Abstract
In this study, we performed a network meta-analysis to compare the outcomes of seven most common surgical procedures to fix DRF, including bridging external fixation, non-bridging external fixation, K-wire fixation, plaster fixation, dorsal plating, volar plating and dorsal and volar plating. Published studies were retrieved through PubMed, Embase and Cochrane Library databases. The database search terms used were the following keywords and MeSH terms: DRF, bridging external fixation, non-bridging external fixation, K-wire fixation, plaster fixation, dorsal plating, volar plating and dorsal and volar plating. The network meta-analysis was performed to rank the probabilities of postoperative complication risks for the seven surgical modalities in DRF patients. This network meta-analysis included data obtained from a total of 19 RCTs. Our results revealed that compared to DRF patients treated with bridging external fixation, marked differences in pin-track infection (PTI) rate were found in patients treated with plaster fixation, volar plating and dorsal and volar plating. Cluster analysis showed that plaster fixation is associated with the lowest probability of postoperative complication in DRF patients. Plaster fixation is associated with the lowest risk for postoperative complications in DRF patients, when compared to six other common DRF surgical methods examined.
Similar content being viewed by others
Introduction
Distal radius fracture (DRF) accounts for 1/6th of all fracture-related emergency room visits and is a common bone fracture of the upper limb occurring in the distal end of the radius1. DRFs have bimodal distribution, with the first peak observed in pediatric patients, where DRF constitutes approximately 25% of all fractures and the second DRF peak is seen in the elderly population, constituting 18% of all fractures in this age group2. DRF incidence is estimated at 26 per 10,000 person-years and it accounts for 72% of all fractures of the forearm and 8 ~ 17% of all fractures of the extremities3. Multiple risk factors for DRFs have been identified, such as gender, environmental conditions (ice and snow), sports activities, vitamin D deficiency, osteoporosis and certain medication (glucocorticosteroids)4. The most common complications of DRFs include tendon rupture, arthrosis, chronic regional pain syndrome (CRPS), neurologic compromise, malunion, nonunion, ulnar impaction, stiffness, loss of rotation and, in rare occasion, compartment syndrome5. Other notable complications of DRFs are pin-track infection (PTI) and carpal tunnel syndrome (CTS)6. Thus, careful attention must be paid to the initial presentation and pattern of injury to ensure successful surgical outcomes and to avoid postoperative complications. Surgical interventions for DRFs include bridge plating, percutaneous Kirschner wire (K-wire) fixation, closed reduction and cast immobilization, fixation with volar or dorsal plates7. Study showed that specific treatment approaches are generally chosen based on DRF injury features and the individual surgeon’s experience with various approaches8.
Bridging external fixation is a popular method used with static fixators to bridge the wrist and immobilize the wrist joint and the fracture, with fracture reduction maintained by ligametotaxis9. Non-bridging external fixation of DRFs is a general technique associated with lower risk of dorsal malunion, compared to bridging external fixation10. K-wire fixation is a minimally invasive procedure for DRF, between conservative treatment and open reduction internal fixation (ORIF), which involves wires passing through the skin and into the bone to hold the fracture in its correct anatomical position11. Plaster fixation with closed reduction is traditionally performed in older DRF patients where exploration is necessary to assess soft tissue injury, if the fracture is transverse or stable on reduction12. Dorsal plating enables direct exposure and reconstruction of the joint with a capsular incision, but requires dissection of extensor retinaculum and plate positioning under this tendon, often resulting in tendonitis or tendon rupture13. Volar plating is increasingly used in elderly DRF patients since it provides better reduction, fracture stability and early mobilization. In addition, compared to dorsal plating, volar plating has better soft-tissue coverage and less tendon irritation14. Dorsal and volar plating with conventional plates report good clinical outcomes in younger patients sustaining variety of complex fractures15. Although DRFs are routinely treated with both surgical and non-surgical approaches, the best approach for DRF treatments remains hotly debated14,16. Thus, studies comparing different treatment approaches for DRF are extremely helpful for both patients and surgeons to understand the risks.
Meta-analysis framework allows pooling outcomes of homogeneous studies on the same topic and but comparisons between more than two interventions are not possible17. On the other hand, a network meta-analysis can indirectly compare three or more interventions and can simultaneously integrate both direct and indirect comparisons of multiple interventions18,19. In this study, we use network meta-analysis to compare the risks of postoperative complications in DRF patients treated with bridging external fixation, non-bridging external fixation, K-wire fixation, plaster fixation, dorsal plating, volar plating and dorsal and volar plating.
