Abstract
Background:
The prognostic impact of tumour-promoting immune cells in cervical cancer is unclear.
Methods:
Federation of Gynaecology and Obstetrics (FIGO) stage IB and IIA cervical cancer patients (N=101) were assessed for tumour-associated CD66b+ neutrophils and CD163+ macrophages by immunohistochemistry in whole tissue sections using stereology. Results were correlated with previous results on tumour-infiltrating CD3+, CD4+, and CD8+ lymphocytes in the same cohort with recurrence-free survival (RFS) as end point.
Results:
The highest densities of CD66b+ neutrophils and CD163+ macrophages were observed in the peritumoural compartment (median 53.1 cells mm−2 and 1.3% area fraction, respectively). Above median peritumoural and stromal CD66b+ neutrophils and peritumoural CD163+ macrophages were significantly associated with short RFS. Multivariate analysis identified high peritumoural neutrophils (HR 2.27; 95% CI 1.09–4.75; P=0.03), low peritumoural CD8+ lymphocytes (HR 3.67; 95% CI 1.63–8.25; P=0.002), and lymph node metastases (HR 2.70; 95% CI 1.26–5.76; P=0.01) as independent prognostic factors for short RFS, whereas CD163+ macrophages were not significant. An index of combined intratumoral and peritumoral CD66b+ neutrophils to CD8+ lymphocytes had good discriminatory power for each quartile with 5-year RFS of 92%, 80%, 62%, and 44% (P=0.001).
Conclusion:
Tumour-associated neutrophil count is an independent prognostic factor for short RFS in localised cervical cancer. Combining CD66b and CD8 may further improve prognostic stratification. These findings require prospective validation.
Similar content being viewed by others
Main
Squamous cell cervical cancer is a frequent cancer worldwide (Bray et al, 2013). The favourable prognostic impact of lymphocyte infiltration is well documented (Rahir and Moser, 2012), however, the role of tumour-promoting immune cells is largely unknown. Cancer inflammation has emerged as an enabling characteristic for the hallmarks of cancer, and the detrimental effect of tumour-associated innate immune cells has been suggested in a number of cancer types (Mantovani, 2009; Hanahan and Weinberg, 2011), although conflicting results have been published (Souto et al, 2011). In cervical cancer, studies have demonstrated a negative prognostic effect of elevated blood neutrophil and monocyte counts have been demonstrated (Cho and Kim, 2009; Lee et al, 2012b). In addition, blood neutrophil-to-lymphocyte ratio (NLR) has been identified as a poor prognostic factor (Lee et al, 2012a). Suppression of lymphocyte function has been documented for neutrophils (Schmielau and Finn, 2001) and tumour-associated macrophages (TAMs) (Lepique et al, 2009). Matrix metalloproteinase-9 secreted by TAMs, and in particular tumour-associated neutrophils (TANs), has been correlated with poor survival (Ardi et al, 2009). Tumour-associated macrophages have been correlated with accelerated lymphangiogenesis (Schoppmann et al, 2002; Utrera-Barillas et al, 2010), which is perceived as a necessary step for lymph node metastasing. Collectively, these data from cervical cancer indicate a potential harmful role of TANs and TAMs.
Our institution has previously reported poor prognosis for patients with the presence of intratumoural CD66b+ neutrophils in primary (Jensen et al, 2009a) and metastatic renal cell carcinoma (Donskov et al, 2006), as well as poor prognosis for patients with primary melanoma with the presence of intratumoural neutrophils (Jensen et al, 2012) and CD163+ macrophages (Jensen et al, 2009b). In the present study, we assessed CD66b+ neutrophils and CD163+ macrophages in the tumour nests and adjacent stromal tissue in patients with localised cervical cancer. We correlated the assessments with previous findings of tumour-associated CD4+ and CD8+ lymphocyte counts with recurrence-free survival (RFS) as end point.
