Abstract
The prognostic role of lymphadenectomy during surgery for oesophageal cancer is questioned. We aimed to test whether higher lymph node harvest increases the risk of early postoperative reoperation or mortality. A population-based cohort study including almost all patients who underwent resection for oesophageal cancer in Sweden in 1987–2010. Data were collected from medical records and well-established nationwide Swedish registries. The exposures were number of removed lymph nodes (primary) and number of node metastases (secondary). The main study outcome was reoperation/mortality within 30 days of primary surgery. Relative risks (RRs) with 95% confidence intervals (CIs) were calculated using Poisson regression, adjusted for age, sex, co-morbidity, neoadjuvant therapy, tumour stage, tumour histology, surgeon volume, and calendar period. Among 1,820 participants, the risk of reoperation/mortality did not increase with greater lymph node harvest (RR = 0.98, 95%CI 0.96–1.00, discrete variable) or with greater number of removed metastatic nodes (RR = 1.00, 95% CI 0.95–1.05, discrete variable). Similarly, in stratified analyses within pre-defined categories of tumor stage, surgeon volume and calendar period, increased number of removed nodes or node metastases did not increase the risk of reoperation/mortality. Lymphadenectomy during oesophageal cancer surgery is a safe procedure in the short term perspective.
Similar content being viewed by others
Introduction
Oesophageal cancer is one of the most common and deadly cancer types, and it is the 6th most common cause of cancer death globally1. Surgical resection is the cornerstone of the curatively intended treatment of oesophageal cancer and survival following oesophagectomy has improved over the last few decades2. This improvement is likely due to multiple factors, including improvements in patient selection, perioperative care and centralisation of services. Yet, only 30% of patients survive 5 years following surgery according to recent population-based data3, which stresses the need to identify factors that can further optimise surgical treatment. The extent of lymph node removal might be a relevant factor in this respect. Although based on a limited body of evidence, the use of a fairly extensive (2-field) lymphadenectomy is generally recommended4,5,6. However, the independent prognostic role of lymphadenectomy has been questioned in two recent studies from our research group7,8. The possible lack of an independent association between lymph node harvest and long-term prognosis highlights the need to also examine the role of lymphadenectomy in relation to serious short-term outcomes, caused by postoperative complications. We hypothesized that the additional surgical trauma associated with a more extensive lymphadenectomy increases the risk of postoperative complications requiring reoperation, or leading to mortality within 30 days of oesophagectomy. To test this hypothesis, we conducted a population-based nationwide Swedish cohort study.
Results
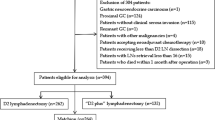
Patients
The entire study cohort included 1 820 patients who underwent surgical resection for oesophageal cancer. Among these, 1 434 patients (79%) had complete data on all study exposures, covariates and outcomes, and were thus selected for the complete case analysis. Since the results were very similar for the entire cohort (imputation of missing data) and the cohort with all data available (complete case analysis), we present only the results for the entire cohort. Characteristics of the patients categorised into quartiles of number of lymph nodes are presented in Table 1. A greater number of removed nodes were associated with higher surgeon volume and more recent calendar period.
Lymph node harvest and 30-day postoperative outcomes
An increased lymph node harvest did not increase the risk of reoperation/mortality within 30 days of surgery (Table 2). When the total number of lymph nodes was analysed as a discrete variable the RR was 0.98 (95% CI 0.96–1.00) and the corresponding RR for number of metastatic nodes was 1.00 (95% CI 0.95–1.05). Comparing the highest quartile of lymph node yield and node metastases with the lowest two quartiles produced RRs of 0.80 (95% CI 0.51–1.26) and 0.85 (95% CI 0.56–1.27), respectively. There were no statistically significant associations between number of lymph nodes or node metastases and any of the six outcomes when analysed separately (Table 2). In analyses stratified by categories of tumour stage, surgeon volume and calendar period, an increased lymph node harvest did not entail an increased risk of reoperation/mortality within 30 days of oesophagectomy (Table 3).
Discussion
This study did not support the hypothesis of an increased risk of 30-day postoperative reoperation or mortality associated with an increased total number of lymph nodes or increased number of metastatic nodes removed.