Methods and Materials
Search strategy
PubMed, EBSCO and Cochrane Library databases were exhaustively searched (last updated search, May 2015) to identify published randomized clinical trials (RCTs) relevant to seven common surgical interventions in DRF patients. Search terms used for retrieving relevant literature from these databases included combinations of the following keywords and MeSH terms: DRF, bridging external fixation, non-bridging external fixation, K-wire fixation, plaster fixation, dorsal plating, volar plating and dorsal and volar plating.
Inclusion and exclusion criteria
Studies were selected for incorporation into this network meta-analysis if they conformed to the following inclusion criteria: (1) study type: RCTs; (2) interventions: bridging external fixation, non-bridging external fixation, K-wire fixation, plaster fixation, dorsal plating, volar plating and dorsal and volar plating; (3) study subjects: patients clinically or radiologically confirmed as DRF; (4) study outcomes: incidence of CTS, CRPS and PTI rate in DRF patients. Studies were excluded if they (1) lacked data integrity; (2) were not RCTs; (3) were duplicate studies; or (4) involved complex intervention strategies.
Data extraction
Two investigators independently extracted the required data using a standard data collection form. The following information was collected from the selected studies: first author, publication year, country, ethnicity, language, disease, interventions, age, gender, adverse outcomes and number of research subjects. Any disagreements between the two investigators during study selection or data collection were resolved by discussion, re-examination of the data or consulting other investigators.
Statistical analysis
R 3.2.0 software, an open source statistical program, was used to generate the graphical output of the network diagram. Each node represents an intervention, while the node size represents sample size and the width of the connecting line between each node represents the number of studies reporting the comparison. The gemtc installation package of the R software provided a comprehensive set of predictive tools to conduct network meta-analysis in a Bayesian setting.There were four common outcomes for input of Arm- or contrast-level network data: binary, continuous, count or survival. As first described by Lu and Ades, it models relative effects (e.g., log-odds ratio) by setting a generalized linear model (GLM) under Bayesian framework by connecting to JAGS, WinBUGS or OpenBUGS20, which was subsequently extended by others21,22. One of the most important feature of this package is its ability to model inconsistency22,23. The software provides modeling flexibility since users can specify different likelihood and link functions, several Markov-Chain Monte-Carlo (MCMC) sampling options and priors for hyper parameters. Rankograms was utilized for plotting the estimates of rank probabilities. The surface under the cumulative ranking curve (SUCRA), a simple transformation of the mean rank, allows organization of the treatments by hierarchy, both for variance and location of all relative treatment effects24. Higher SUCRA value means a better ranking of the treatment. Multivariate analysis was applied for multiple outcomes in order to explain the correlation between outcomes. Cluster analysis, as an exploratory data mining technique, was used for grouping objects based on their features, with low degree of association between members of different groups and high degree of association between members of the same group25. Using clusterank command, clustered ranking plots can be obtained in STATA program. Outcome1 and outcome2 became the data variables containing the SUCRA scores for all treatments in this network. The different colors correspond to the estimated clusters and were utilized for grouping the treatments according to their similarity for both outcomes.
Results
Baseline characteristics of included studies
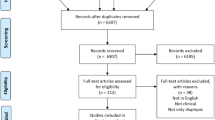
Electronic database search and manual searches retrieved a total of 1249 articles. After excluding 227 duplicate studies, 36 letters and reviews, 12 non-human studies and 209 studies irrelevant to DRF, 765 studies remained for full-text evaluation. Of the 765 studies, 289 articles were excluded since they were not RCTs or were irrelevant to PTI, CRPS and CTS and 11 studies were eliminated for lack of sufficient data or for having incomplete or weakly correlative data. Finally, 19 RCTs met our stringent inclusion/exclusion criteria and these 19 studies were selected for inclusion in our network meta-analysis9,10,14,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41. The 19 studies contained a combined total of 1,805 patients who underwent various surgical treatments for DRF (496 patients with bridging external fixation; 525 patients with non-bridging external fixation; 243 patients with K-wire fixation; 84 patients with plaster fixation; 71 patients with dorsal plating; 128 patients with volar plating; and 258 patients with dorsal and volar plating). With respect to the outcome indictors, 12 studies reported the incidence of CTS, 19 studies reported PTI rate and 17 studies reported the incidence of CRPS. Table 1 shows the baseline characteristics for included studies.