Material and methods
The study included 102 patients treated with surgery or radiotherapy for cervical squamous cell carcinoma for the International Federation of Gynaecology and Obstetrics (FIGO) stage IB and IIA (Benedet et al, 2000), at Aalborg Hospital from 1990 to 2000 (Table 1). Retrospective clinical sub-classification in stage IB1 and IB2 was not possible. All patients had squamous cell carcinoma. The cohort is identical to the cohort published by Nedergaard et al (2007a); however, one patient was excluded due to the lack of tissue rendering 101 patients for the assessments. Tumour samples were collected from the tumour tissue blocks used for routine pathologic evaluation. We aimed at analysing two sections from separate tissue blocks of each tumour. A previous study in renal cell cancer has shown that analysis of two sections is superior to analysis of a single section, as it significantly decreases the coefficient of variance when taking the variance between tumours and the variation between sections into account (Jensen, Donskov et al, unpublished data). However, in 16 patients (16%) only one section was available. The study was approved by the local Ethics Committee.
Immunohistochemistry
Formalin-fixed paraffin-embedded tumour specimens were sectioned at 2 μm and mounted on glass slides. Primary antibodies were against CD66b (clone G10F5, 1 : 600, no. 555723, BD Biosciences, San Jose, CA, USA), CD34 (clone QBEND10, 1 : 400, Beckman Coulter, Immunotech PN IM0786, Prague, Czech Republic), and CD163 (clone EDHu-1, 1 : 100, MCA 1853, Abd Serotec, Oxford, UK). Immunohistochemistry was performed using a Benchmark XT automated stainer (Ventana Medical Systems, Tucson, AZ, USA). Deparaffinisation, epitope retrieval, and immunostaining were performed according to the instructions of the pathological department by using cell conditioning solutions. Double stainings with CD66b and CD34 were visualised with the ultraVIEW Universal diaminobenzidine detection system (Ventana Medical Systems) and ultraVIEW Universal Alkaline Phosphatase Red Detection Kit (Fast red) detection system (Ventana Medical Systems), respectively. Single staining with CD163 was visualised with ultraVIEW Universal Alkaline Phosphatase Red Detection Kit (Fast red) detection system (Ventana Medical Systems). Positive signals were amplified using ultraVIEW copper, and sections were counterstained with haematoxylin and bluing reagent.
The stainings for CD3+, CD4+, and CD8+ lymphocytes have been described in detail previously (Nedergaard et al, 2007a).
Quantitative evaluation of immunostaining
The evaluation was done using computer-assisted sampling (newCAST software, Visiopharm, Hoersholm, Denmark) applying statistically unbiased stereological sampling of fields of view (Gundersen et al, 1988a, 1988b). Whole slides were scanned at a maximum resolution of × 20 using a whole slide scanner (NanoZoomer 2.0, Hamamatsu Photonics, Hamamatsu City, Japan). Digital images were then imported into newCAST. The total tumour area visible and adjacent tumour-associated stroma at low resolution was outlined as region-of-interest. Areas of necrosis or artefacts were ignored. The quantitative histological analysis was done by one observer blinded to all clinical features and previous lymphocyte counts.
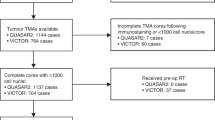
Double staining of CD66b and CD34 allowed for the distinction between intra- and extravascular neutrophil localisation as previously described (Jensen et al, 2009a, 2012). Neutrophils and macrophages were further classified according to tumour compartment as located in tumour nests, peritumoural (i.e., in the stroma at the migrating border of tumour nests) (Figure 1), or stromal as previously described by Nedergaard et al (2007b). An area of stroma was denoted peritumoural, if at least one epithelial malignant cell was observed in the field of view inside a sampling frame. If no tumour cells were observed the area was denoted as stromal. For estimation of the density of CD66b+ neutrophils (Figure 1A) the first counting frame was sampled by the software at random, and subsequently a mean of 64 counting frames (each 40 480 μm2) were sampled in the total tumour area in a systematic manner (Gundersen et al, 1988a) at a total magnification of 1556 ( × 40 lens). Individual neutrophil profiles were counted when a neutrophil nucleus was clearly visible along with a surrounding positive IHC signal. For assessment of CD163+ macrophages (Figure 1B), point counting (Kamper et al, 2011) was applied to estimate the area fraction of CD163+ immunostains per viable tumour area at a magnification of 1556 ( × 40 lens). Point counting of CD163 immunostains was chosen as the cell borders of individual macrophages could not be outlined with sufficient precision. A mean of 28 fields of visions were assessed per tumour section. Areas of necrosis or artefacts were ignored. This stereological approach with a single section from each tumour tissue block only allows for estimation of two-dimensional cell profiles either as number or area fraction. Assessment of number of CD3+, CD4+, and CD8+ lymphocytes were performed with identical stereological approach as for CD66b+ neutrophil estimation and has been described in detail previously (Nedergaard et al, 2007a).
