Abstract
Background:
We aimed to assess the connection between chronic inflammatory disorders (CIDs) and Merkel cell carcinoma (MCC).
Methods:
Merkel cell carcinoma cases diagnosed in 1978–2009 were extracted from the Finnish Cancer Registry and controls from the Population Registry. Information on reimbursed CIDs was linked to clinicopathological data including Merkel cell polyomavirus (MCV) status by qPCR and immunohistochemistry for the large T antigen of MCV (LTA), Ki-67 and tumour-infiltrating lymphocytes.
Results:
Chronic inflammatory disorders increased the risk of MCC significantly (odds ratio (OR) 1.39, 95% confidence interval (CI) 1.03–1.88), specifically connective tissue/systemic diseases (OR 1.75, 95% CI 1.09–1.80) and diabetic conditions (OR 1.51, 95% CI 1.03–2.22). Chronic inflammatory disorders associated with larger tumour diameter (P=0.02) and higher Ki-67 expression (P=0.005). The expression of LTA was seen significantly more often in the absence of CIDs (P=0.05).
Conclusions:
Patients with CID are at significantly higher risk for aggressive MCC. Merkel cell polyomavirus positivity is more common in MCC patients unafflicted by CID.
Similar content being viewed by others
Main
Merkel cell polyomavirus (MCV) has a causal role in the tumourigenesis of Merkel cell carcinoma (MCC) (WHO, 2013). Recent evidence implicates two subgroups of MCC tumours: the MCV-positive and MCV-negative group, which differ in their clinical characteristics and pathobiological properties (Leroux-Kozal et al, 2014; Sahi et al, 2014; Veija et al, 2015). Merkel cell polyomavirus positivity of the tumour is associated with a favourable prognosis. However, the prognosis of MCV-positive patients is dependent on the intensity of antiviral immune response (Paulson et al, 2011), and immunosuppression leads to poorer outcome regardless of MCV status (Paulson et al, 2013). Higher numbers of tumour invading CD8+ lymphocytes in MCV-positive tumours correlates with a favourable MCC prognosis (Paulson et al, 2011; Sihto et al, 2012; Harms et al, 2013).
The association between chronic inflammatory disorders (CIDs) and MCC has received less systematic attention than other immunocompromising states such as HIV infection or post-transplant immunosuppression (Arron et al, 2014). We sought to examine the risk for MCC in patients with CIDs in a nationwide case–control setting. Further, we linked the epidemiological data to the clinicopathological data of the MCC cases to assess whether CIDs correlate with the course of the disease or the tumours’ clinical characteristics.
Materials and methods
In phase I, registry data were used in an epidemiological case–control setting to determine whether CIDs affect the risk for MCC. In phase II, MCC patients included in phase I were linked via their personal identity codes to their clinicopathological characteristics.
An Institutional Ethics Committee approved the study plan. The National Institute of Health and Welfare granted its permission to use the information of the Finnish Cancer Registry (FCR). The National Social Insurance institution (SII) provided permission to access drug reimbursement data.
Our group has gathered all paraffinised primary MCC tumour samples available in Finland since 1978. During the past 10 years, we have compiled a database of information on the patient characteristics and course of the disease, as well as tumour characteristics including viral status, tumour genomics and the expression of various immunohistochemical markers. The ongoing MCC projects of our research group continue to utilise this database.
Phase I
Merkel cell carcinoma cases diagnosed in 1978–2009 were identified from the FCR. They were matched for 15 referent persons randomly selected from the Population Register Centre based on the following criteria: (1) same gender and (2) same year of birth. Of these 15 persons, those alive at the time of the MCC diagnosis of the case served as controls.
The SII manages a database that includes specific data on medicine expense reimbursements for chronic diseases. We retrieved data on the SII categories comprising CIDs (Table 1) by using the personal identity codes of the cases and controls as a key. Only diseases prior to MCC diagnosis date were noted.
On the basis of statistical power analysis, the CIDs were grouped together for further calculations according to the affected organ systems (Table 2). A conditional logistic regression model was used to estimate, by means of the odds ratio (OR) with 95 % confidence intervals (95% CI), the risk for MCC.
Phase II
Merkel cell carcinoma patients identified in phase I were linked via personal identity codes to the clinicopathological data of our MCC patient–tumour database. The clinical data comprised the sex of the patients, the pattern of metastatic dissemination and tumour recurrence rates. We examined metastasis in two alternative categories, with a division between local and metastasised disease or local disease, nodal metastasis and systemic metastasis. Combined with immunohistochemistry for Ki-67, these characteristics were used to chart how aggressive the disease was.
The real-time qPCR method used to quantify MCV DNA appears in detail elsewhere (Sihto et al, 2012). We also retrieved previously gathered data on the expression of the large T antigen of MCV (LTA) and Ki-67 for the cases (Sihto et al, 2012). Ki-67 staining was classified into three categories: low (0–32.7% positively staining tumour cell nuclei, 35 tumours), medium (33.6–66% positive nuclei, 36 tumours) and high (61–100% positive nuclei, 36 tumours). We also analysed Ki-67 expression as a continuous variable. The absolute numbers of tumour-infiltrating lymphocytes (CD68+, CD8+ and CD3+) were detected by scanning the whole-tumour sections after histochemical labelling (Sihto et al, 2012) and divided into tertiles for the statistical analysis (Supplementary Table 1).
