Abstract
Because of their unique properties, multipotent mesenchymal stem cells (MSCs) represent one of the most promising adult stem cells being used worldwide in a wide array of clinical applications. Overall, compelling evidence supports the long-term safety of ex vivo expanded human MSCs, which do not seem to transform spontaneously. However, experimental data reveal a link between MSCs and cancer, and MSCs have been reported to inhibit or promote tumor growth depending on yet undefined conditions. Interestingly, solid evidence based on transgenic mice and genetic intervention of MSCs has placed these cells as the most likely cell of origin for certain sarcomas. This research area is being increasingly explored to develop accurate MSC-based models of sarcomagenesis, which will be undoubtedly valuable in providing a better understanding about the etiology and pathogenesis of mesenchymal cancer, eventually leading to the development of more specific therapies directed against the sarcoma-initiating cell. Unfortunately, still little is known about the mechanisms underlying MSC transformation and further studies are required to develop bona fide sarcoma models based on human MSCs. Here, we comprehensively review the existing MSC-based models of sarcoma and discuss the most common mechanisms leading to tumoral transformation of MSCs and sarcomagenesis.
Similar content being viewed by others
Introduction
Multipotent mesenchymal stem cells (MSCs), also called bone marrow (BM) stromal cells or skeletal stem cells, are multipotent cells that represent a rare subset of BM cells and constitute a source of progenitors for mesodermic tissues1. To date, the developmental origin and the histological localization of the more immature population of MSCs remain elusive and likewise, a reliable specific marker to define this population has not yet been identified. The International Society for Cellular Therapy proposed a minimal set of criteria to define the ex vivo MSC cultures: (i) the cells must be plastic adherent when maintained in standard culture conditions, (ii) they must express CD105, CD73 and CD90 and lack expression of CD45, CD34, CD14, CD11b, CD79b, CD19 and HLA-DR and (iii) they must be able to differentiate into osteoblasts, adipocytes and chondroblasts in vitro2. In addition to BM, cells fulfilling these properties are present in a variety of tissues during development and therefore can be isolated from several embryonic and adult tissues including adipose tissue, umbilical cord, liver or muscle3,4,5. The exact nature and localization of MSCs in vivo remain poorly understood but increasing evidence indicates that MSC precursors from different tissues could have a perivascular distribution6. Interestingly, in vivo transplantation has been proposed as a surrogate assay to address the multipotent differentiation ability of the stromal cells derived from different tissues7. In fact, this in vivo approach has already revealed differences in the differentiation potential of MSCs derived from BM and other tissues. While more accurate methods to derive and characterize MSC cultures are being developed, the prevailing consensus is that unfractionated populations of MSCs contain subpopulations spanning different stages of mesodermal development with distinct potency ranging from multilineage stem cells to unilineage precursors or even fully differentiated cells. Thus, cultures are heterogeneous in potency and it is likely that only a small MSC subset represents the bona fide multipotent stem cell population.
The potential of MSCs for cell-based therapies relies on several key properties: (i) capacity to differentiate into several cell lineages; (ii) lack of immunogenicity; (iii) immunomodulatory properties; (iv) robust ex vivo expansion potential; (v) ability to secrete factors, which regulate cell proliferation, differentiation and migration and; (vi) homing ability to damaged tissues and tumor sites8. Due to these properties, MSCs are being used worldwide in a variety of clinical applications including tissue repair, treatment of graft-versus-host disease and autoimmune diseases and are being used as vehicles to deliver anti-cancer therapies8.
Nevertheless, recent evidence has revealed a link between MSCs and cancer. MSCs have been reported to inhibit or promote tumor growth depending on yet undefined conditions9. Likewise, the tumoral transformation of MSCs by different mechanisms gives rise to the formation of sarcomas in vivo, hence placing MSCs as the most likely cell of origin for certain sarcomas10. Sarcomas comprise a heterogenous group of malignant tumors of mesenchymal origin that were historically grouped according to the tumor location into two main types: soft tissue sarcoma (STS) and primary bone sarcoma11. An alternative genetic-based classification of sarcomas evolved upon the subsequent identification of molecular and genetic alterations associated with specific histological subtypes of sarcomas. According to this classification, sarcomas fall into two main categories. One group, including alveolar rhabdomyosarcoma (ARMS), myxoid liposarcoma (MLS), Ewing's sarcoma and synovial sarcoma, is characterized by the presence of tumor-specific translocations while the other group, represented by leiomyosarcoma, malignant fibrous histiocytoma (MFH) and osteosarcoma, is characterized by complex karyotypes indicative of severe genetic and chromosomal instability12.
In the hierarchical model for cancer genesis it is hypothesized that different cells within the tumor have distinct potential to initiate and maintain a tumor, and that there exist a rare subset of so-called cancer stem cells (CSCs) capable of long-term tumor maintenance. These CSCs have been recently identified in several types of tumors and are thought to be the only cells within the bulk tumor with the ability to reinitiate and maintain tumor growth13. Likewise, there are cell types susceptible of acquiring early cancer-initiating mutation(s), which eventually result in de novo tumor formation. The cell-of-origin or tumor-initiating cell (TIC) is not necessarily the CSC since the TIC and CSC concepts refer to cancer-initiating cells and cancer-propagating cells, respectively14. In this regard, increasing evidence suggests that MSCs might be the TIC capable of initiating sarcomagenesis. Thus, several types of human sarcomas have been reproduced in vivo upon the overexpression of specific fusion oncoproteins or disruption of key signaling pathways in MSCs. Likewise, there are also studies supporting that sarcomas could represent good examples of the CSC model and that these sarcoma CSCs display MSC properties. Therefore, the development of human sarcoma models based on experimentally induced transformation of MSCs will constitute an unprecedented system in the search for target-specific therapies against sarcomas. Here, we review the existing models of sarcomas based on transformed MSCs.
Tumoral transformation of MSCs
It has been recently established that transformed MSCs may initiate sarcomagenesis in vivo. Many efforts have been directed to characterize the transformation process and also to prospectively generate specific models for different sarcomas. These studies include both spontaneous and induced transformation of MSCs mediated by specific alterations affecting key signaling pathways such as the cell cycle control.
Spontaneous transformation of MSCs
Mouse MSCs
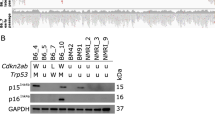
Mouse MSCs (mMSCs) are especially predisposed to acquiring transformation events after long-term in vitro culture favoring clonal selection of transformed cells15,16,17,18,19 (Table 1). Upon inoculation into immunodeficient mice, spontaneously transformed mMSCs promote the formation of sarcomas resembling the histopathological properties of fibrosarcoma15,16 and osteosarcoma17,18. In these reports, the transformation of mMSCs was associated with the accumulation of chromosome instability16,17,18,19, p53 mutations15 or loss of CDKN2A/p1617, highlighting the importance of a tight cell cycle control in MSC homeostasis.
Human MSCs
More importantly, in the human setting, the ex vivo expansion of human MSCs (hMSCs) is a pre-requisite for using these cells in some clinical applications. Consequently, the possibility that hMSCs may also undergo spontaneous transformation after long-term in vitro culture became a concern, which has drawn especial attention in recent years. One group described the outgrowth of a cell population with a transformed phenotype derived from normal BM-hMSC cultures, although the authors could not rule out the presence of a rare CD133+ non-stromal cell population in the starting material20 (Table 1). Likewise, it is worth mentioning that two other comprehensive studies initially reporting spontaneous transformation of both BM-hMSCs and human adipose-derived mesenchymal stem cells (hASCs) after long-term in vitro culture have been recently retracted due to cross-contamination of the MSC cultures with cancer cell lines21,22. On the other hand, many other authors have reported a lack of hMSC transformation after extensive in vitro culture23,24,25,26,27,28. These studies show that the life span of hMSCs is donor dependent and that cultures regularly become senescent after 15 to 25 passages. Likewise, no chromosomal abnormalities are normally detected by array-CGH and cytogenetic analysis23, although in some preparations of clinical-grade hMSCs the occurrence of donor-associated aneuploidy without transformation was observed28. Altogether, these studies strongly suggest that ex vivo expanded hMSC cultures are genetically stable with no solid evidence of in vitro spontaneous transformation, thus supporting the safe use of hMSCs in clinical applications.