(A ) Representative example of CD66b+/CD34+ staining (20x lens) with tumour nest neutrophil (black thin arrow) and peritumoural neutrophil (white thin arrow). An unbiased counting frame is applied. (B) CD163+ immunostaining (20x lens) illustrating tumour nest macrophage (black fat arrow) and peritumoural macrophages (white fat arrow). A counting grid is applied.
Heterogeneity and reproducibility
Heterogeneity between paired sections from the same patient was modest, as a significant concordance was observed for neutrophil count peritumourally (Paired T-test correlation=0.6; P=0.0001) with the paired t-test revealing no significant differences between samples (P=0.7). Likewise, for macrophages peritumourally we observed a paired T-test correlation of 0.69 with no significant differences between samples (P=0.08). Intraobserver reproducibility of variables was tested in a systematic random sample of every 10th case (N=10), ranked according to neutrophil density. A high reproducibility was observed for neutrophils in all compartments (Spearman ρ>0.80; P<0.0001).
Statistics
Follow-up was median 9.8 years and clinical features (Table 1) were as previously published (Nedergaard et al, 2007a). Correlation between paired sections was tested with paired samples T-test. Intraobserver reproducibility of variables was tested with Spearman rank test. For all cell assessments the median was used as cutoff point. Survival distributions were estimated using the Kaplan–Meier method and the relationship between survival and each parameter was analysed with the log-rank test. A Cox proportional hazards model was created to identify independent predictors of RFS, including factors with a P-value <0.01 in univariate analyses. On the basis of the number of patients in the cohort and the number of events we included a maximum of five variables in the multivariate analysis (Vittinghoff and McCulloch, 2007): peritumoral CD66b+ neutrophils above median, peritumoral CD163+ macrophages above median, peritumoral CD8+ lymphocytes below median, peritumoral CD4+ lymphocytes below median, and presence of lymph node metastases. Statistical analyses were performed using SPSS version 20.0 (SPSS, Chicago, IL, USA) statistical software. All tests were two-sided and P-values <0.05 were considered statistically significant.
Results
Patient characteristics
Characteristics of the 101 cervical cancer patients are listed in Table 1. For patients alive minimum follow-up was at least 5 years. Overall, 10-year RFS rate was 67% for stage IB and 70% for stage IIA.
Tumour-infiltrating neutrophils, macrophages, and lymphocytes correlated with RFS
The number of intravascular neutrophils was negligible (mean absolute count 0). The median densities of neutrophils in tumour nests, peritumoural, and stromal were 23.2 cells mm−2 (range 0–939), 53.1 cells mm−2 (range 1.7–677), and 28.3 cells mm−2 (range 0–780), respectively. The median area fraction of macrophages in tumour nests, peritumoural, and stromal were 0.22% (0–12%), 1.3% (0–17%), and 0.73% (0–9.4%), respectively.
A density of CD66b+ neutrophils above median in the peritumoural compartment and stromal compartment was significantly associated with short RFS (P=0.039 and P=0.011, respectively) (Figure 2), whereas neutrophils within the tumour nests were not (P=0.23). For CD163+ macrophages assessments, a density above median in the peritumoural compartment was significantly associated with short RFS (P=0.042) (Figure 2). The density of CD163+ macrophages in the stroma or intratumoural compartments was not significantly associated with RFS. The highest rate of recurrence was noted for patients with the highest density (quartile 4) of neutrophils and macrophages in all three compartments (Table 2). The 5-year RFS was 52% for patients with peritumoural neutrophil in the fourth quartile compared with 76% for patients with peritumoral neutrophils in the first quartile. Likewise, the 5-year RFS was 60% for patients with peritumoural macrophages density in the fourth quartile compared with 80% for patients with peritumoral macrophages in the first quartile. Higher median densities of peritumoral macrophages were observed in patients with lymph node metastasing with a median area fraction of 2.7% for patients with lymph node metastases vs 1.1% for patients without lymph node metastases (Mann–Whitney P=0.004). However, the two groups were overlapping and no optimal cutpoint could be established. The results of tumour-infiltrating lymphocytes in these patients and the correlation with RFS have previously been published (Nedergaard et al, 2007a). Low peritumoural CD4+ and CD8+ lymphocyte counts stratified at median values were statistically significantly correlated with short RFS (P⩽0.03).