Methodological advantages of the study include the population-based design with a high participation rate, robust assessment of exposures and outcomes, and the adjustment for several potential confounding factors. These factors counteract bias from selection, misclassification, and confounding, respectively. One can discuss whether reoperation is a good assessment of complications, but we deemed that the validity of this variable was substantially higher than evaluating individual complications that might easily have been missed in the discharge records, while reoperations are not. An obvious confounding factor in this study is surgeon volume, since surgeons with a higher annual volume of oesophagectomy also typically remove more lymph nodes and have better short-term outcomes than less experienced surgeons7,9. Therefore, we adjusted for annual surgeon volume in the multivariable model and also performed stratified analyses among surgeons above and below the median volume. Yet, we cannot entirely exclude residual confounding, e.g. due to rough categorization or misclassification. Another methodological issue is that reoperation and mortality are competing events, since mortality occurring before any potential later reoperation is not accounted for. Therefore, the combined reoperation/mortality outcome was selected as the main study outcome, while the results regarding the separate reoperation outcomes should be interpreted with caution. We used 30-day outcomes to avoid including reoperations for later complications that tend to be less severe, and the use of 30-day mortality rather than 90-day mortality was because this study focused on reoperations but included mortality because of the issue of competing events. Another source of error is missing data on some variables, including the lymph node variables. To account for this we used both imputation analysis (imputation where data were missing) and complete case analysis (including only patients with data on all variables). The similar results using both these analytical approaches indicate that the presence of missing data did not strongly influence the results of the study. Another source of error is misclassification of the assessment of the number of lymph nodes removed, which could differ between histopathologists. Such misclassification should be random, and thus dilute potential associations. However, our previous study on lymph node removal and long-term prognosis revealed strong associations between lymph node metastases and mortality, which lends validity to the node assessment7. Finally, despite the large sample size, the relatively low frequency of the study outcomes reduced the statistical precision, particularly in the subgroup analyses.
Two recent studies from our group indicate a lack of long-term prognostic benefit from a higher lymph node yield during surgery for oesophageal cancer after controlling for surgeon volume7,8. One was based on nationwide Swedish data7, and the other was based on data from a high-volume center for oesophageal cancer surgery in London, the United Kingdom8. On the other hand, the results from the present study indicate that a more extensive lymph node dissection might not be harmful. The lack of increased risk of serious poor short-term outcomes following a more extensive lymphadenectomy needs to be confirmed in future research before any clinical recommendations can be made. Although the volume of resected tissue can vary substantially between two surgeons, it is possible that standardization of the lymph node dissection after having conducted a substantial number of oesophagectomies makes this dissection quite safe. The issues following the additional surgical trauma associated with a more extensive lymphadenectomy might be counteracted by the increasing surgeon experience that tends to parallel the extent of lymph node removal.
In conclusion, this large and population-based cohort study provides no evidence that a more extensive lymphadenectomy increases the risk of reoperation or mortality within 30 days of primary resectional surgery for oesophageal cancer. Thus, lymphadenectomy can be regarded a safe procedure in the short term.
Methods
Design
The study was designed and analyzed according to a detailed study protocol which was developed and completed prior to the initiation of the study. Earlier versions of our nationwide Swedish cohort for oesophageal cancer surgery have been described in detail elsewhere2,7,10. In brief, the study cohort included virtually all patients (98%) who underwent open thoraco-abdominal resection for oesophageal cancer in Sweden during the period 1987 to 2010. The study exposures were the total number of lymph nodes removed and the number of lymph node metastases removed. Data on lymph node harvest were retrieved from the histopathology records of the resected tumour specimens throughout Sweden. The main study outcome was reoperation/mortality occurring within 30 days of primary oesophagectomy. Secondary outcomes were reoperation (for any reason), reoperation for anastomotic leakage, reoperation with laparotomy, reoperation for wound infection, and mortality, all within 30 days of the primary surgery. The data for assessing reoperation and mortality were collected from the Swedish Patient Registry (operation codes) and the Swedish Causes of Death Registry (date of death), respectively. Data on all relevant clinical variables as potential confounders (presented below) were retrieved from medical records, mainly histopathology records and operation charts.
Approvals
The study and the study protocol were approved by the institutional and licensing committee, i.e. the Regional Ethical Review Board in Stockholm (reference number 12/537–32). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was not obtained since this is not required for this type of study (based on registry data and medical records) according to Swedish law.