Cell cycle control in MSC-based sarcoma modeling
Cell cycle checkpoints play a crucial role in maintaining the cellular homeostasis and either gain- or loss-of-function mutations affecting cell cycle regulators are often associated with sarcoma development12.
mMSCs
In the mouse setting, the use of genetically targeted mMSCs has demonstrated how the deficiency of different cell cycle regulators, especially p53, triggers a transformation process in mMSCs resulting in the generation of sarcoma29,30,31 (Table 2). For instance, in contrast to wild-type (wt) ASCs, p53-depleted mASCs were capable of originating leiomyosarcoma-like tumors after injection into immunodeficient mice31. This finding is further supported by a differentiation-based microRNA study, which has identified leiomyosarcoma as an MSC-related malignancy32. Another study has shown that the complete loss of p53 expression in p21−/−p53+/− mASCs after long-term culture induces cell growth, karyotypic instability and loss of p16INK4A which prevents senescence, resulting in the formation of fibrosarcoma-like tumors in vivo30. Similarly, alterations in other cell cycle regulators such as p16INK4A or p19ARF have also been detected during the process of MSC transformation17,30 whereas overexpression of c-MYC in p16INK4A−/−p19ARF−/− BM-mMSCs results in osteosarcoma development accompanied by loss of adipogenesis33. Importantly, the loss of other cell cycle regulators such as Rb does not transform mMSCs but its deficiency potentiates tumor development of p53-deficient mMSCs, generating more undifferentiated sarcomas31.
Mouse models
Several groups have also developed useful genetically engineered mouse models of sarcomagenesis based on the inactivation of p53 and/or Rb specifically in the osteoblastic lineage34,35. These studies not only confirm that sarcoma development is dependent on the loss of p53 and potentiated by the loss of Rb but also that these tumors display many of the features of human osteosarcomas, linking the inactivation of p53 and/or Rb in a committed mesenchymal lineage to osteosarcoma development. Similar results were shown in another mouse model in which p53 and Rb were inactivated in early mesenchymal tissues of embryonic limb buds36. In this study, mice carrying a p53 deletion developed different types of sarcomas, with osteosarcoma being the most common one. Interestingly, although Rb-deficient mice develop normally, Rb deficiency synergizes with p53 deletion to accelerate sarcoma formation and increase the frequency of poorly differentiated sarcomas. In other mouse models where mutations are restricted to muscle or uterus by local delivery of the Cre recombinase, the expression of oncogenic K-RAS or the mutation of endogenous K-RAS is needed to efficiently induce sarcoma formation in p53-deficient tissues37,38. Sarcomas developed in these models were characterized as pleomorphic rhabdomyosarcoma and high-grade sarcomas with myofibroblastic differentiation. Interestingly, deletion of the INK4A-ARF locus could substitute the p53 mutation in this K-RAS mutation-based model of sarcoma development37.
Human MSCs
Fortunately, hMSCs do not undergo malignant transformation as easily as mMSCs. For instance, opposite to mMSCs the inactivation of p53 or p53 and Rb does not induce transformation in hMSCs, although p53-/Rb-deficient hMSCs display a higher growth rate in vitro coupled to an extended lifespan39,40. In order to efficiently induce in vivo sarcomas from hMSCs, several non-physiological oncogenic events had to be combined41,42 (Table 2). Specifically, these oncogenic hits include the introduction of the catalytic subunit of the human telomerase (hTERT), HPV-16 E6 and E7 (which abrogate the functions of p53 and Rb family members), SV40 small T or large T antigens (which results in c-MYC stabilization and inactivates Rb and p53, respectively) and oncogenic H-RAS (which provides a constitutive mitogenic signal)41,42. In one of these models, the process of transformation of hMSCs is associated with a gradual increase in genomic hypomethylation, although this phenomenon is not necessary for transformation43. Using an alternative approach, another group succeeded in transforming hMSCs through ectopic expression of hTERT, H-RAS and BMI-1, which inhibits the expression of genes controlled by polycomb response elements including p16INK4A44. It was also reported that some hTERT-transduced hMSC lines lose contact inhibition, acquire anchorage-independent growth and form tumors in mice after long-term in vitro culture45. This transformation process was associated with the deletion of the Ink4a/ARF locus and with the acquisition of an activating mutation in K-RAS. Overall, in vivo tumors originated from most of these transformed hMSCs were classified as undifferentiated spindle cell sarcomas41,42,44.
Other signaling pathways involved in MSC transformation
Besides the inactivation of cell cycle regulators, the transformation process of hMSCs has been linked to alterations in signaling pathways such as PI3K-AKT and WNT signaling (Table 2).
PI3K-AKT pathway
The PI3K-AKT pathway is involved in cell survival and proliferation and is a downstream effector shared by different growth factor receptors abnormally activated in sarcomas, such as IGF1R, PDGFR or c-KIT receptor12. In this regard, it has been reported that the PI3K-AKT-mTOR signaling pathway plays a critical role in the development of leiomyosarcomas46. Thus, mice carrying a homozygous deletion of PTEN (a negative regulator of the PI3K-AKT pathway) in the smooth muscle lineage efficiently developed leiomyosarcoma46. The involvement of PTEN and PI3K-AKT in leiomyosarcoma is also implicated by the fact that these signaling pathways are dysregulated in leiomyosarcoma-forming p53-decifient mMSCs40.
WNT pathway
The WNT/β-catenin signaling pathway plays a central role in modulating the balance between self-renewal and differentiation in stem and progenitor cells47. In addition, WNT signaling also regulates the proliferation, differentiation and invasion capacity of hMSCs48,49. While these functions exerted by the WNT pathway may be useful in tissue regeneration, an aberrant or inadequate activation of this pathway may deregulate the balance between proliferation, differentiation and apoptosis, leading to malignant transformation. Accordingly, a recent study supports a role for aberrant β-catenin stabilization in the promotion of MSC-derived tumorigenesis50. In this work, the development of a mouse model harboring a targeted mutation in the APC gene provided evidence for the link between aggressive fibromatosis, a mesenchymal neoplasm, and MSCs. More importantly, inactivation of WNT signaling upon treatment of previously SV40-immortalized hMSCs with the WNT inhibitor DKK1 led to full malignant transformation of these hMSCs and the consequent in vivo formation of MFH51. Conversely, restoration of WNT signaling in MFH cells allowed them to differentiate along different mesenchymal lineages51. Furthermore, it was reported that key components of the Wnt signaling pathway are downregulated in osteosarcoma as compared to normal hMSCs and hMSCs differentiated into osteoblasts52. Interestingly, the role of WNT signaling in sarcomas seems to differ from its role in carcinomas because hMSC transformation and sarcomagenesis are associated with WNT signaling inhibition while different models of carcinomas are linked to activating mutations in components of the WNT pathway51.
The take-home messages from the aforementioned reports are as follows: (i) hMSCs do not seem to transform spontaneously during ex vivo expansion; (ii) mMSCs and mouse models highlight how the inactivation of key cell cycle regulators and/or alterations of other relevant signaling pathways induce the development of sarcomas from MSCs or their committed mesenchymal lineages; (iii) several cooperating oncogenic mutations have to work together in order to promote sarcoma development from difficult-to-transform hMSCs and; (iv) distinct cell populations at different developmental stages in the mesenchymal lineage hierarchy may serve as the cell of origin for different sarcoma subtypes.
Fusion gene-based models of sarcomas
The MSC origin of sarcomas characterized by the presence of tumor-specific fusion oncogenes as a result of chromosomal translocations has also been actively investigated and several types of tumors resembling human sarcomas have been reproduced in vivo upon the expression of sarcoma-specific fusion proteins in mMSCs and mouse models. Specifically, Ewing's sarcoma, MLS, ARMS and synovial sarcoma have been reproduced upon expression of EWS-FLI-1, FUS-CHOP, PAX-FKHR and SYT-SSX, respectively (Table 3).
Ewing's sarcoma MSC models
Ewing's sarcoma is a poorly differentiated tumor of uncertain histogenesis and aggressive biologic behavior. Two decades ago, the understanding of the biology of Ewing's sarcoma took a leap forward with the identification of recurrent EWS fusions, which drive oncogenesis in this disease53.
mMSCs
Two different groups have reported that the expression of EWS-FLI-1 in BM-mMSCs resulted in cell transformation and sarcoma development when implanted into immunodeficient mice54,55. These tumors shared some features with Ewing's sarcoma, including cell surface markers and cell morphology. Interestingly, the expression of EWS-FLI-1 was able to transform mMSCs on its own in one of the studies55 while secondary hits acquired in culture (i.e. p53 mutation) were required in another study54. Intriguingly, other Ewing's sarcoma-associated fusion genes such as EWS-ERG and FUS-ERG could not be stably expressed in mMSCs56.
