Abstract
Background/Objectives:
Nutritional status has been shown to affect quality of life, tolerance of future treatments and survival in people having undergone major upper gastrointestinal surgery. The objective of this trial was to assess the impact of intense individualized dietary advice following major upper gastrointestinal surgery on nutritional status, dietary intake, gastrointestinal symptoms and quality of life, compared to the current usual care.
Subjects/Methods:
On discharge from hospital, people having had major upper gastrointestinal surgery were randomized to have dietetic follow-up fortnightly for 6 months or to a control group. Data collection was conducted at baseline, and at 1, 3 and 6 months.
Results:
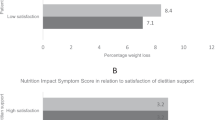
Twenty-seven people were randomized to either the intervention or control group. There was a small but non-significant difference in percent weight loss in the intervention (−0.8±8.8) compared to the control group (−2.7±9.7) at 6 months. There were no other differences between the two groups.
Conclusions:
This small study did not demonstrate that intense individualized dietary advice leads to improvements in nutritional status and quality of life for people having had major upper gastrointestinal surgery. The study does highlight that this group is at high nutritional risk, and does support the need for a larger multicentre study.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Martin L, Lagergren P . Long-term weight change after oesophageal cancer surgery. Brit J Surg 2009; 96: 1308–1314.
Carey S, Storey D, Biankin AV, Martin D, Young J, Allman-Farinelli M . Long term nutritional status and quality of life following major upper gastrointestinal surgery: A cross-sectional study. Clin Nutr 2011; 30: 774–779.
Bae J, Kim S, Kim Y, Ryu KW, Lee JH, Noh JH et al. Health-related quality of life among disease-free stomach cancer survivors in Korea. Qual Life Res 2006; 15: 1587–1596.
Conroy T, Uwer L, Deblock M . Health-related quality-of-life assessment in gastrointestinal cancer: are results relevant for clinical practice? Curr Opin Oncol 2007; 19: 401–406.
Huang JJ, Yeo CJ, Sohn TA, Lillemoe KD, Sauter PK, Coleman J et al. Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg 2000; 231: 890–898.
Senesse P, Assenat E, Schneider S, Chargari C, Magne N, Azria D et al. Nutritional support during oncologic treatment of patients with gastrointestinal cancer: who could benefit? Cancer Treat Rev 2008; 34: 568–575.
Yu W, Seo Y, Chung H . Postoperative body weight loss and survival after curative resection for gastric cancer. Brit J Surg 2002; 89: 467–470.
Carey S, He L, Ferrie S . Nutritional management of patients undergoing major upper gastrointestinal surgery: a survey of current practice in Australia. Nutr Diet 2010; 67: 219–223.
Carey S, Ferrie S, Young J, Allman-Farinelli M . Long-term nutrition support in gastrointestinal disease—A systematic review of the evidence. Nutrition 2012; 28: 4–8.
Norman K, Pirlich M, Smoliner C, Kilbert A, Schulzke JD, Ockenga J et al. Cost-effectiveness of a 3-month intervention with oral nutritional supplements in disease-related malnutrition: a randomised controlled pilot study. Eur J Clin Nutr 2011; 65: 735–742.
Copland L, Liedman B, Rothenberg E, Bosaeus I . Effects of nutritional support long time after total gastrectomy. Clin Nutr 2007; 26: 605–613.
Detsky A, McLaughlin J, Baker J, Johnston N, Whittaker S, Mendelson Ra et al. What is subjective global assessment of nutritional status? J Parenter Enteral Nutr 1987; 11: 8–13.
Guenther PM, De Maio TJ, Ingwersen LA, Berlin M . The multiple-pass approach for the 24-hour recall in the Continuing Survey of Food Intakes by Individuals (CSF11) 1994–1996. Presented at the International Conference on Dietary Assessment Methods. Mass: Boston, 1995.
Johnson RK, Driscoll P, Goran MI . Comparison of multiple-pass 24-hour recall estimates of energy intake with total energy expenditure determined by the doubly labeled water method in young children. J Am Diet Assoc 1996; 96: 1140–1144.
Schoeller DA . How accurate is self-reported dietary energy intake? Nutr Rev 1990; 48: 373–379.
Schofield WN . Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 1985; 39 (Suppl 1), 5–41.
World Health Organization. Energy and protein requirements. Report of a joint FAO/WHO/UNU Expert Consultation. World Health Organization Technical Report Series 1985; 724: 1–206.