Pearson’s χ2-test was used for the analysis of categorical variables, and the Mann–Whitney U-test for continuous variables. We used Kaplan–Meier analysis, log-rank test and Wilcoxon test to analyse differences in overall survival between the subgroups defined by inflammatory history and Ki-67 expression (high tertile vs low and medium tertiles). Multivariate survival analysis was conducted with the Cox regression model. The variables consisted of age, gender, history of CID, tumour size, LTA expression and Ki-67 expression.
Results
Phase I: chronic inflammatory disorders and the risk of MCC
The final case–control study set comprised 267 cases and 3 270 controls. Of the 267 MCC patients, 59 (22.1%) were diagnosed with at least one CID, whereas the respective number for the controls was 487 (14.9%). Chronic inflammatory disorders led to significantly higher risk for MCC (OR 1.63, 95% CI 1.19–2.22). The OR was not significantly affected by the gender or age of the MCC patients.
The history of inflammatory systemic/connective tissue disorders significantly increased the risk for MCC (OR 2.01, 95% CI 1.26–3.20), due mainly to rheumatoid conditions, which had an OR of 1.96 (95% CI 1.22–3.15). In addition, diabetic conditions significantly increased the risk for MCC (OR 1.51, 95% CI 1.03–2.22). Neural and gastrointestinal CIDs were rare. The results appear in full in Table 2.
Phase II: chronic inflammatory disorders and features of MCC tumours
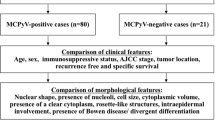
Data on MCV status were available for 142 MCC patients (Supplementary Figure 1), on Ki-67 expression for 107 patients, and on the TILs for 129 patients on the CD68+ stain, 93 on the CD8+ stain and 128 for the CD3+ stain. Information on tumour size and metastasis was available for 134 patients.
Merkel cell polyomavirus DNA was more frequently found in MCC tumours of patients with no CIDs (77% vs 64%, Table 3), although the finding was not statistically significant. The LTA, however, was expressed significantly more often in the absence of CID (71% vs 53%, P=0.05). We observed no significant difference in the viral copy numbers between the groups (Table 3).
The expression of Ki-67 was significantly higher in tumours of MCC patients with CID, with a mean percentage of 63% vs 56% (P=0.005; Supplementary Table 1). The finding was further strengthened by tertile analysis (P=0.007). Chronic inflammatory disorders associated with a larger tumour diameter P=0.02 (Table 3), but the statistical significance disappeared when the tumours were stratified by MCV status (pMCV+=0.06, pMCV−=0.23). Chronic inflammatory disorders did not associate with progression to metastatic disease (Table 3). No significant differences were detected in the overall survival or the TIL numbers between the subgroups (Supplementary Table 1). In the multivariate survival analysis, the only statistically significant variable was age at MCC diagnosis (hazard ratio=1.033, 95% CI 1.002–1.066, P=0.036).
Discussion
We identified a statistically significant increase in the risk for MCC in patients with a history of CIDs. Patients with inflammatory connective tissue diseases and diabetes were at the highest risk for MCC. The results are similar to the relative risk estimates of MCC following rheumatoid arthritis published in the United States (OR 1.39, 95% CI 1.10–1.74) and Sweden (SIR 2.42, 95% CI 0.96–5.01) (Lanoy and Engels, 2010; Hemminki et al, 2012). The tumours of patients with a history of CID were also larger and expressed elevated levels of the proliferation marker Ki-67. This supports the earlier notion of the aggressive course of the disease in immunodefective individuals (Paulson et al, 2013).
Merkel cell carcinoma patients diagnosed with CIDs presented frequently with MCV qPCR-positive tumours. Expression of the LTA occurred in the tumours significantly more often in the absence of CID. The finding is surprising and differs from reports of MCV incidence among the cohort of immunosuppressed MCC patients with chronic lymphocytic leukaemia (Koljonen et al, 2009). This finding seems to stress the difference between stark immunosuppression and more subtle changes in the immune responses in patients with chronic inflammation. One could hypothesise that the immunomodulatory role of chronic inflammation in MCC pathogenesis and predisposition to oncogenesis is more complicated, and may involve tumour surveillance instead of surveillance against virus infection. However, no statistically significant difference was detected in the MCV DNA status between the groups, even though it usually correlates accurately with LTA expression. Confirmation of the finding in other MCC cohorts would be informative.
Tumour-infiltrating lymphocytes are under vigorous scrutiny in MCC due to the new immunomodulating treatment options derived from melanoma research. High CD8+/CD4+ and FoxP3+/CD4+ ratios, as well as CD8+ and CD3+ numbers are associated with good survival (Sihto et al, 2012). This is the first study to look into the TIL spectrum of MCC tumours in immunocompromised patients. We found no significant differences in the numbers of TILs between the patient groups implicating that immunodeficiencies affect the function rather than the trafficking of TILs into MCC tumours.
