Abstract
Purpose:
To acquire high definition spectral domain optical coherence tomography (SD-OCT) images of supine, non-anesthetized infants in the office by a novel modification of a commercially available table-top, chin rest system.
Method:
Spectralis, a combined HRA+OCT device (Heidelberg Engineering, Heidelberg, Germany) was modified to convert the table-top system into a hand-held device using a two-step modification of the existing system. This device was used to obtain high-resolution OCT images of four infants with aggressive posterior retinopathy of prematurity (APROP) who required no general anesthesia.
Results:
Serial imaging at two time periods of the exact area of clinical interest were obtained and were comparable. The entire procedure was safely completed in the office. The obtained OCT images guided selective laser ablation of flat neovascularization which were missed on clinical examination.
Conclusion:
With this simple modification and technique, the ability of using the Spectralis, a popular combined angiography and OCT imaging device for imaging supine, non-anesthetized infants has been established. This possibility would allow the dual use of the table-top system to serve also as a hand-held device for paediatric cases that can be imaged in the office setting with limited operating room facility in a busy practice.
Similar content being viewed by others
Introduction
Despite the recent introduction of a hand-held non-contact optical coherence tomography (OCT) system to image the infant retina,1 OCT imaging of infants has been limited chiefly because of the fact that most commercially available machines are vertically oriented and disallow imaging of supine, non-anaesthetized, and uncooperative children.2, 3, 4, 5 Using a novel modification, we show how the disassembled vertical camera unit of the Spectralis (HRA+OCT; Heidelberg Engineering, Heidelberg, Germany) allows high-definition spectral-domain (SD) OCT images in four cases of supine premature infants.
Following a two-step disassembly, the freed camera is pointed downwards in alignment with the infant's eye (Figure 1). The retina is brought to focus on the infrared (IR) window and the corresponding OCT images are acquired. The retinal periphery is imaged by tilting the camera head. The resulting laterally inverted images must be considered in reporting the localization of the pathology. Four cases of aggressive posterior retinopathy of prematurity (APROP) underwent OCT imaging using the above technique. Two cases are detailed here.
The disassembled Spectralis imaging system converting the table-top chin-rest system into a mobile hand-held device is demonstrated. The infant is placed on a table adjoining the system in the office room and can be imaged without the use of general anaesthesia. As the infant's head is closer to the camera head and the technician stands at the head end of the infant, the resulting images are laterally inverted and must be kept in mind while interpreting localisation.
Case reports
Case 1
A female infant born at 2000 g and 32 weeks gestation diagnosed with aggressive posterior retinopathy of prematurity (APROP) had undergone laser photocoagulation at a post-conceptual age of 38+2 weeks. A week later, media haze from recent laser prevented accurate localization of the persistent flat neovascularization (FNV) in the left eye. Spectral-domain optical coherence tomography (SD-OCT) images, however, confirmed and localized the FNV, which allowed selective laser ablation of these vessels.6 A week later, the resolution of the FNV was confirmed on repeat OCT of the same site, corroborated on clinical examination and Retcam images (RETCAM Shuttle, Clarity MSI, CA, USA) (Figures 2 and 3).
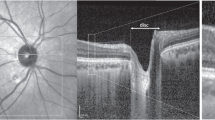
An infant (Case 1) with aggressive posterior retinopathy of prematurity (APROP) imaged on the Spectralis using the modified technique. A composite of the left eye temporal quadrant imaged with a Retcam (above), and infrared and spectral-domain OCT images (below) was imaged 5 days after the initial laser photoablation for APROP. The red circle shows the area of suspected flat neovascularization (FNV), which was confirmed on the OCT (blue arrow). The OCT reveals increased retinal thickness underlying and adjoining the FNV, suggestive of retinal oedema. The laterally inverted OCT as noted must be kept in mind while interpreting the localisation. The color reproduction of this figure is available on the html full text version of the manuscript.