Multivariate analysis
A multivariate Cox proportional-hazard regression model was used to analyse the relative strength and potential independence of CD4+ lymphocytes, CD8+ lymphocytes, CD66b+ neutrophils, CD163+ macrophages, and lymph node metastases. For comparability, estimates from the peritumoural compartment were chosen for the model. Federation of Gynaecology and Obstetrics stage or age had no significant impact on RFS in univariate analysis in this material and thus were not included in multivariate analysis. High density of peritumoural CD66b+ neutrophils, low density of CD8+ lymphocytes, and lymph node metastases were significant independent predictors of poor RFS (Table 3), whereas low density of CD4+ lymphocytes and high densities of CD163+ macrophages were not significant.
Neutrophil-to-lymphocyte ratio
The prognostic information provided by the peritumoral CD66b+ neutrophil to peritumoral CD8+ lymphocyte ratio was not significantly different from that of individual cell counts (P=0.05). However, as the whole tumor area is much easier definable than individual compartments, we further constructed a ratio based on combined intratumoral and peritumoral counts of CD66b+ neutrophils and CD8+ lymphocytes (i.e., the Tumour Associated-Neutrophil to Lymphocyte Ratio (TA-NLR)). The TA-NLR had excellent discriminatory power for each quartile with 5-year RFS for TA-NLR quartile I (<0.065), II (0.07–0.16), III (0.17–0.36), and IV (>0.364) of 92%, 80%, 62%, and 44%, respectively (P=0.001) (Figure 3).
Discussion
To our knowledge, this is the first study to identify tumour-associated CD66b+ neutrophils as an independent poor prognostic factor for RFS in patients with early-stage cervical cancer. Peritumoural neutrophil counts had good discriminatory power, identifying subgroups with 5-year RFS of 52% and 76%, respectively. Moreover, a simple combined prognostic score incorporating both intratumoral and peritumoral CD66b+ neutrophils to intratumoral and peritumoral CD8+ lymphocytes, that is, TA-NLR, was able to further discriminate patients with particularly poor and good risk (5-year RFS of 44% vs 92%, respectively). Elevated densities of CD163+ macrophages were significantly correlated with the presence of lymph node metastases, but were not independently associated with RFS. Thus, patients with high densities of peritumoral neutrophils, low densities of CD8+ lymphocytes, or high TA-NLR should be considered for closer follow-up or intensified adjuvant treatment because of the higher risk of recurrence. These intratumoral features may also serve as stratification factors in adjuvant trials. However, the results require validation in an independent and larger population.
The interplay between immune cells and tumour microenvironment is an area of intense research. Tumours are composed of an assemblage of various cell types, including cancer cells, cancer stem cells, endothelial cells, fibroblasts, and immune cells, that communicate and collaborate (Hanahan and Weinberg, 2011). A delicate interplay between these cells determines whether a tumour progresses or regresses. Tumour-infiltrating lymphocytes have been demonstrated to be a favourable prognostic feature in cervical cancer and other tumour types (Rahir and Moser, 2012). In the present study, we likewise demonstrated that high numbers of CD8+ T-lymphocytes were independently associated with long RFS. However, a novel hallmark of cancer is the capability to avoid tumour destruction (Hanahan and Weinberg, 2011), and TANs as well as TAMs have the potential to suppress cytotoxic lymphocyte function (Schmielau and Finn, 2001; Lepique et al, 2009). High blood neutrophils as well as elevated blood neutrophil-to-lymphocyte ratio have been correlated with poor patient outcome in cervical cancer and other cancers (Yamanaka et al, 2007; Tomita et al, 2012; Lee et al, 2012a). Our observations of high peritumoural CD66b+ neutrophils and low peritumoural CD8+ lymphocytes as independent prognostic factors for short RFS, as well as the TA-NLR demonstrating a strong discriminatory power, are in line with this and suggest a link between peripheral immune cells and the immune cells of the tumour microenvironment, as well as a delicate balance between these immune cells.