Mouse models
Several knock-in and transgenic mouse models expressing EWS-FLI-1 or other Ewing's sarcoma-related fusion genes have been recently created57. The constitutive expression of EWS-FLI-1 has an embryonic lethal phenotype58. A tissue-specific cre-loxP-based strategy was thus used to achieve conditional expression of EWS-FLI-1 in vivo. Accordingly, mice with conditional expression of EWS-FLI-1 in primitive mesenchymal cells of the embryonic limb buds showed several developmental defects of the limbs but EWS-FLI-1 on its own was unable to induce formation of tumors in these mice58. However, when p53 was simultaneously deleted, EWS-FLI-1 promoted sarcoma formation. Thus, as aforementioned, conditional deletion of p53 in early mesenchymal tissues of embryonic limb buds predominantly gave rise to osteosarcomas36, and the presence of EWS-FLI-1 shifted the tumor phenotype towards more undifferentiated sarcomas, similar to Ewing's sarcoma58. Overall, similar to that observed in EWS-FLI-1-expressing hMSCs, additional cooperating mutations seem to be required for transformation in Ewing's sarcoma mouse models.
Human MSCs
In the human setting, EWS-FLI-1-expressing hMSCs failed to originate tumors when injected into immunodeficient mice,59 although the expression of EWS-FLI-1 in hMSCs induced a transcriptional expression pattern similar to that observed in human Ewing's sarcoma and upregulated the expression of CD99, a specific marker for Ewing's sarcoma59. The lack of transformation in this model underpins the need of yet undefined secondary cooperating mutations to transform hMSCs. The MSC origin for Ewing's sarcoma has been strengthened further in other experiments based on hMSCs. For instance, treatment of Ewing's tumor cell lines with specific EWS-FLI1 short hairpin RNAs shifted their gene expression profile towards that of normal MSCs60. In addition, CSCs displaying MSC properties have been identified in Ewing's sarcoma61. In a follow-up study, these authors showed that human pediatric, but not adult, MSCs expressing EWS-FLI-1 display in vitro features of Ewing's sarcoma CSCs62. This phenotype was due to the EWS-FLI-1-mediated repression of the miR-145 promoter, which, in turn, leads to the upregulation of embryonic stem cell transcription factors SOX2, OCT4 and NANOG, thus linking development, cell ontogeny and cancer.
MLS models
Liposarcomas are the most common type of STS, representing ∼20% of STS. Several types of liposarcoma are recognized, including well differentiated, dedifferentiated, myxoid, round cell and pleomorphic liposarcoma. MLS is characterized by the recurrent translocation t(12;16)(q13;p11), which fuses FUS to CHOP (also known as DDIT3) on chromosome 12. MLS has also been modeled by expressing of the FUS-CHOP fusion gene, which is found in > 90% of these tumors63.
mMSCs
Early in vitro approaches have shown the transforming effects of FUS-CHOP in NIH-3T3 fibroblasts64, but not in 3T3-L1 pre-adipocytes, suggesting that the transformation activity of FUS-CHOP is influenced by the cellular environment. More importantly, the expression of FUS-CHOP in both BM-mMSCs and mASCs gave rise to MLS-like tumors40,65. Nevertheless, in contrast to BM-mMSCs, secondary cooperating hits such as p53 deficiency are required for liposarcoma development from mASCs, suggesting that BM-mMSCs are more susceptible to FUS-CHOP-induced transformation and sarcomagenesis than mASCs. In the absence of FUS-CHOP, p53−/− mASCs originated leiomyosarcoma31, indicating that the expression of FUS-CHOP redirects the tumor genesis/phenotype40. These studies support the contention that the FUS-CHOP fusion is a critical event in MLS pathogenesis and that MSCs may represent the liposarcoma-initiating cell. Differential gene expression studies using these mMSCs have suggested potential genes and pathways specifically altered by FUS-CHOP expression, which could be involved in liposarcoma development, including PDGF signaling, RXR signaling, and sphingolipid and fatty acid metabolism40,65.
Mouse models
Transgenic mouse models have also provided clues about the transforming mechanisms and identity of the target cell where FUS-CHOP exerts its tumorigenic effect. Thus, transgenic mice expressing FUS-CHOP or CHOP-FUS transgenes under the control of the ubiquitous E1Fa promoter gave rise to similar liposarcomas that resemble their human counterparts66,67. On the other hand, although the uncontrolled expression of CHOP after the chromosomal translocation seems to play a leading role in liposarcoma development64, transgenic mice expressing CHOP alone do not develop any tumor67 and the expression of FUS restores liposarcoma development in these CHOP-transgenic mice68. These results provide evidence that the FUS portion of FUS-CHOP also plays a specific and critical role in the pathogenesis of liposarcoma. Furthermore, the immature nature of liposarcoma cell progenitors was suggested by the generation of an aP2-FUS-CHOP transgenic model, where FUS-CHOP was not able to induce liposarcoma development when expressed in differentiated, aP2-expressing, adipocytes69. In addition, studies using embryonic fibroblasts from these mouse models have concluded that FUS-CHOP prevents the development of adipocytic precursors by repressing PPARγ and C/EBP as part of a mechanism of differentiation disruption that seems to be required for liposarcoma development69,70.
Human MSCs
In the human setting, however, the expression of FUS-CHOP does not transform either wt or p53-deficient hASCs40. Nevertheless, the expression of either FUS-CHOP or CHOP in fibrosarcoma cell lines induces the formation of liposarcoma-like tumors71, highlighting the need for further cooperating mutations in the FUS-CHOP-expressing hMSC model. A microarray gene expression profiling has revealed potential deregulated pathways (e.g., Wnt, PTEN or PI3K/AKT) in liposarcoma formation from p53-deficient FUS-CHOP-expressing mASCs, which might also be potential candidates for cooperating mutations in the transformation of hASCs40.
ARMS models
The ARMS is a subtype of rhabdomyosarcoma characterized by an appearance similar to the alveoli of the lungs. There is also evidence that MSCs are the cells of origin for ARMS72. This tumor is characterized by the expression of either PAX3-FKHR or PAX7-FKHR fusion genes in MSCs, pushing MSC differentiation towards a myogenic lineage while inhibiting terminal differentiation.
mMSCs
Initial studies showed the ability of PAX3-FKHR to transform mouse fibroblasts73. However, PAX3-FKHR and PAX7-FKHR fusions induced skeletal myogenesis but not transformation when introduced in BM-mMSCs74. Nevertheless, the expression of a dominant-negative form of p53 or SV40 large T antigen (which inactivates both p53 and Rb) elicits tumor formation in a proportion of the PAX-FKHR-expressing cells. Additional expression of the constitutively active H-RASG12V leads to tumor formation in all of the PAX-FKHR-expressing populations. These PAX-FKHR-expressing tumors display histological features and gene expression profiles similar to human ARMS74.
Mouse models
Similar to the aforementioned studies on primary MSCs, mouse models of PAX-FKHR fusions also several the need for additional secondary genetic events to develop overt ARMS. In one study using a Pax3-Fkhr knock-in approach, the heterozygous offspring of PAX3-FKHR chimeric mice showed developmental abnormalities although no signs of malignancy were observed75. In another model, a conditional Pax3-Fkhr knock-in allele was introduced specifically in MYF6-expressing skeletal muscle76. Although ARMS occurs at low frequency in these conditional mice, complementary disruption of p53 or the INK4A/ARF locus substantially increases the frequency of ARMS76.
Synovial sarcoma models
Synovial sarcomas (SS) often arise deep in the soft tissue near a joint in the extremity of young adult patients. Most SS are characterized by t(X;18)(p11.2;q11.2), resulting in a fusion between the SS18 (SYT) gene on chromosome 18 and one of the SSX genes on the X chromosome, creating SS18-SSX1, SS18-SSX2 or SS18-SSX4 chimeric genes77. Although less studied than other STS, there are also several clues suggesting a potential MSC origin in synovial sarcoma.
Mouse models
An interesting mouse model of SS based on the conditional expression of SYT-SSX2 in several skeletal muscle cell types has been reported78. Interestingly, SS tumor is reproduced when the SYT-SSX2 fusion is expressed in immature myoblasts (MYF5+) but not in more differentiated cells (MYF6+), highlighting how the same genetic alteration may lead to different outcomes/tumor phenotype in different cell populations down the lineage hierarchy.