Barak N, Wall-Alonso E, Sitrin MD . Evaluation of stress factors and body weight adjustments currently used to estimate energy expenditure in hospitalized patients. J Parenter Enteral Nutri 2002; 26: 231–238.
Ferrie S, Ward M Back to Basics: Estimating Energy Requirements for Adult Hospital Patients. Blackwell Publishing: Asia, 2007; 192–199.
Revicki DA, Wood M, Wiklund I, Crawley J . Reliability and validity of the gastrointestinal symptom rating scale in patients with gastroesophageal reflux disease. Qual Life Res 1997; 7: 75–83.
Olsson U, Bosaeus I, Svedlund J, Bergbom I . Patients' subjective symptoms, quality of life and intake of food during the recovery period 3 and 12 months after upper gastrointestinal surgery. Eur J Cancer Care 2007; 16: 74–85.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993; 85: 365–376.
Ryan AM, Rowley SP, Healy LA, Flood PM, Ravi N, Reynolds JV . Post-oesophagectomy early enteral nutrition via a needle catheter jejunostomy: 8-year experience at a specialist unit. Clin Nutr 2006; 25: 386–393.
Hyltander A, Bosaeus I, Svedlund J, Liedman B, Hugosson I, Wallengren O et al. Supportive nutrition on recovery of metabolism, nutritional state, health-related quality of life, and exercise capacity after major surgery: a randomized study. Clin Gastroenterol Hepatol 2005; 3: 466–474.
Rutishauser IH . Dietary intake measurements. Public Health Nutr 2005; 8: 1100–1117.
De Castro JM . Eating behavior: lessons from the real world of humans. Nutrition 2000; 16: 800–813.
Tracey E, Alam N, Chen W, Bishop J ‘Cancer in New South Wales: Incidence and Mortality Report.’. Cancer Institute of New South Wales, New South Wales Health: Sydney, 2006.
Carey S, Young JM, M Allman-Farinelli . Food and nutrient intake among people following major upper gastrointestinal surgery. Food Nutr Sci 2012; 3: 1004–1008.
Subar AF, Thompson FE, Potischman N, Forsyth BH, Buday R, Richards D et al. Formative research of a quick list for an automated self-administred 24-hour dietary recall. J Am Diet Assoc 2007; 107: 1002–1007.
Martin L, Jia C, Rouvelas I, Lagergren P . Risk factors for malnutrition after oesophageal and cardia cancer surgery. Brit J Surg 2008; 95: 1362–1368.
Carey S, Laws R, Young J, Allman-Farinelli M . Struggling with life after major upper gastrointestinal surgery—a qualitative study. Qual Health Res. in press.
Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P et al. ESPEN Guidelines on Enteral Nutrition: surgery including organ transplantation. Clin Nutr 2006; 25: 224–244.
Bae J, Park J, Yang H, Kim J . Nutritional status of gastric cancer patients after total gastrectomy. World J Surg 1998; 22: 254–260.
Scholmerich J . Postgastrectomy syndromes—diagnosis and treatment. Best Pract Res Clin Gastroenterol 2004; 18: 917–933.
Scottish Intercollegiate Guidelines Network (SIGN). Management of Oesophageal and Gastric Cancer. A national clinical guideline: Edinburgh, Scotland, 2006.
Acknowledgements
We would like to thank the upper gastrointestinal surgeons Royal Prince Alfred Hospital for allowing their patients to be recruited into this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions: All authors have contributed to the paper. SC conceived and designed the research, collected the data, analyzed the results and drafted the manuscript. SF was involved in analysis and interpretation of data and manuscript preparation. RR conducted the nutrition intervention. JB contributed to data collection. MA-F and JY were involved in the design of the research, analysis and interpretation of results and manuscript preparation.
Rights and permissions
About this article
Cite this article
Carey, S., Ferrie, S., Ryan, R. et al. Long-term nutrition intervention following major upper gastrointestinal surgery: a prospective randomized controlled trial. Eur J Clin Nutr 67, 324–329 (2013). https://doi.org/10.1038/ejcn.2013.17
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2013.17
Keywords
This article is cited by
-
Using intervention mapping to develop an outpatient nursing nutritional intervention to improve nutritional status in undernourished patients planned for surgery
BMC Health Services Research (2020)
-
Oral nutrition interventions in patients undergoing gastrointestinal surgery for cancer: A systematic literature review
Supportive Care in Cancer (2020)
-
Changes in the nutritional status of elderly patients after esophagectomy
Esophagus (2019)