristics among groups, and Wilcoxon's signed rank test was used to reveal any changes in systolic and diastolic BP after injection, relative to pre-injection baseline values. P-values <0.05 were deemed to indicate statistical significance. Where a patient received more than one injection, statistical analysis was limited to data from the eye receiving the first injection.
Results
Over a 6-month period, a total of 185 eyes in 135 patients seen in our department received intravitreal bevacizumab injection; of these, 50 patients (37%) received repeated injection in the same eye (14 patients) or in the other eye (36 patients) over a mean period of 2 months. Only the first eye injected per patient was used in the statistical analysis, so that 135 eyes in 135 patients were included in this study. These were divided into groups of DR, RVO, CNV, or other diseases (central serous chorioretinopathy, polypoidal choroidal vasculopathy, retinal angiomatous proliferation, etc). More specifically, bevacizumab was given for macular oedema (78.7%) and neo-vascularization (21.3%) in the DR group, 83.3 and 16.7% in the RVO group, respectively.
The basic characteristics of the patients did not differ significantly among groups, except in the presence of underlying hypertension and diabetes mellitus (Table 1). The incidence of hypertension was significantly lower in the CNV group, whereas that of diabetes was significantly higher in the DR group, relative to other groups (P<0.05).
The mean systolic and diastolic BP measured preoperatively was 132.57±17.17 and 80.59±11.43 mm Hg, respectively. There was no significant difference in mean baseline systolic or diastolic BP between the groups (systolic, P=0.14; diastolic, P=0.39; Tables 2 and 3).
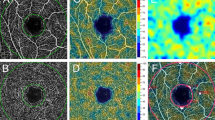
Mean systolic BP was increased significantly from baseline values at 30 min after intravitreal bevacizumab injection in the CNV group (P=0.023; Figure 1c). This group then showed significant decreases in systolic and diastolic BP from baseline values at 1 day (systolic, P=0.014; diastolic, P=0.005), 1 week (systolic, P=0.023; diastolic, P=0.001), and 3 weeks after injection (systolic, P=0.015; diastolic, P=0.001), but no significant change was found after 2 months (Figure 1c). None of the other groups showed any significant post-treatment change in BP (Figures 1a–d). No hypertensive crisis was reported in any of the groups during the 6-month follow-up period (Tables 2 and 3).
BP change in the DR group (a), the RVO group (b), the CNV group (c), and the group with other diseases (d), after a single 1.25 mg intravitreal injection of bevacizumab. The boxplot depicts the 50% interquartile range for BP among the patients. Error bars indicate SD. *Significant change, relative to baseline measurement (P<0.05).
Discussion
Recent studies have revealed the efficacy of intravitreal bevacizumab injection, which is widely used for many chorioretinal vascular disorders.1, 3, 4 Although many studies have investigated the elevation of IOP and BP after intravitreal bevacizumab,12, 13, 15, 16 none has evaluated its effects on BP in relation to the specific ocular pathology present. The mechanism by which inhibition of VEGF induces hypertension is unclear, but a recent study reported that endothelial dysfunction and capillary rarefaction are closely associated with the observed increase in BP.14 This led us to ask how bevacizumab injection influenced BP in patient groups with differing ocular pathologies, among whom both the presence of systemic disease and the mean age of patients might be expected to differ.
In this study, CNV group showed a significant increase in systolic BP at 30 min after intravitreal bevacizumab injection, followed by significant decreases in systolic and diastolic BP at follow-up visits from 1 day to 3 weeks after injection. There was no other significant change in BP after injection in the other groups. The change seen in the CNV group may have been due to diurnal physiological changes, or may have been a response to the easing of surgery-related stress, as reported by Kernt et al.15 The strict regulation of vascular tone by anti-hypertensive drugs in patients would be expected to reduce the chances of pre- or post-operative BP changes resulting from emotional stress, white coat syndrome, or diurnal variation. It might be suggested that the measured BP in the CNV group was more influenced by the factors mentioned above, relative to that seen in the other groups, because it included fewer hypertensive patients. This hypothesis can be supported by an earlier study reported by Lee et al,16 for which similar results were obtained from evaluating the changes in BP in patients with and without hypertension after intravitreal bevacizumab injection with the same population group.
Regardless, the initial increase of BP at 30 min after injection reported in the CNV group might reflect the emotional stress associated with the procedure rather than adverse effects of anti-VEGF therapy, because the maximal serum concentration of bevacizumab after intravitreal injection is reached at post-operative day 8, according to an animal study.17 Although it is difficult to directly compare the pharmacokinetics of bevacizumab seen in rabbit model with that in human beings, it is suspected that systemic exposure may be less in human beings because of their larger serum compartment.17 The pharmacokinetic data of serum concentration of bevacizumab after intravitreal injection from two hypertensive patients were reported, and peak serum levels of bevacizumab were 86.5 and 59.8 ng/ml at post-injection hours 120 and 168, respectively.18 Taken these together, the increase in the 30-min systolic BP values was probably not because of the adverse effects of anti-VEGF therapy.
Limitations of this study include the relatively small sample size and the use of single BP measurement. Ambulatory BP monitoring has been proved to be clinically superior, compared with single sphygmomanometric measurements. However, the use of ambulatory BP monitoring to detect a rise after intravitreal bevacizumab injection is not practical and convenient for patients, considering that Mourad et al14 recently reported that a significant increase in BP after systemic bevacizumab treatment (mean cumulative dose: 3.16 g) is known to occur after 6 months because of microvascular rarefaction and inhibition of NO pathway. Importantly, our results are similar to those of an earlier study using devices for automatic 24-h recording of circadian BP after intravitreal bevacizumab injection.18 BP shows high intra- and interindividual variability, as well as diurnal changes.19 In this study, baseline measurements were taken 1–2 h before the procedure, and follow-up examinations were performed in the afternoon, to minimize the effect of diurnal variation on BP.