Human MSCs
In the human setting, silencing of the fusion gene expression with specific shRNA in primary SS cells induces the expression of mesenchymal markers and enhances their ability to differentiate into osteocytes, chondrocytes and adipocytes, suggesting that MSCs could be at the origin of this disease79. Similarly, the expression of SYT-SSX1 in hMSCs induces a transcriptional profile very similar to the SS expression signature80.
We have reviewed mounting evidence suggesting that multipotent and long-lived MSCs may provide an ideal cellular target for the initiation of some sarcomas upon the expression of specific fusion genes. However, no fusion gene-based model of sarcoma has been developed so far using hMSCs. The fusion genes seem to primarily act to block differentiation towards a given pathway. According to the simplistic dogma of cancer where both differentiation and proliferation processes have to be impaired or deregulated for cancer initiation, the differentiation blockage is not sufficient for malignant transformation and secondary transforming hits would be needed to fully transform hMSCs. The identification of these relevant cooperating events will likely lead to the successful development of these currently non-existing sarcoma models (based on hMSCs). Interestingly, preliminary results from our lab suggest that it is possible to develop a human sarcoma model based on the enforced expression of a specific fusion gene in human MSCs harboring cooperating transforming hits (data not shown).
Sarcoma-initiating/stem cells
There is considerable evidence that sarcomas are hierarchically organized and sustained by a subpopulation of self-renewing cells that can generate the full repertoire of tumor cells. CSCs that display tumor re-initiating properties have been recently identified in osteosarcoma81,82,83, chondrosarcoma82, Ewing's sarcoma61 and synovial sarcoma79. The identification of these sarcoma-initiating cells was based on both their ability to form spherical, clonal expanding colonies (called sarcospheres) in anchorage-independent and serum-starved conditions and the expression of stem cell markers61,79,81,82,83,84. All of these CSCs are characterized by the expression of the pluripotent stem cell markers OCT3/4, NANOG and SOX2 and are able to self-renew and to sustain the tumor in serial transplantation experiments. More importantly, many of these sarcoma-initiating cells express MSC markers79,81,82,83 and retain MSC in vitro differentiation properties, giving rise to adipogenic, chondrogenic and osteogenic lineages61,79,82. In addition, these MSC-like CSCs are associated with drug resistance and metastasis81,84 and therefore, they may be responsible for the frequent relapses observed in sarcomas85.
It is worth mentioning that some of the factors involved in induced pluripotency are also involved in sarcomagenesis. For instance, SOX2 has been reported to play a key role in the development of Ewing's sarcoma62, whereas BMI1, which has been previously shown to be involved in sarcomagenesis44, has also very recently been shown to be relevant in induced pluripotency86.
Although an alternative model in which stochastic genetic events determine the development of the tumor can not be excluded, the aforementioned data indicate that at least some sarcomas fulfill phenotypic and functional features reminiscent of the hierarchical model of cancer, suggesting a strong link between sarcomas and MSCs. Intriguingly, MSCs may not only be the TIC in sarcomas, but also, a population of altered MSCs could constitute the CSCs responsible for maintaining tumor growth, being able to initiate tumorigenesis upon serial transplantation.
MSCs and tumor growth
The role of MSCs in tumorigenesis could also be an indirect phenomenon87,88. MSCs are frequently recruited to the site of tissue injury or tumor growth and sometimes, in the appropriate and permissive environment and under stress conditions, this could also represent a potential source of malignancy. Thus, MSCs within the tumor stroma facilitate breast cancer metastasis through the secretion of the chemokines CCL589 and CCL290. Likewise, hMSCs target osteosarcoma and promote its growth and pulmonary metastasis through secretion of CCL591. Moreover, a recent study reported that MSCs protect breast cancer cells through the TGF-β1-mediated increase of regulatory T-cells92.
The BM microenvironment plays a role in the pathogenesis of a variety of hematological malignancies including acute lymphoblastic leukemia (ALL), multiple myeloma or myelodysplastic syndrome93,94,95. The onset and progression of hematological malignancies are in many cases dependent on mutual interactions between the leukemic blasts/plasma cells and BM stroma/MSCs, which provide survival and growth-promoting signals8,95,96. Interestingly, the fusion MLL-AF4 was recently found expressed in both BM-MSCs and leukemic blasts in 100% of infants suffering from pro-B ALL highlighting an unrecognized role of the BM milieu in the pathogenesis of this dismal infant leukemia97. Importantly, this study revealed the absence of monoclonal rearrangements in MLL-AF4+ BM-MSCs precluding the possibility of cellular plasticity or de-differentiation of B-ALL blasts and suggests that MLL-AF4 might arise in a population of mesodermal precursors. In addition, BM-MSCs are resistant to chemotherapy-induced apoptosis98,99,100 and contribute to generating drug resistance in tumor cells95,101. Likewise, several studies have evidenced that hMSCs are highly resistant to ionizing radiation102. Collectively, these data suggest important implications for cancer therapy as this chemo- and radio-resistance could lead to the accumulation of mutations, resulting in MSC transformation and eventual generation of refractory/secondary tumors98.
Despite the reported ability of MSCs to contribute to tumor growth under certain circumstances, there are also solid studies claiming their potential to inhibit tumor growth. Thus, human and mMSCs can home to tumor sites and inhibit the growth of neoplastic cells as shown in models of gliomas103, Kaposi's sarcomas104 and hepatoma105,106. Other study shows that hMSCs exhibit an antiproliferative activity on tumor cells, although in in-vivo experiments, the co-injection of MSCs caused an increase in tumor cell growth rate107.
Intriguingly, experimental evidence suggests that MSCs may either favor or inhibit tumor growth depending on the genetic background of the tumor cells108. For instance, MSCs have been shown to accelerate tumoral growth and promote metastasis of estrogen receptor-alpha+ (ERα+) but not ERα− breast cancer cells89. Likewise, the capacity of MSCs to inhibit cellular growth in Kaposi's sarcoma depends on their ability to shut down AKT activity in the tumor cells104. These findings imply that if the interactions between cancer cells and MSCs in specific cancers can be elucidated, we could develop more effective anti-cancer strategies based on the use of wt or manipulated MSCs.
In addition to the ability of MSCs to promote tumor growth, other non-MSC cell types may acquire mesenchymal properties and exert a relevant function in cancer development. Thus, the epithelial to mesenchymal transition (EMT) plays crucial roles in the formation of the body plan and in the differentiation of multiple tissues and organs. EMT can also adversely cause organ fibrosis and promote carcinoma progression through a variety of mechanisms. EMT promotes the acquisition of a mesenchymal phenotype by tumoral epithelial cells, resulting in gain of migratory and invasive properties and induction of stem cell properties. Thus, the mesenchymal state is associated with the capacity of carcinoma (epithelial) cells to migrate to distant organs and maintain stemness, allowing their subsequent differentiation into multiple cell types and initiation of metastasis109.
Worth mentioning, emerging evidence links mesenchymal-state metastasic cancer with infiltrating macrophages110. It has been proposed that many metastasic cancers may arise from myeloid/macrophages rather than from EMTs. In fact, numerous cancers exhibit multiple properties of macrophages, including phagocytosis. It is tempting to speculate that the macrophage properties expressed in metastasic cancers may arise from damage to an already existing mesenchymal cell. Although this is still a nascent area of investigation, the view of metastasis as a myeloid/macrophage disease might impact future cancer research and intervention110.
In light of the roles of MSCs in tumorigenesis, it would be crucial to expand our understanding about the nature of MSCs in order to better utilize the immunosuppressive and regenerative properties of hMSCs without promoting tumor growth.
Open questions
Because of their unique properties, MSCs represent one of the most promising adult stem cells being used worldwide in many clinical applications. However, owing to some of their intrinsic aforementioned properties, MSCs may also become a double-edged sword since they may support tumor cell growth and are being explored as the target cell for the origin of sarcomas. At this point, it is important to stress that there is no solid evidence for hMSC transformation during ex vivo expansion, and therefore, hMSCs seem to be generally safe for clinical applications in terms of potential risk of transformation to sarcoma, based on early data. However, longer follow-up of patients is still highly demanded. In any case, the fact that hMSCs could be the target cell for transforming mutations giving rise to sarcoma formation should not necessarily hamper their clinical use, since the likelihood of transformation of the infused cells should not be higher than that of patient's own cells.