Statistical analysis
The number of lymph nodes and the number of lymph node metastases were analyzed both as continuous variables and categorical variables (quartiles) in relation to risk of the study outcomes. Since the number of nodes and node metastases was low in the first and second quartiles, these were collapsed into one group. Poisson regression was used to calculate relative risks (RRs) with 95% confidence intervals (CIs). Log-transformed person-time was included in the model as an offset. We assumed that each individual contributed the same weight towards person-time. RRs were adjusted for eight variables that were selected as potential confounders based on previous research: 1) age (continuous variable), 2) sex (categorized into male or female), 3) tumor stage (0-I, II or III-IV), 4) co-morbidity (Charlson co-morbidity index11: 0, 1 or >1), 5) neoadjuvant oncological therapy (yes or no), 6) histological tumour type (adenocarcinoma or squamous cell carcinoma), 7) annual surgeon volume of oesophagectomies (<17 or ≥17), and 8) calendar period (1987–1999 or 2000–2010). Furthermore, six more variables were created with a combination of either number of lymph nodes or the number of lymph node metastases and tumor stage (0-I, II and III-IV), annual surgeon volume of oesophagectomies (<17 and ≥17) and calendar period of surgery (1987–1999 and 2000–2010). These analyses were conducted to evaluate if the association between either number of lymph nodes or the number of lymph node metastases and the outcome reoperation/mortality might change depending on tumour stage, annual surgeon volume and calendar time. To handle missing data on exposures or covariates, we conducted both multiple imputation (using the entire cohort while imputing missing data) and complete case analysis (using only patients for whom all variables were available). Twenty data sets were imputed in the multiple imputation analysis. The monotone logistic method in PROC MI was used on the assumption that the missing data were missing at random (MAR)12. The variables included in the imputation were the eight potential confounders presented above, one of the exposures and one of the outcomes, depending on the model. Furthermore, PROC MIANALYZE was used to combine the results from the analyses of the 20 datasets. The underlying assumption was evaluated by means of sensitivity analyses utilizing pattern-mixture models using the statement ‘missing not at random’. The statistical software SAS version 9.4 (SAS Institute, Cary, NC) was used for all data management and statistical analysis.
Additional Information
How to cite this article: Lagergren, J. et al. Lymphadenectomy and risk of reoperation or mortality shortly after surgery for oesophageal cancer. Sci. Rep. 6, 36092; doi: 10.1038/srep36092 (2016).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Torre, L. A. et al. Global cancer statistics, 2012. CA: a cancer journal for clinicians 65, 87–108, 10.3322/caac.21262 (2015).
Rouvelas, I. et al. Survival after surgery for oesophageal cancer: a population-based study. The lancet oncology 6, 864–870 (2005).
Rutegard, M. et al. Population-based esophageal cancer survival after resection without neoadjuvant therapy: an update. Surgery 152, 903–910, 10.1016/j.surg.2012.03.025 (2012).
Allum, W. H. et al. Guidelines for the management of oesophageal and gastric cancer. Gut 60, 1449–1472, 10.1136/gut.2010.228254 (2011).
Lagarde, S. M., Vrouenraets, B. C., Stassen, L. P. & van Lanschot, J. J. Evidence-based surgical treatment of esophageal cancer: overview of high-quality studies. The Annals of thoracic surgery 89, 1319–1326, 10.1016/j.athoracsur.2009.09.062 (2010).
Rizk, N. P. et al. Optimum lymphadenectomy for esophageal cancer. Annals of surgery 251, 46–50, 10.1097/SLA.0b013e3181b2f6ee (2010).
van der Schaaf, M., Johar, A., Wijnhoven, B., Lagergren, P. & Lagergren, J. Extent of lymph node removal during esophageal cancer surgery and survival. Journal of the National Cancer Institute 107, 10.1093/jnci/djv043 (2015).
Lagergren, J. et al. Extent of Lymphadenectomy and Prognosis After Esophageal Cancer Surgery. JAMA surgery, 1–8, 10.1001/jamasurg.2015.2611 (2015).
Birkmeyer, J. D. et al. Surgeon volume and operative mortality in the United States. The New England journal of medicine 349, 2117–2127, 10.1056/NEJMsa035205 (2003).
Derogar, M., Sadr-Azodi, O., Johar, A., Lagergren, P. & Lagergren, J. Hospital and surgeon volume in relation to survival after esophageal cancer surgery in a population-based study. J Clin Oncol 31, 551–557, 10.1200/JCO.2012.46.1517 (2013).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases 40, 373–383 (1987).
Little, R. & Rubin, D. Statistical analysis with missing data. Wiley-Interscience (2002).
Acknowledgements
The study was funded by the Swedish Research Council (grant number C0324101) and the Swedish Cancer Society (grant number 14 0322).
Author information
Authors and Affiliations
Contributions
Study concept and design: J.L., F.M. and P.L. Acquisition of data: J.L., F.M. and P.L. Analysis and interpretation of data: J.L., F.M. and P.L. Drafting of the manuscript: J.L. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: F.M. Obtained funding: J.L.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Lagergren, J., Mattsson, F., Davies, A. et al. Lymphadenectomy and risk of reoperation or mortality shortly after surgery for oesophageal cancer. Sci Rep 6, 36092 (2016). https://doi.org/10.1038/srep36092
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep36092
This article is cited by
-
Comparisons between minimally invasive and open esophagectomy for esophageal cancer with cervical anastomosis: a retrospective study
Journal of Cardiothoracic Surgery (2020)
-
Chirurgische Strategie in der multimodalen Behandlung des Magen- und Ösophaguskarzinoms
Der Chirurg (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.