It would have been very useful to analyse any differences in BP patterns of change according to CNV pathology and a diagnosis of hypertension. As risk factors of AMD include age and cardiovascular risk factor, the basic characteristics of patients with CNV caused by AMD would be different from that of patients with CNV secondary to other diseases. Taken these facts into account in the analysis, the results would have been different. However, the number of patients in this study may still be too small to obtain any statistically meaningful results by such an analysis. Further studies with a larger sample size are needed to clarify this matter.
In conclusion, we have shown that intravitreal bevacizumab injection seems to be safe in terms of its effect on BP, regardless of ocular pathology.

References
Arevalo JF, Fromow-Guerra J, Quiroz-Mercado H, Sanchez JG, Wu L, Maia M et al. Primary intravitreal bevacizumab (Avastin) for diabetic macular edema. Ophthalmology 2007; 114: 743–750.
Michels S, Rosenfeld PJ, Puliafito CA, Marcus EN, Venkatraman AS . Systemic bevacizumab (Avastin) therapy for neovascular age-related macular degeneration. Ophthalmology 2005; 112: 1035–1047.
Rich RM, Resenfeld PJ, Puliafito CA, Dubovy SR, Davis JL, Flynn Jr HW et al. Short-term safety and efficacy of intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Retina 2006; 26: 495–511.
Gündüz K, Bakri SJ . Intravitreal bevacizumab for macular edema secondary to branch retinal vein occlusion. Eye 2008; 22: 1168–1171.
Tolentino MJ, Miller LW, Gragoudas ES, Jakobiec FA, Flynn E, Chatzistefanou K et al. Intravitreal injections of vascular endothelial growth factor produce retinal ischemia and microangiopathy in an adult primate. Ophthalmology 2006; 103: 1820–1828.
Tolentino MJ, Miller JW, Gragoudas ES, Chatzistefanou K, Ferrara N, Adamis AP . Vascular endothelial growth factor is sufficient to produce iris neovascularization and neovascular glaucoma in a nonhuman primate. Arch Ophthalmol 1996; 114: 964–970.
Adamis AP, Miller JW, Bernal MT, D’Amico DJ, Folkman J, Yeo TK et al. Increased vascular endothelial growth factor levels in the vitreous of eyes with proliferative diabetic retinopathy. Am J Ophthalmol 1994; 118: 445–450.
Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 1994; 331: 1480–1487.
Pe’er J, Shweiki D, Itin A, Hemo I, Gnessin H, Keshet E . Hypoxia-induced expression of vascular endothelial growth factor by retinal cells is a common factor in neovascularizing ocular diseases. Lab Invest 1995; 72: 638–645.
Lopez PF, Sippy BD, Lambert M, Thach AB, Hinton DR . Transdifferentiated retinal pigment epithelial cells are immunoreactive for vascular endothelial growth factor in surgically excised age-related macular degeneration-related membranes. Invest Ophthalmol Vis Sci 1996; 37: 855–868.
Kvanta A, Algvere PV, Berglin L, Seregard S . Subfoveal fibrovascular membranes in age-related macular degeneration express vascular endothelial growth factor. Invest Ophthalmol Vis Sci 1996; 37: 1929–1934.
Wu L, Martínez-Castellanos MA, Quiroz-Mercado H, Arevalo JF, Berrocal MH, Farah ME et al. Twelve-month safety of intravitreal injections of bevacizumab (Avastin): results of the Pan-American Collaborative Retina Study Group (PACORES). Graefes Arch Clin Exp Ophthalmol 2008; 246: 81–87.
Fung AE, Rosenfeld PJ, Reichel E . The international intravitreal bevacizumab safety survey: using the internet to assess drug safety worldwide. Br J Ophthalmol 2006; 90: 1344–1349.
Mourad JJ, des Guetz G, Dabbabi H, Levy BI . Blood pressure rise following angiogenesis inhibition by bevacizumab. A crucial role for microcirculation. Ann Oncol 2008; 19: 927–934.
Kernt M, Neubauer AS, Kampik A . Intravitreal bevacizumab (Avastin) treatment is safe in terms of intraocular and blood pressure. Acta Ophthalmol Scand 2007; 85: 119–120.
Lee K, Yang H, Lim H, Lew HM . A prospective study of blood pressure and intraocular pressure changes in hypertensive and nonhypertensive patients after intravitreal bevacizumab injection. Retina 2009; 29: 1409–1417.
Bakri SJ, Snyder MR, Reid JM, Pulido JS, Singh RJ . Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology 2007; 114: 855–859.
Ziemssen F, Zhu Q, Peters S, Grisanti S, El Wardani M, Szurman P et al. Intensified monitoring of circadian blood pressure and heart rate before and after intravitreous injection of bevacizumab: preliminary findings of a pilot study. Int Ophthalmol 2009; 29: 213–224.
Ceyhan M, Gunaydin S, Yorgancioglu C, Zorlutuna Y, Uluoglu C, Zengil H . Comparison of circadian rhythm characteristics of blood pressure and heart rate in patients before and after elective coronary artery bypass surgery. Chronobiol Int 2003; 20: 337–349.
Acknowledgements
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/zhAJMj.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chung, YR., Lee, K., Cho, EH. et al. Blood pressure changes after intravitreal bevacizumab in patients grouped by ocular pathology. Eye 24, 1320–1324 (2010). https://doi.org/10.1038/eye.2010.22
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.22
Keywords
This article is cited by
-
The ideal intravitreal injection setting: office, ambulatory surgery room or operating theatre? A narrative review and international survey
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)