Here, we have reviewed the published literature suggesting a role of MSC populations as TIC and CSC for different types of sarcoma. Besides the intrinsic transforming ability of specific mutations, it is necessary that these mutations hit the appropriate target cell in order to induce sarcoma formation. A debate has emerged about the cell of origin that suffers these mutations responsible for sarcoma development. Two main models may be conceptualized to support the MSCs as a potential target cell for sarcomas. It is suggested that either (i) the different sarcomas come from MSCs at different stages of differentiation that suffer specific mutations resulting in a blockage of terminal differentiation which, in turn, determines the degree of tumor differentiation, or (ii) sarcomas originate from a primitive MSC, which acquires relevant mutations that direct tumor genesis (Figure 1).
Schematic cartoon depicting how distinct sarcomas may result from a coordinated acquisition of cooperating oncogenic hits in the appropriate target cell throughout the mesenchymal hierarchy. In the absence of oncogenic hits the normal MSC (black circle; left) differentiates down the mesenchymal hierarchy eventually giving rise to mature and functional mesenchymal derivatives including adipocytes, chondrocytes and osteocytes. The “two-hit” model is thought to be necessary for explaining the eventual development of cancer: one hit is presumed to promote differentiation impairment while the second hit more frequently targets proliferation/apoptosis. Distinct early cancer-initiating hits (white-colored; hits A1-A4) are supposed to arise in long-lived MSCs, or perhaps, in early committed mesenchymal progenitors. It is very unlikely that a single early cancer-initiating hit induces sarcomagenesis on its own, and therefore sequential secondary cooperating hits (green, blue or red-coloured hits) are commonly required to achieve a malignant clonal expansion of mesenchymal derivatives. The more differentiated the stage (less MSC potency) along the mesenchymal hierarchy targeted by the secondary oncogenic mutation, the more differentiated the sarcoma appears. This model stresses both the importance of the intrinsic transforming ability of specific mutations and the need to target the appropriate cell type along the mesenchymal lineages.
The first model is supported by studies showing that the gene expression signature is surprisingly similar between sarcomas in different stages of differentiation and normal MSCs in similar stages of differentiation. Such studies were reported for liposarcoma111, chondrosarcoma112, osteosarcoma52 and leiomyosarcoma32. Likewise, osteosarcoma and ARMS have been modeled by the establishment of relevant oncogenic hits in nearly differentiated cells of the osteoblastic and myoblastic lineages, respectively34,35,76. The second model is supported by many studies reporting sarcoma formation from spontaneous or mutation-induced transformation of human or mouse primitive MSCs. Likewise, several types of CSCs presenting MSC properties have been reported61,79,82 and moreover, sarcoma cells of certain subtypes can also differentiate into multiple mesenchymal lineages in vitro30,31,42. Existing sarcoma mouse models also provide arguments in favor of this theory. Thus, MLS development has been reported after ubiquitous expression of FUS-CHOP but not when the fusion protein expression was restricted to aP2-expressing adipocytes suggesting that liposarcoma comes from a more immature cell type66,69. Similarly, the SYT-SSX2 fusion gene is able to trigger SS formation when it is expressed in immature myoblasts but not in more differentiated cells78.
Most likely, both models are not exclusive and could converge in a common model where sarcoma originates from MSCs that suffer sequential mutations targeting differentiation and proliferation pathways, resulting in sarcomas showing different degrees of differentiation depending on the potency of the cell along the MSC lineage that eventually gives rise to the tumor (Figure 1). The pathogenesis of Li-Fraumeni patients represents an interesting system to address whether these models could converge in a common model because these patients carry germline mutations of p53, which do not transform undifferentiated cells but might cooperate with subsequent mutations in more differentiated cells to induce sarcoma development. Further work aimed to better understand the nature of MSCs is needed to provide more specific markers, which will allow the identification of subpopulations with different differentiation capacities, which would facilitate the generation of both in vitro and in vivo sarcoma models based on the transformation of immature MSCs.
Worth mentioning, the tissue source of the MSCs may also represent an important factor influencing MSC transformation and the development of bona fide MSC-based models for sarcomagenesis. It should not be assumed that MSCs present in different tissues all have the same potential to differentiate along the different mesodermal lineages. Moreover, the environment and signaling stimuli that MSCs receive also vary among tissues. Therefore, future studies are expected to dissect the link between the tissue from which MSCs are sourced and the resulting sarcoma phenotype. For instance, p53-deficient mASCs originate leiomyosarcoma31, while the loss of p53 in mesenchymal cells of limb buds or in the osteogenic lineage gives rise to osteosarcoma development34,36. Likewise, supporting a role for MSCs from tissues other than BM in the initiation of sarcomas, it has been recently reported that local resident MSCs and not BM-derived cells are the preferential target for initiation of undifferentiated pleomorphic sarcomas associated with p53 and Rb deficiency113.
Regarding the mechanisms underlying MSC transformation, mounting evidence suggests that the expression of sarcoma-related fusion genes in hMSCs does not suffice on its own for sarcoma initiation revealing the need for secondary oncogenic hits to achieve overt MSC transformation and in vivo sarcoma growth. Since fusion genes mostly disrupt differentiation, cooperating mutations are expected to target proliferation and apoptosis checkpoints. In this regard, the inactivation of p53 is sufficient to transform mMSCs31 and generate sarcomas in mesenchymal tissues of mouse models36. Similarly, p53 mutation has also been successfully used as a cooperating transforming hit in the development of several models of fusion gene-associated sarcomas from mMSCs40,54,74 or in mouse models58,76 (Table 3). According to the available literature, the frequency of p53 mutations in human sarcomas ranges from ∼6% in well-differentiated/dedifferentiated liposacomas to 23% in osteosarcomas114. Nevertheless, the disruption of p53 signaling seems to be a key oncogenic event in many types of sarcomas12. For example, the expression of EWS-FLI-1 could silence p53 activity through the formation of an EWS-FLI-1/p53 complex115 or inhibit NOTCH induced-p53 activation116. Moreover, the p53 inhibitor Mdm2 is often overexpressed in STS117, and p53 and p16INK4A/p14ARF pathways are frequently disrupted in MLS118. Finally, other common abnormalities in sarcomas that could function as cooperating hits include defects in pathways controlled by Rb and different growth signaling factors, like those mediated by IGF1, PDGF or c-KIT12.
In order to develop MSC-based models for sarcomagenesis, which closely reproduce the human disease it would be crucial to characterize more specific secondary cooperating mutations including point mutations, genomic losses and gains and copy number variations, etc, that are indispensable for sarcoma onset and progression. A desirable approach would be to apply cutting-edge whole-genome technologies such as deep sequencing to a cohort of different types of primary sarcomas in an attempt to identify specific mutations shared by a group of patients with the same tumor. The resulting data should then be functionally validated in vitro and in vivo in normal or fusion gene-harboring MSCs. Using this technology a recent study has identified frequently mutated genes in different subtypes of sarcomas that could constitute new targets for more specific therapies119. These frequently mutated genes include TP53 in pleomorphic liposarcomas, NF1 in myxofibrosarcomas and PIK3CA (the catalytic subunit of PI3K) in MLS.
Concluding remarks
Sarcomas are generally studied when the full transformation events have already occurred and therefore, the mechanisms of transformation and pathogenesis are not amenable to analysis with patient samples. Thus there exists the need to establish bona fide mouse and human-based models to recapitulate sarcomagenesis in vitro and in vivo. Over recent years, mounting evidence indicates that MSCs from different sources (BM, adipose-tissue, etc) may represent the putative target cell of origin for a variety of human sarcomas, thus linking MSCs and cancer. Future research should be aimed at defining precisely the specific phenotype of the MSC populations at the origin of the different types of sarcomas as well as at dissecting the mechanisms governing MSC transformation. We envision that experimental research based on MSCs coupled to whole-genome sequencing of different types of primary sarcomas will advance our attempts to develop accurate MSC-based models of sarcomagenesis and to decipher the underlying mechanisms, provide a better understanding about the onset and progression of mesenchymal cancer, and lead to the eventual development of more specific therapies directed against the sarcoma-initiating cell.
References
Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science 1999; 284:143–147.
Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006; 8:315–317.
da Silva Meirelles L, Chagastelles PC, Nardi NB . Mesenchymal stem cells reside in virtually all post-natal organs and tissues. J Cell Sci 2006; 119:2204–2213.