Tumour-associated neutrophils and TAMs functionally contribute to multiple hallmarks of cancer (Hanahan and Weinberg, 2011); TANs are involved in tumour initiation, angiogenesis, invasion, progression, and dissemination of cancer (Coussens and Werb, 2001; Di Carlo et al, 2001; Wu et al, 2001; Ishikawa et al, 2008; Fridlender et al, 2009; Tazzyman et al, 2009; Hofman, 2010; Donskov, 2013).
Wu et al (2011) assessed neutrophils localised in the tumour nests, peritumoural, and in the stroma in cervical cancer patients and likewise observed the highest density of neutrophils in the peritumoural area, however, the authors did not correlate their findings with patient outcome. A major novelty of our study is the systematic assessment of the innate immune cells in the different compartments, i.e., tumour, peritumoral and stroma, and the correlation of these cell subsets with recurrence. We confirmed the findings of the highest densities of CD66b+ neutrophils and CD163+ macrophages in the peritumoural compartment, but were only able to demonstrate an independent prognostic capacity for peritumoral CD66b+ neutrophils. This may reflect the importance of neutrophil activity in the migrating tumour border and should be further studied. However, our TA-NLR data suggest that the compartment distribution of immune cells is less important for recurrence assessment and a simple estimate of numbers of CD66b+ neutrophils relative to numbers of CD8+ lymphocytes in the global tumour area may be clinically translatable. We observed higher densities of peritumoral macrophages in patients with lymph node metastases, which suggest an association between macrophage infiltration and lymph node metastasing. Tumour-associated macrophages in the tumour-associated stroma has been shown to relate to the secretion of endothelial growth factors, as well as other factors, which accelerates lymphangiogenesis and can lead to lymph node metastasing (Schoppmann et al, 2002; Utrera-Barillas et al, 2010).
The CD163+ macrophage marker is considered specific for M2-polarised macrophages (Lau et al, 2004; Ambarus et al, 2012). The less specific CD68+ pan-macrophage marker (which may also be expressed by other cell types) have previously been explored in a feasibility study of cervical cancer patients by Nedergaard et al (2007b) and was likewise found not to be significantly associated with tumour recurrence. This supports our results of no independent correlation between macrophages and RFS.
In this study, we employed stereological systematic random sampling methods, and although manual cell counting is labour intensive, the sampling technique is unbiased, efficient and reproducible, and also allows for discrimination of individual cells belonging to the different tumour and stromal compartments. However, limitations to our study are the retrospective design, the small sample size, the lack of some clinical prognostic factors due to the clinical standard between 1990 and 2000, and the lack of HPV subtyping.
In conclusion, elevated CD66b+ TAN count is an independent prognostic factor for short RFS in early-stage cervical cancer. Combining assessments of CD66b+ neutrophils and CD8+ lymphocytes may further improve prognostic stratification. Prospective, larger studies to validate and further elucidate this finding are required.
Change history
28 May 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ambarus CA, Krausz S, van Eijk M, Hamann J, Radstake TR, Reedquist KA, Tak PP, Baeten DL (2012) Systematic validation of specific phenotypic markers for in vitro polarized human macrophages. J Immunol Methods 375 (1-2): 196–206
Ardi VC, Van den Steen PE, Opdenakker G, Schweighofer B, Deryugina EI, Quigley JP (2009) Neutrophil MMP-9 proenzyme, unencumbered by TIMP-1, undergoes efficient activation in vivo and catalytically induces angiogenesis via a basic fibroblast growth factor (FGF-2)/FGFR-2 pathway. J Biol Chem 284 (38): 25854–25866
Benedet JL, Bender H, Jones H 3rd, Ngan HY, Pecorelli S (2000) FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet 70 (2): 209–262