A composite of the same case as in Figure 2 (Case 1), showing the resolution of the flat neovascularization (FNV) from the same location (red circle) imaged by the Spectralis OCT (below) and corroborated with the Retcam image (above). This image was obtained 7 days after the first session, and the eye had undergone supplement laser over the FNV based on the OCT findings in Figure 2. There is resolution of retinal oedema compared to Figure 2. The color reproduction of this figure is available on the html full text version of the manuscript.
Case 2
A male infant born at 1300 g and 30 weeks gestation underwent similar SD-OCT-assisted selective laser photoablation of the FNV a week after the initial treatment (Figures 4 and 5).
Case 2: The composite of the left eye of Case 2, imaged 6 days after laser photoablation for APROP. The Retcam image above indistinctly shows (red circle) the area of the persistent flat neovascularization (FNV), which was more clearly shown on the infrared window and the optical coherence tomography (OCT) (blue arrow) on the Spectralis using the modified technique. The laterally oriented (inverted) OCT image is a result of the technique described and does not hinder visualisation. The color reproduction of this figure is available on the html full text version of the manuscript.
Case 2: The composite of the same eye of Case 2, imaged 10 days later, showing the resolution of the FNV (red circle) from the same location as in Figure 4, imaged on an optical coherence tomography (OCT) on the Spectralis. The Retcam image shows healing laser scars and a clearer media than before. Selective laser ablation of the FNV was possible owing to the accurate localisation on the OCT. The color reproduction of this figure is available on the html full text version of the manuscript.
Discussion
This report establishes that the Spectralis, a table-top system, can also be modified to serve as a hand-held device for imaging supine, non-anaesthetized infants in the office setting, obviating the need of general anaesthesia or an operating room. Moreover, the Spectralis has the capability of performing combinations of fluorescein and indocyanine green angiography simultaneously, which may be explored in the future for paediatric cases. In this report, the four cases imaged using this method benefitted from the rapid and high-resolution OCT images, which allowed targeted therapeutic intervention. Its utility in routine retinopathy of prematurity cases and other paediatric retinal conditions needs further investigation.

Conflict of interest
The authors declare no conflict of interest.
References
Scott AW, Farsiu S, Enyedi LB, Wallace DK, Toth CA . Imaging the infant retina with a hand-held spectral-domain optical coherence tomography device. Am J Ophthalmol 2009; 147: 364–373.
Shields CL, Mashayekhi A, Luo CK, Materin MA, Shields JA . Optical coherence tomography in children: analysis of 44 eyes with intraocular tumors and simulating conditions. J Pediatr Ophthalmol Strabismus 2004; 41: 338–344.
Joshi MM, Trese MT, Capone A . Optical coherence tomography findings in stage 4A retinopathy of prematurity: a theory for visual variability. Ophthalmology 2006; 113: 657–660.
Harris PD, Farmery AD, Patel CK . The challenges of positioning an infant undergoing optical coherence tomography under general anaesthesia. Paediatr Anaesth 2009; 19 (1): 64–65.
Patel CK . Optical coherence tomography in the management of acute retinopathy of prematurity. Am J Ophthalmol 2006; 141: 582–584.
Vinekar A, Trese MT, Capone Jr A, Photographic Screening for Retinopathy of Prematurity (PHOTO-ROP) cooperative Group. Evolution of retinal detachment in posterior retinopathy of prematurity: impact on treatment approach. Am J Ophthalmol 2008; 145 (3): 548–555.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vinekar, A., Sivakumar, M., Shetty, R. et al. A novel technique using spectral-domain optical coherence tomography (Spectralis, SD-OCT+HRA) to image supine non-anaesthetized infants: utility demonstrated in aggressive posterior retinopathy of prematurity. Eye 24, 379–382 (2010). https://doi.org/10.1038/eye.2009.313
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.313
Keywords
This article is cited by
-
Evaluation of the Returned Electromagnetic Signal from Retro-reflectors in Turbid Media
Scientific Reports (2019)
-
Update on the Intraoperative OCT: Where Do We Stand?
Current Ophthalmology Reports (2018)
-
Retinopathy of Prematurity in a Rural Neonatal Intensive Care Unit in South India—A Prospective Study
The Indian Journal of Pediatrics (2012)