Kern S, Eichler H, Stoeve J, Kluter H, Bieback K . Comparative analysis of mesenchymal stem cells from bone marrow, umbilical cord blood, or adipose tissue. Stem Cells 2006; 24:1294–1301.
Sanchez L, Gutierrez-Aranda I, Ligero G, et al. Enrichment of human ESC-derived multipotent mesenchymal stem cells with immunosuppressive and anti-inflammatory properties capable to protect against experimental inflammatory bowel disease. Stem Cells 2011; 29:251–262.
Crisan M, Yap S, Casteilla L, et al. A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell 2008; 3:301–313.
Bianco P, Robey PG, Simmons PJ . Mesenchymal stem cells: revisiting history, concepts, and assays. Cell Stem Cell 2008; 2:313–319.
Garcia-Castro J, Trigueros C, Madrenas J, et al. Mesenchymal stem cells and their use as cell replacement therapy and disease modelling tool. J Cell Mol Med 2008; 12:2552–2565.
Stagg J . Mesenchymal stem cells in cancer. Stem Cell Rev 2008; 4:119–124.
Mohseny AB, Hogendoorn PC . Mesenchymal tumors: when stem cells go mad. Stem Cells 2011; 29:397–403.
Skubitz KM, D'Adamo DR . Sarcoma. Mayo Clin Proc 2007; 82:1409–1432.
Helman LJ, Meltzer P . Mechanisms of sarcoma development. Nat Rev Cancer 2003; 3:685–694.
Vermeulen L, Sprick MR, Kemper K, Stassi G, Medema JP . Cancer stem cells--old concepts, new insights. Cell Death Differ 2008; 15:947–958.
Visvader JE . Cells of origin in cancer. Nature 2011; 469:314–322.
Li H, Fan X, Kovi RC, et al. Spontaneous expression of embryonic factors and p53 point mutations in aged mesenchymal stem cells: a model of age-related tumorigenesis in mice. Cancer Res 2007; 67:10889–10898.
Miura M, Miura Y, Padilla-Nash HM, et al. Accumulated chromosomal instability in murine bone marrow mesenchymal stem cells leads to malignant transformation. Stem Cells 2006; 24:1095–1103.
Mohseny AB, Szuhai K, Romeo S, et al. Osteosarcoma originates from mesenchymal stem cells in consequence of aneuploidization and genomic loss of Cdkn2. J Pathol 2009; 219:294–305.
Tolar J, Nauta AJ, Osborn MJ, et al. Sarcoma derived from cultured mesenchymal stem cells. Stem Cells 2007; 25:371–379.
Zhou YF, Bosch-Marce M, Okuyama H, et al. Spontaneous transformation of cultured mouse bone marrow-derived stromal cells. Cancer Res 2006; 66:10849–10854.
Wang Y, Huso DL, Harrington J, et al. Outgrowth of a transformed cell population derived from normal human BM mesenchymal stem cell culture. Cytotherapy 2005; 7:509–519.
Garcia S, Martin MC, de la Fuente R, et al. Pitfalls in spontaneous in vitro transformation of human mesenchymal stem cells. Exp Cell Res 2010; 316:1648–1650.
Torsvik A, Rosland GV, Svendsen A, et al. Spontaneous malignant transformation of human mesenchymal stem cells reflects cross-contamination: putting the research field on track - letter. Cancer Res 2010; 70:6393–6396.
Bernardo ME, Zaffaroni N, Novara F, et al. Human bone marrow derived mesenchymal stem cells do not undergo transformation after long-term in vitro culture and do not exhibit telomere maintenance mechanisms. Cancer Res 2007; 67:9142–9149.
Choumerianou DM, Dimitriou H, Perdikogianni C, et al. Study of oncogenic transformation in ex vivo expanded mesenchymal cells, from paediatric bone marrow. Cell Prolif 2008; 41:909–922.
Gou S, Wang C, Liu T, et al. Spontaneous differentiation of murine bone marrow-derived mesenchymal stem cells into adipocytes without malignant transformation after long-term culture. Cells Tissues Organs 2010; 191:185–192.
Grimes BR, Steiner CM, Merfeld-Clauss S, et al. Interphase FISH demonstrates that human adipose stromal cells maintain a high level of genomic stability in long-term culture. Stem Cells Dev 2009; 18:717–724.
Larson BL, Ylostalo J, Lee RH, Gregory C, Prockop DJ . Sox11 is expressed in early progenitor human multipotent stromal cells and decreases with extensive expansion of the cells. Tissue Eng Part A 2010; 16:3385–3394.
Tarte K, Gaillard J, Lataillade JJ, et al. Clinical-grade production of human mesenchymal stromal cells: occurrence of aneuploidy without transformation. Blood 2010; 115:1549–1553.
Armesilla-Diaz A, Elvira G, Silva A . p53 regulates the proliferation, differentiation and spontaneous transformation of mesenchymal stem cells. Exp Cell Res 2009; 315:3598–3610.
Rodriguez R, Rubio R, Masip M, et al. Loss of p53 induces tumorigenesis in p21-deficient mesenchymal stem cells. Neoplasia 2009; 11:397–407.
Rubio R, Garcia-Castro J, Gutierrez-Aranda I, et al. Deficiency in p53 but not retinoblastoma induces the transformation of mesenchymal stem cells in vitro and initiates leiomyosarcoma in vivo. Cancer Res 2010; 70:4185–4194.
Danielson LS, Menendez S, Attolini CS, et al. A differentiation-based microRNA signature identifies leiomyosarcoma as a mesenchymal stem cell-related malignancy. Am J Pathol 2010; 177:908–917.
Shimizu T, Ishikawa T, Sugihara E, et al. c-MYC overexpression with loss of Ink4a/Arf transforms bone marrow stromal cells into osteosarcoma accompanied by loss of adipogenesis. Oncogene 2010; 29:5687–5699.
Berman SD, Calo E, Landman AS, et al. Metastatic osteosarcoma induced by inactivation of Rb and p53 in the osteoblast lineage. Proc Natl Acad Sci U S A 2008; 105:11851–11856.
Walkley CR, Qudsi R, Sankaran VG, et al. Conditional mouse osteosarcoma, dependent on p53 loss and potentiated by loss of Rb, mimics the human disease. Genes Dev 2008; 22:1662–1676.
Lin PP, Pandey MK, Jin F, et al. Targeted mutation of p53 and Rb in mesenchymal cells of the limb bud produces sarcomas in mice. Carcinogenesis 2009; 30:1789–1795.
Kirsch DG, Dinulescu DM, Miller JB, et al. A spatially and temporally restricted mouse model of soft tissue sarcoma. Nat Med 2007; 13:992–997.
Tsumura H, Yoshida T, Saito H, Imanaka-Yoshida K, Suzuki N . Cooperation of oncogenic K-ras and p53 deficiency in pleomorphic rhabdomyosarcoma development in adult mice. Oncogene 2006; 25:7673–7679.
Hung SC, Yang DM, Chang CF, et al. Immortalization without neoplastic transformation of human mesenchymal stem cells by transduction with HPV16 E6/E7 genes. Int J Cancer 2004; 110:313–319.
Rodriguez R, Rubio R, Gutierrez-Aranda I, et al. Fus-Chop fusion protein expression coupled to P53 deficiency induces liposarcoma in mouse but not human adipose-derived mesenchymal stem/stromal cells. Stem Cells 2011; 29:179–192.
Funes JM, Quintero M, Henderson S, et al. Transformation of human mesenchymal stem cells increases their dependency on oxidative phosphorylation for energy production. Proc Natl Acad Sci U S A 2007; 104:6223–6228.
Li N, Yang R, Zhang W, et al. Genetically transforming human mesenchymal stem cells to sarcomas: changes in cellular phenotype and multilineage differentiation potential. Cancer 2009; 115:4795–4806.
Wild L, Funes JM, Boshoff C, Flanagan JM . In vitro transformation of mesenchymal stem cells induces gradual genomic hypomethylation. Carcinogenesis 2010; 31:1854–1862.
Shima Y, Okamoto T, Aoyama T, et al. In vitro transformation of mesenchymal stem cells by oncogenic H-rasVal12. Biochem Biophys Res Commun 2007; 353:60–66.
Serakinci N, Guldberg P, Burns JS, et al. Adult human mesenchymal stem cell as a target for neoplastic transformation. Oncogene 2004; 23:5095–5098.