Evidence network
This study included 7 most common surgical treatments for DRF: bridging external fixation, non-bridging external fixation, K-wire fixation, plaster fixation, dorsal plating, volar plating and dorsal and volar plating. The highest incidence of CTS was observed in patients treated with bridge external fixation. In this network meta-analysis, majority of the studies showed direct comparisons for bridge external fixation vs. volar plating, bridge external fixation vs. K-wire fixation and bridging external fixation vs. non-bridging external fixation (Fig. 1a). With respect to PTI rate, patients treated with bridge external fixation, non-bridging external fixation and dorsal and volar plating showed the highest rates. In this network meta-analysis, most of the studies showed direct comparisons for bridge external fixation vs. volar plating, dorsal and volar plating vs. K-wire fixation and bridging external fixation vs. non-bridging external fixation (Fig. 1b). The incidence of CPRS was highest in patients treated with bridge external fixation and non-bridging external fixation. In this network meta-analysis, majority of studies showed direct comparison for bridging external fixation vs. non-bridging external fixation (Fig. 1c).
Test results of inconsistency
Test results of inconsistency for the three adverse outcomes showed that P values for all the direct and indirect comparisons were more than 0.05, indicating the results were consistent between direct and indirect comparisons (Fig. 2a–c). Network meta-analysis can be merged, thus the effect sizes of direct and indirect comparisons can be combined using the consistency model.
Inconsistency test for the seven treatment modalities.
(a) carpal tunnel syndrome; (b) pin-track infection; (c) complex regional pain syndrome; 01: bridging external fixation; 02: non-bridging external fixation; 03: K-wire fixation; 04: plaster fixation; 05: dorsal plating; 06: volar plating; 07: dorsal and volar plating).
The incidence of CTS
The results of network meta-analysis suggested no statistically significant difference in the incidence of CTS in DRF patients treated with non-bridging external fixation, K-wire fixation, plaster fixation, dorsal plating, volar plating and dorsal and volar plating when compared to patients treated with bridging external fixation (non-bridging external fixation: OR = 0.86, 95% CI = 0.17 ~ 4.85; K-wire fixation: OR = 1.82, 95% CI = 0.07 ~ 52.85; plaster fixation: OR = 0.70, 95% CI = 0.09 ~ 5.75; dorsal plating: OR = 0.17, 95% CI = 0.02 ~ 1.54; volar plating: OR = 1.18, 95% CI = 0.18 ~ 6.71; dorsal and volar plating: OR = 0.46, 95% CI = 0.02 ~ 13.66) (Table 2a). Dorsal plating ranked seventh with the highest probability among the seven DRF treatments, suggesting the lowest risk of CTS in patients treated with dorsal plating (Fig. 3a). The highest SUCRA value of 89.4% further confirmed that dorsal plating ranked at the top, with the lowest adverse outcome (Table 3).
Probability ranking plots for the seven treatment modalities.
(a) carpal tunnel syndrome; (b) pin-track infection; (c) complex regional pain syndrome; 1: bridging external fixation; 2: non-bridging external fixation; 3: K-wire fixation; 4: plaster fixation; 5: dorsal plating; 6: volar plating; 7: dorsal and volar plating).
PTI rate
The results of network meta-analysis showed statistically significant differences in PTI rate when DRF patients treated with plaster fixation, volar plating and dorsal and volar plating were compared with patients treated with bridging external fixation (plaster fixation: OR = 0.18, 95% CI = 0.04 ~ 0.67; volar plating: OR = 0.21, 95% CI = 0.05 ~ 0.69; dorsal and volar plating: OR = 0.18, 95% CI = 0.05 ~ 0.67). However, such differences were not found in DRF patients treated with non-bridging external fixation, K-wire fixation and dorsal plating (non-bridging external fixation: OR = 1.97, 95% CI = 0.96 ~ 3.64; K-wire fixation: OR = 0.43, 95% CI = 0.11 ~ 1.85; dorsal plating: OR = 0.24, 95% CI = 0.03 ~ 1.28) (Table 2b). Plaster fixation ranked seventh with the highest probability among the seven DRF treatments, indicating the least risk of PTI in DRF patients treated with plaster fixation (Fig. 3b). The highest SUCRA value of 75.3% further confirmed that the lowest risk for PTI with plaster fixation (Table 3).
The incidence of CRPS
The results of network meta-analysis revealed no statistically significant differences in the incidence of CRPS in DRF patients treated with non-bridging external fixation, K-wire fixation, plaster fixation, dorsal plating, volar plating and dorsal and volar plating when compared to patients treated with bridging external fixation (non-bridging external fixation: OR = 0.67, 95% CI = 0.25 ~ 1.67; K-wire fixation: OR = 1.35, 95% CI = 0.23 ~ 10.08; plaster fixation: OR = 0.60, 95% CI = 0.13 ~ 2.09; dorsal plating: OR = 0.98, 95% CI = 0.18~3.99; volar plating: OR = 1.19, 95% CI = 0.25 ~ 4.99; dorsal and volar plating: OR = 1.31, 95% CI = 0.22 ~ 7.16) (Table 2c). Plaster fixation ranked seventh with the highest probability among the seven DRF treatments, indicating the lowest risk for CRPS in DRF patients treated with plaster fixation (Fig. 3c). SUCRA plots further confirmed that plaster fixation had the highest SUCRA value at 77.3% (Table 3).