Bray F, Ren JS, Masuyer E, Ferlay J (2013) Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer 132 (5): 1133–1145
Cho H, Kim JH (2009) Multiplication of neutrophil and monocyte counts (MNM) as an easily obtainable tumour marker for cervical cancer. Biomarkers 14 (3): 161–170
Coussens LM, Werb Z (2001) Inflammatory cells and cancer: think different!. J Exp Med 193 (6): F23–F26
Di Carlo E, Forni G, Lollini P, Colombo MP, Modesti A, Musiani P (2001) The intriguing role of polymorphonuclear neutrophils in antitumor reactions. Blood 97 (2): 339–345
Donskov F (2013) Immunomonitoring and prognostic relevance of neutrophils in clinical trials. Semin Cancer Biol ; e-pub ahead of print 10 February 2013, doi:101016/jsemcancer201302001
Donskov F, Hokland M, Marcussen N, Torp Madsen HH, von der Maase H (2006) Monocytes and neutrophils as ‘bad guys’ for the outcome of interleukin-2 with and without histamine in metastatic renal cell carcinoma--results from a randomised phase II trial. Br J Cancer 94 (2): 218–226
Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, Worthen GS, Albelda SM (2009) Polarization of tumor-associated neutrophil phenotype by TGF-beta: ‘N1’ versus ‘N2’ TAN. Cancer Cell 16 (3): 183–194
Gundersen H, Bendtsen T, Korbo L, Marcussen N, Møller A, Nielsen K, Nyengaard J, Pakkenberg B, Sørensen F, Vesterby A others (1988a) Some new, simple and efficient stereological methods and their use in pathological research and diagnosis. APMIS 96: 379–394
Gundersen HJ, Bagger P, Bendtsen TF, Evans SM, Korbo L, Marcussen N, Moller A, Nielsen K, Nyengaard JR, Pakkenberg B, Sorensen FB, Vesterby A, West MJ (1988b) The new stereological tools: disector, fractionator, nucleator and point sampled intercepts and their use in pathological research and diagnosis. APMIS 96 (10): 857–881
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144 (5): 646–674
Hofman PM (2010) Pathobiology of the neutrophil-intestinal epithelial cell interaction: role in carcinogenesis. World J Gastroenterol 16 (46): 5790–5800
Ishikawa K, Takenaga K, Akimoto M, Koshikawa N, Yamaguchi A, Imanishi H, Nakada K, Honma Y, Hayashi J (2008) ROS-generating mitochondrial DNA mutations can regulate tumor cell metastasis. Science 320 (5876): 661–664
Jensen HK, Donskov F, Marcussen N, Nordsmark M, Lundbeck F, von der Maase H (2009a) Presence of intratumoral neutrophils is an independent prognostic factor in localized renal cell carcinoma. J Clin Oncol 27 (28): 4709–4717
Jensen TO, Schmidt H, Moller HJ, Donskov F, Hoyer M, Sjoegren P, Christensen IJ, Steiniche T (2012) Intratumoral neutrophils and plasmacytoid dendritic cells indicate poor prognosis and are associated with pSTAT3 expression in AJCC stage I/II melanoma. Cancer 118 (9): 2476–2485
Jensen TO, Schmidt H, Moller HJ, Hoyer M, Maniecki MB, Sjoegren P, Christensen IJ, Steiniche T (2009b) Macrophage markers in serum and tumor have prognostic impact in American Joint Committee on Cancer stage I/II melanoma. J Clin Oncol 27 (20): 3330–3337
Kamper P, Bendix K, Hamilton-Dutoit S, Honore B, Nyengaard JR, d'Amore F (2011) Tumor-infiltrating macrophages correlate with adverse prognosis and Epstein-Barr virus status in classical Hodgkin's lymphoma. Haematologica 96 (2): 269–276
Lau SK, Chu PG, Weiss LM (2004) CD163: a specific marker of macrophages in paraffin-embedded tissue samples. Am J Clin Pathol 122 (5): 794–801
Lee YY, Choi CH, Kim HJ, Kim TJ, Lee JW, Lee JH, Bae DS, Kim BG (2012a) Pretreatment neutrophil:lymphocyte ratio as a prognostic factor in cervical carcinoma. Anticancer Res 32 (4): 1555–1561
Lee YY, Choi CH, Sung CO, Do IG, Huh S, Song T, Kim MK, Kim HJ, Kim TJ, Lee JW, Kim BG, Bae DS (2012b) Prognostic value of pre-treatment circulating monocyte count in patients with cervical cancer: comparison with SCC-Ag level. Gynecol Oncol 124 (1): 92–97
Lepique AP, Daghastanli KR, Cuccovia IM, Villa LL (2009) HPV16 tumor associated macrophages suppress antitumor T cell responses. Clin Cancer Res 15 (13): 4391–4400
Mantovani A (2009) Cancer: inflaming metastasis. Nature 457 (7225): 36–37