Hernando E, Charytonowicz E, Dudas ME, et al. The AKT-mTOR pathway plays a critical role in the development of leiomyosarcomas. Nat Med 2007; 13:748–753.
Fodde R, Brabletz T . Wnt/beta-catenin signaling in cancer stemness and malignant behavior. Curr Opin Cell Biol 2007; 19:150–158.
De Boer J, Wang HJ, Van Blitterswijk C . Effects of Wnt signaling on proliferation and differentiation of human mesenchymal stem cells. Tissue Eng 2004; 10:393–401.
Neth P, Ciccarella M, Egea V, et al. Wnt signaling regulates the invasion capacity of human mesenchymal stem cells. Stem Cells 2006; 24:1892–1903.
Wu C, Nik-Amini S, Nadesan P, Stanford WL, Alman BA . Aggressive fibromatosis (desmoid tumor) is derived from mesenchymal progenitor cells. Cancer Res 2010; 70:7690–7698.
Matushansky I, Hernando E, Socci ND, et al. Derivation of sarcomas from mesenchymal stem cells via inactivation of the Wnt pathway. J Clin Invest 2007; 117:3248–3257.
Cleton-Jansen AM, Anninga JK, Briaire-de Bruijn IH, et al. Profiling of high-grade central osteosarcoma and its putative progenitor cells identifies tumourigenic pathways. Br J Cancer 2009; 101:1909–1918.
de Alava E, Gerald WL . Molecular biology of the Ewing's sarcoma/primitive neuroectodermal tumor family. J Clin Oncol 2000; 18:204–213.
Castillero-Trejo Y, Eliazer S, Xiang L, Richardson JA, Ilaria RL, Jr. Expression of the EWS/FLI-1 oncogene in murine primary bone-derived cells Results in EWS/FLI-1-dependent, ewing sarcoma-like tumors. Cancer Res 2005; 65:8698–8705.
Riggi N, Cironi L, Provero P, et al. Development of Ewing's sarcoma from primary bone marrow-derived mesenchymal progenitor cells. Cancer Res 2005; 65:11459–11468.
Cironi L, Riggi N, Provero P, et al. IGF1 is a common target gene of Ewing's sarcoma fusion proteins in mesenchymal progenitor cells. PLoS One 2008; 3:e2634.
Lin PP, Wang Y, Lozano G . Mesenchymal stem cells and the origin of Ewing's sarcoma. Sarcoma 2011; 2011:276463.
Lin PP, Pandey MK, Jin F, et al. EWS-FLI1 induces developmental abnormalities and accelerates sarcoma formation in a transgenic mouse model. Cancer Res 2008; 68:8968–8975.
Riggi N, Suva ML, Suva D, et al. EWS-FLI-1 expression triggers a Ewing's sarcoma initiation program in primary human mesenchymal stem cells. Cancer Res 2008; 68:2176–2185.
Tirode F, Laud-Duval K, Prieur A, et al. Mesenchymal stem cell features of Ewing tumors. Cancer Cell 2007; 11:421–429.
Suva ML, Riggi N, Stehle JC, et al. Identification of cancer stem cells in Ewing's sarcoma. Cancer Res 2009; 69:1776–1781.
Riggi N, Suva ML, De Vito C, et al. EWS-FLI-1 modulates miRNA145 and SOX2 expression to initiate mesenchymal stem cell reprogramming toward Ewing sarcoma cancer stem cells. Genes Dev 2010; 24:916–932.
Perez-Mancera PA, Sanchez-Garcia I . Understanding mesenchymal cancer: the liposarcoma-associated FUS-DDIT3 fusion gene as a model. Semin Cancer Biol 2005; 15:206–214.
Zinszner H, Albalat R, Ron D . A novel effector domain from the RNA-binding protein TLS or EWS is required for oncogenic transformation by CHOP. Genes Dev 1994; 8:2513–2526.
Riggi N, Cironi L, Provero P, et al. Expression of the FUS-CHOP fusion protein in primary mesenchymal progenitor cells gives rise to a model of myxoid liposarcoma. Cancer Res 2006; 66:7016–7023.
Perez-Losada J, Pintado B, Gutierrez-Adan A, et al. The chimeric FUS/TLS-CHOP fusion protein specifically induces liposarcomas in transgenic mice. Oncogene 2000; 19:2413–2422.
Perez-Losada J, Sanchez-Martin M, Rodriguez-Garcia MA, et al. Liposarcoma initiated by FUS/TLS-CHOP: the FUS/TLS domain plays a critical role in the pathogenesis of liposarcoma. Oncogene 2000; 19:6015–6022.
Perez-Mancera PA, Perez-Losada J, Sanchez-Martin M, et al. Expression of the FUS domain restores liposarcoma development in CHOP transgenic mice. Oncogene 2002; 21:1679–1684.
Perez-Mancera PA, Vicente-Duenas C, Gonzalez-Herrero I, et al. Fat-specific FUS-DDIT3-transgenic mice establish PPARgamma inactivation is required to liposarcoma development. Carcinogenesis 2007; 28:2069–2073.
Perez-Mancera PA, Bermejo-Rodriguez C, Sanchez-Martin M, et al. FUS-DDIT3 prevents the development of adipocytic precursors in liposarcoma by repressing PPARgamma and C/EBPalpha and activating eIF4E. PLoS One 2008; 3:e2569.
Engstrom K, Willen H, Kabjorn-Gustafsson C, et al. The myxoid/round cell liposarcoma fusion oncogene FUS-DDIT3 and the normal DDIT3 induce a liposarcoma phenotype in transfected human fibrosarcoma cells. Am J Pathol 2006; 168:1642–1653.
Charytonowicz E, Cordon-Cardo C, Matushansky I, Ziman M . Alveolar rhabdomyosarcoma: is the cell of origin a mesenchymal stem cell? Cancer Lett 2009; 279:126–136.
Scheidler S, Fredericks WJ, Rauscher FJ 3rd, Barr FG, Vogt PK . The hybrid PAX3-FKHR fusion protein of alveolar rhabdomyosarcoma transforms fibroblasts in culture. Proc Natl Acad Sci U S A 1996; 93:9805–9809.
Ren YX, Finckenstein FG, Abdueva DA, et al. Mouse mesenchymal stem cells expressing PAX-FKHR form alveolar rhabdomyosarcomas by cooperating with secondary mutations. Cancer Res 2008; 68:6587–6597.
Lagutina I, Conway SJ, Sublett J, Grosveld GC . Pax3-FKHR knock-in mice show developmental aberrations but do not develop tumors. Mol Cell Biol 2002; 22:7204–7216.
Keller C, Arenkiel BR, Coffin CM, et al. Alveolar rhabdomyosarcomas in conditional Pax3:Fkhr mice: cooperativity of Ink4a/ARF and Trp53 loss of function. Genes Dev 2004; 18:2614–2626.
Jain S, Xu R, Prieto VG, Lee P . Molecular classification of soft tissue sarcomas and its clinical applications. Int J Clin Exp Pathol 2010; 3:416–428.
Haldar M, Hancock JD, Coffin CM, Lessnick SL, Capecchi MR . A conditional mouse model of synovial sarcoma: insights into a myogenic origin. Cancer Cell 2007; 11:375–388.
Naka N, Takenaka S, Araki N, et al. Synovial sarcoma is a stem cell malignancy. Stem Cells 2010; 28:1119–1131.
Cironi L, Provero P, Riggi N, et al. Epigenetic features of human mesenchymal stem cells determine their permissiveness for induction of relevant transcriptional changes by SYT-SSX1. PLoS One 2009; 4:e7904.
Adhikari AS, Agarwal N, Wood BM, et al. CD117 and Stro-1 identify osteosarcoma tumor-initiating cells associated with metastasis and drug resistance. Cancer Res 2010; 70:4602–4612.
Gibbs CP, Kukekov VG, Reith JD, et al. Stem-like cells in bone sarcomas: implications for tumorigenesis. Neoplasia 2005; 7:967–976.
Levings PP, McGarry SV, Currie TP, et al. Expression of an exogenous human Oct-4 promoter identifies tumor-initiating cells in osteosarcoma. Cancer Res 2009; 69:5648–5655.
Fujii H, Honoki K, Tsujiuchi T, et al. Sphere-forming stem-like cell populations with drug resistance in human sarcoma cell lines. Int J Oncol 2009; 34:1381–1386.
Honoki K . Do stem-like cells play a role in drug resistance of sarcomas? Expert Rev Anticancer Ther 2010; 10:261–270.