The results of this study recommend consideration for MCC, especially when dealing with patients with rheumatic and diabetic diseases, as it is more common and more aggressive in these patients. Further studies are needed to elucidate the specific mechanism behind the effect and the interaction between MCV infection and chronic inflammation.
Change history
17 January 2017
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arron ST, Canavan T, Yu SS (2014) Organ transplant recipients with Merkel cell carcinoma have reduced progression-free, overall, and disease-specific survival independent of stage at presentation. J Am Acad Dermatol 71 (4): 684–690.
Harms PW, Patel RM, Verhaegen ME, Giordano TJ, Nash KT, Johnson CN, Daignault S, Thomas DG, Gudjonsson JE, Elder JT, Dlugosz AA, Johnson TM, Fullen DR, Bichakjian CK (2013) Distinct gene expression profiles of viral- and nonviral-associated Merkel cell carcinoma revealed by transcriptome analysis. J Invest Dermatol 133 (4): 936–945.
Hemminki K, Liu X, Ji J, Sundquist J, Sundquist K (2012) Kaposi sarcoma and Merkel cell carcinoma after autoimmune disease. Int J Cancer 131 (3): E326–E328.
Koljonen V, Kukko H, Pukkala E, Sankila R, Bohling T, Tukiainen E, Sihto H, Joensuu H (2009) Chronic lymphocytic leukaemia patients have a high risk of Merkel-cell polyomavirus DNA-positive Merkel-cell carcinoma. Br J Cancer 101 (8): 1444–1447.
Lanoy E, Engels EA (2010) Skin cancers associated with autoimmune conditions among elderly adults. Br J Cancer 103 (1): 112–114.
Leroux-Kozal V, Leveque N, Brodard V, Lesage C, Dudez O, Makeieff M, Kanagaratnam L, Diebold M (2014) Merkel cell carcinoma: histopathological and prognostic features according to the immunohistochemical expression of Merkel cell polyomavirus large T antigen correlated with viral load. Hum Pathol 46 (3): 443–453.
Paulson KG, Iyer JG, Blom A, Warton EM, Sokil M, Yelistratova L, Schuman L, Nagase K, Bhatia S, Asgari MM, Nghiem P (2013) Systemic immune suppression predicts diminished Merkel cell carcinoma-specific survival independent of stage. J Invest Dermatol 133 (3): 642–646.
Paulson KG, Iyer JG, Tegeder AR, Thibodeau R, Schelter J, Koba S, Schrama D, Simonson WT, Lemos BD, Byrd DR, Koelle DM, Galloway DA, Leonard JH, Madeleine MM, Argenyi ZB, Disis ML, Becker JC, Cleary MA, Nghiem P (2011) Transcriptome-wide studies of Merkel cell carcinoma and validation of intratumoral CD8+ lymphocyte invasion as an independent predictor of survival. J Clin Oncol 29 (12): 1539–1546.
Sahi H, Savola S, Sihto H, Koljonen V, Bohling T, Knuutila S (2014) RB1 gene in Merkel cell carcinoma: hypermethylation in all tumors and concurrent heterozygous deletions in the polyomavirus-negative subgroup. APMIS 122 (12): 1157–1166.
Sihto H, Bohling T, Kavola H, Koljonen V, Salmi M, Jalkanen S, Joensuu H (2012) Tumor infiltrating immune cells and outcome of Merkel cell carcinoma: a population-based study. Clin Cancer Res 18 (10): 2872–2881.
Veija T, Sahi H, Koljonen V, Bohling T, Knuutila S, Mosakhani N (2015) miRNA-34a underexpressed in Merkel cell polyomavirus-negative Merkel cell carcinoma. Virchows Arch 466 (3): 289–295.
WHO (2013) IARC monograph on the evaluation of carcinogenic risks to humans. Malaria and Some Polyomaviruses (SV40, BK, JC, and Merkel Cell Viruses) 104, International Agency for Research on Cancer: Lyon, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Sahi, H., Sihto, H., Artama, M. et al. History of chronic inflammatory disorders increases the risk of Merkel cell carcinoma, but does not correlate with Merkel cell polyomavirus infection. Br J Cancer 116, 260–264 (2017). https://doi.org/10.1038/bjc.2016.391
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.391
Keywords
This article is cited by
-
Merkel Cell Carcinoma with Gastric Metastasis, a Rare Presentation: Case Report and Literature Review
Journal of Gastrointestinal Cancer (2023)
-
Merkel-Zell-Karzinom
Der Onkologe (2021)
-
Clinical and molecular characterization of virus-positive and virus-negative Merkel cell carcinoma
Genome Medicine (2020)
-
Immuncheckpointinhibition beim Merkel-Zell-Karzinom
Der Hautarzt (2019)
-
Merkelzellkarzinom
Der Hautarzt (2019)