Nedergaard BS, Ladekarl M, Thomsen HF, Nyengaard JR, Nielsen K (2007a) Low density of CD3+, CD4+ and CD8+ cells is associated with increased risk of relapse in squamous cell cervical cancer. Br J Cancer 97 (8): 1135–1138
Nedergaard BS, Nielsen K, Nyengaard JR, Ladekarl M (2007b) Stereologic estimation of the total numbers, the composition and the anatomic distribution of lymphocytes in cone biopsies from patients with stage I squamous cell carcinoma of the cervix uteri. APMIS 115 (12): 1321–1330
Rahir G, Moser M (2012) Tumor microenvironment and lymphocyte infiltration. Cancer Immunol Immunother 61 (6): 751–759
Schmielau J, Finn OJ (2001) Activated granulocytes and granulocyte-derived hydrogen peroxide are the underlying mechanism of suppression of t-cell function in advanced cancer patients. Cancer Res 61 (12): 4756–4760
Schoppmann SF, Birner P, Stockl J, Kalt R, Ullrich R, Caucig C, Kriehuber E, Nagy K, Alitalo K, Kerjaschki D (2002) Tumor-associated macrophages express lymphatic endothelial growth factors and are related to peritumoral lymphangiogenesis. Am J Pathol 161 (3): 947–956
Souto JC, Vila L, Bru A (2011) Polymorphonuclear neutrophils and cancer: intense and sustained neutrophilia as a treatment against solid tumors. Med Res Rev 31 (3): 311–363
Tazzyman S, Lewis CE, Murdoch C (2009) Neutrophils: key mediators of tumour angiogenesis. Int J Exp Pathol 90 (3): 222–231
Tomita M, Shimizu T, Ayabe T, Nakamura K, Onitsuka T (2012) Elevated preoperative inflammatory markers based on neutrophil-to-lymphocyte ratio and C-reactive protein predict poor survival in resected non-small cell lung cancer. Anticancer Res 32 (8): 3535–3538
Utrera-Barillas D, Castro-Manrreza M, Castellanos E, Gutierrez-Rodriguez M, Arciniega-Ruiz de Esparza O, Garcia-Cebada J, Velazquez JR, Flores-Resendiz D, Hernandez-Hernandez D, Benitez-Bribiesca L (2010) The role of macrophages and mast cells in lymphangiogenesis and angiogenesis in cervical carcinogenesis. Exp Mol Pathol 89 (2): 190–196
Vittinghoff E, McCulloch CE (2007) Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 165 (6): 710–718
Wu QD, Wang JH, Condron C, Bouchier-Hayes D, Redmond HP (2001) Human neutrophils facilitate tumor cell transendothelial migration. Am J Physiol Cell Physiol 280 (4): C814–C822
Wu Y, Zhao Q, Peng C, Sun L, Li XF, Kuang DM (2011) Neutrophils promote motility of cancer cells via a hyaluronan-mediated TLR4/PI3K activation loop. J Pathol 225 (3): 438–447
Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M (2007) The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology 73 (3-4): 215–220
Acknowledgements
We thank the laboratory staff at the Department of Pathology for technical assistance. This work was supported by The Danish Cancer Society; The Beckett Foundation; Danish Cancer Research Foundation; Max and Inger Woerzner Foundation; A.P. Møller and wife Chastine Mc-Kinney Møller’s Foundation; Jacob Madsens and Olga Madsens Foundation; The Harboe Foundation; The foundation of the family Kjaersgaards, Sunds; Institute of Clinical Medicine; and Radiumstationens Forskningsfond.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Carus, A., Ladekarl, M., Hager, H. et al. Tumour-associated CD66b+ neutrophil count is an independent prognostic factor for recurrence in localised cervical cancer. Br J Cancer 108, 2116–2122 (2013). https://doi.org/10.1038/bjc.2013.167
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.167
Keywords
This article is cited by
-
Increased genital mucosal cytokines in Canadian women associate with higher antigen-presenting cells, inflammatory metabolites, epithelial barrier disruption, and the depletion of L. crispatus
Microbiome (2023)
-
Clinical Translation of Neutrophil Imaging and Its Role in Cancer
Molecular Imaging and Biology (2022)
-
Neutrophils in cancer carcinogenesis and metastasis
Journal of Hematology & Oncology (2021)
-
29 immune-related genes pairs signature predict the prognosis of cervical cancer patients
Scientific Reports (2020)
-
High density of CD66b in primary high-grade ovarian cancer independently predicts response to chemotherapy
Journal of Cancer Research and Clinical Oncology (2020)