Moon JH, Heo JS, Kim JS, et al. Reprogramming fibroblasts into induced pluripotent stem cells with Bmi1. Cell Res 2011; 21:1305–1315.
Lazennec G, Jorgensen C . Concise review: adult multipotent stromal cells and cancer: risk or benefit? Stem Cells 2008; 26:1387–1394.
Roorda BD, ter Elst A, Kamps WA, de Bont ES . Bone marrow-derived cells and tumor growth: contribution of bone marrow-derived cells to tumor micro-environments with special focus on mesenchymal stem cells. Crit Rev Oncol Hematol 2009; 69:187–198.
Karnoub AE, Dash AB, Vo AP, et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature 2007; 449:557–563.
Molloy AP, Martin FT, Dwyer RM, et al. Mesenchymal stem cell secretion of chemokines during differentiation into osteoblasts, and their potential role in mediating interactions with breast cancer cells. Int J Cancer 2009; 124:326–332.
Xu WT, Bian ZY, Fan QM, Li G, Tang TT . Human mesenchymal stem cells (hMSCs) target osteosarcoma and promote its growth and pulmonary metastasis. Cancer Lett 2009; 281:32–41.
Patel SA, Meyer JR, Greco SJ, et al. Mesenchymal stem cells protect breast cancer cells through regulatory T cells: role of mesenchymal stem cell-derived TGF-{beta}. J Immunol 2010; 184:5885–5894.
Blau O, Hofmann WK, Baldus CD, et al. Chromosomal aberrations in bone marrow mesenchymal stroma cells from patients with myelodysplastic syndrome and acute myeloblastic leukemia. Exp Hematol 2007; 35:221–229.
Corre J, Mahtouk K, Attal M, et al. Bone marrow mesenchymal stem cells are abnormal in multiple myeloma. Leukemia 2007; 21:1079–1088.
Iwamoto S, Mihara K, Downing JR, Pui CH, Campana D . Mesenchymal cells regulate the response of acute lymphoblastic leukemia cells to asparaginase. J Clin Invest 2007; 117:1049–1057.
Bueno C, Lopes LF, Menendez P . Bone marrow stromal cell-derived Wnt signals as a potential underlying mechanism for cyclin D1 deregulation in multiple myeloma lacking t(11;14)(q13;q32). Blood Cells Mol Dis 2007; 39:366–368.
Menendez P, Catalina P, Rodriguez R, et al. Bone marrow mesenchymal stem cells from infants with MLL-AF4+ acute leukemia harbor and express the MLL-AF4 fusion gene. J Exp Med 2009; 206:3131–3141.
Cruet-Hennequart S, Prendergast AM, Barry FP, Carty MP . Human mesenchymal stem cells (hMSCs) as targets of DNA damaging agents in cancer therapy. Curr Cancer Drug Targets 2010; 10:411–421.
Jager M, Schultheis A, Westhoff B, Krauspe R . Osteogenic progenitor cell potency after high-dose chemotherapy (COSS-96). Anticancer Res 2005; 25:947–954.
Mueller LP, Luetzkendorf J, Mueller T, et al. Presence of mesenchymal stem cells in human bone marrow after exposure to chemotherapy: evidence of resistance to apoptosis induction. Stem Cells 2006; 24:2753–2765.
Meads MB, Hazlehurst LA, Dalton WS . The bone marrow microenvironment as a tumor sanctuary and contributor to drug resistance. Clin Cancer Res 2008; 14:2519–2526.
Christensen R, Alsner J, Brandt Sorensen F, et al. Transformation of human mesenchymal stem cells in radiation carcinogenesis: long-term effect of ionizing radiation. Regen Med 2008; 3:849–861.
Nakamizo A, Marini F, Amano T, et al. Human bone marrow-derived mesenchymal stem cells in the treatment of gliomas. Cancer Res 2005; 65:3307–3318.
Khakoo AY, Pati S, Anderson SA, et al. Human mesenchymal stem cells exert potent antitumorigenic effects in a model of Kaposi's sarcoma. J Exp Med 2006; 203:1235–1247.
Lu YR, Yuan Y, Wang XJ, et al. The growth inhibitory effect of mesenchymal stem cells on tumor cells in vitro and in vivo. Cancer Biol Ther 2007; 7:245–251.
Qiao L, Xu Z, Zhao T, et al. Suppression of tumorigenesis by human mesenchymal stem cells in a hepatoma model. Cell Res 2008; 18:500–507.
Ramasamy R, Lam EW, Soeiro I, et al. Mesenchymal stem cells inhibit proliferation and apoptosis of tumor cells: impact on in vivo tumor growth. Leukemia 2007; 21:304–310.
Zhang W . Mesenchymal stem cells in cancer: friends or foes. Cancer Biol Ther 2008; 7:252–254.
Thiery JP, Acloque H, Huang RY, Nieto MA . Epithelial-mesenchymal transitions in development and disease. Cell 2009; 139:871–890.
Huysentruyt LC, Seyfried TN . Perspectives on the mesenchymal origin of metastatic cancer. Cancer Metastasis Rev; 29:695–707.
Matushansky I, Hernando E, Socci ND, et al. A developmental model of sarcomagenesis defines a differentiation-based classification for liposarcomas. Am J Pathol 2008; 172:1069–1080.
Boeuf S, Kunz P, Hennig T, et al. A chondrogenic gene expression signature in mesenchymal stem cells is a classifier of conventional central chondrosarcoma. J Pathol 2008; 216:158–166.
Choi J, Curtis SJ, Roy DM, Flesken-Nikitin A, Nikitin AY . Local mesenchymal stem/progenitor cells are a preferential target for initiation of adult soft tissue sarcomas associated with p53 and Rb deficiency. Am J Pathol 2010; 177:2645–2658.
Neilsen PM, Pishas KI, Callen DF, Thomas DM . Targeting the p53 pathway in Ewing sarcoma. Sarcoma 2011; 2011: 746939.
Li Y, Tanaka K, Fan X, et al. Inhibition of the transcriptional function of p53 by EWS-Fli1 chimeric protein in Ewing Family Tumors. Cancer Lett 2010; 294:57–65.
Ban J, Bennani-Baiti IM, Kauer M, et al. EWS-FLI1 suppresses NOTCH-activated p53 in Ewing's sarcoma. Cancer Res 2008; 68:7100–7109.
Cordon-Cardo C, Latres E, Drobnjak M, et al. Molecular abnormalities of mdm2 and p53 genes in adult soft tissue sarcomas. Cancer Res 1994; 54:794–799.
Oda Y, Yamamoto H, Takahira T, et al. Frequent alteration of p16(INK4a)/p14(ARF) and p53 pathways in the round cell component of myxoid/round cell liposarcoma: p53 gene alterations and reduced p14(ARF) expression both correlate with poor prognosis. J Pathol 2005; 207:410–421.
Barretina J, Taylor BS, Banerji S, et al. Subtype-specific genomic alterations define new targets for soft-tissue sarcoma therapy. Nat Genet 2010; 42:715–721.
Acknowledgements
This work was funded by the CSJA (0108/2007 to RRo) and CICE (P08-CTS-3678 to PM) de la Junta de Andalucía, the FIS/FEDER (PI100449 to PM), the MICINN (PLE-2009-0111 to PM) and the Asociación Española Contra el Cancer (CI110023 to PM). RRo is supported by a fellowship from the Asociación Española Contra el Cancer (AECC). RRu is funded by the MICINN (PTA2009-2107-I).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Rodriguez, R., Rubio, R. & Menendez, P. Modeling sarcomagenesis using multipotent mesenchymal stem cells. Cell Res 22, 62–77 (2012). https://doi.org/10.1038/cr.2011.157
Published:
Issue Date:
DOI: https://doi.org/10.1038/cr.2011.157
Keywords
This article is cited by
-
C/ebpα represses the oncogenic Runx3–Myc axis in p53-deficient osteosarcoma development
Oncogene (2023)
-
3D Models of Sarcomas: The Next-generation Tool for Personalized Medicine
Phenomics (2023)
-
Molecular mechanisms underpinning sarcomas and implications for current and future therapy
Signal Transduction and Targeted Therapy (2021)
-
Mithramycin delivery systems to develop effective therapies in sarcomas
Journal of Nanobiotechnology (2021)
-
Loss of Stag2 cooperates with EWS-FLI1 to transform murine Mesenchymal stem cells
BMC Cancer (2020)