Cluster analysis
The results of cluster analysis for CTS and PTI rate showed significantly better outcomes for plaster fixation, dorsal plating, volar plating and dorsal and volar plating in DRF patients (Fig. 4a). The results of cluster analysis for the incidence of CTS and CRPS revealed that plaster fixation and non-bridging external fixation were associated with the best outcomes had better curative effect for DRF patients (Fig. 4b). Cluster analysis for PTI rate and CRPS incidence indicated that plaster fixation had the best outcome in DRF patients (Fig. 4c). Taken together, plaster fixation overall is associated with the lowest risk for postoperative complications in DRF patients.
Discussion
The best treatment choice for DRFs remains a topic of intense debate. In this study, we compared the risk of postoperative complications in patients who underwent seven different surgical approaches to treat DRF. Our network meta-analysis consisted of 1805 DRF patients pooled from 19 RCTs that reported the risk of CTS, PTI rate and CRPS in DRF patients following various surgical interventions. Our results showed that plaster fixation offered the highest probability for avoiding postoperative complications, compared to six other treatment modalities.
Although, DRF patients treated with dorsal plating carried the lowest risk of CTS, the risk for CRPS and PTI was the lowest in DRF patients treated with plaster fixation. Dorsal plating is a well-established treatment for DRF with several advantages, including ease of exposure, visualization of the articular surface and the biomechanical advantage of placing the plate as a dorsal buttress42. However, dorsal plating is associated with extensor tendon complications, which allowed the volar locking plating approach to gain more acceptance43. On the other hand, plaster fixation can be tailored according to the fracture features and is suitable for all types of fracture fixation and external fixation, with little adverse reactions44. Plaster bandage is a commonly used material in plaster fixation, containing dehydrated calcium sulfate powder that can be easily molded after absorbing water and gradually crystallizes to harden in a short time to maintain the original shape45. Also, plaster fixation ensures a relatively uniform pressure on the body’s surface and achieves fracture fixation to a certain extent by limiting muscle contraction46.
Interestingly, bridging and non-bridging external fixation, K-wire fixation, dorsal plating, volar plating and dorsal and volar plating, are described as unsuitable for unstable DRFs and these methods are often associated with poor outcomes. Open reduction and internal fixation was widelyused to fix unstable DRFs in the past, but significant complications have been reported recently, such as rupture of tendons, CTS and CRPS30,47. Closed reduction and external fixation has also been widely used to treat unstable DRFs for several decades andcomplications include loss of reduction, PTI and stiffness48. Notably, the longer the K-wires were left protruding, the greater was the incidence of pin-tract infection, thus it is recommended that K-wires should be buried beneath the skin to reduce infection rate49. Similarly, external fixation group (bridging or non-bridging) contributes to early motion of the wrist and pin loosening and is associated with a higher risk of PTI50. More recently, angle-stable constructs are available for both dorsal and volar plating approaches, offering sufficient stable fixation to allow early mobilization. However, while these two plating techniques appear to show good results in the short term, a definite high risk of tendonitis, tendon rupture and hardware irritation is reported51. Based on the above discussion, plaster fixation carries the lowest risk of postoperative complications, compared to the other six modalities in DRF treatment.
The major merits of this network meta-analysis are: first, due to the absence of head-to-head trials for all the surgical interventions, indirect comparisons were obtained through network analysis. Second, we used consistent measurements across different studies and synthesized the data from selected studies within a single network meta-analysis, avoiding potential selection bias. Third, this updated network meta-analysis provides new insights to address the debate on the best approach by synthesizing the existing evidence and revealing important results related to the clinical care of DRF patients. Our study also has limitations. First, only 19 RCTs were enrolled in our study, the relatively small number of included studies increase the uncertainty of our conclusions. Second, incomplete data existed in some studies, which might bias our results.
In conclusion, our network meta-analysis provides strong evidence that plaster fixation is associated with the lowest risk for postoperative complications in DRF treatment, compared to the six other treatment approaches. However, future RCTs that are better designed and containing larger sample size will be needed to confirm our findings and begin testing clinical applications.
Additional Information
How to cite this article: Qiu, W.-J. et al. The comparative risk of developing postoperative complications in patients with distal radius fractures following different treatment modalities. Sci. Rep. 5, 15318; doi: 10.1038/srep15318 (2015).
References
Christen, D. et al. Improved fracture risk assessment based on nonlinear micro-finite element simulations from HRpQCT images at the distal radius. J Bone Miner Res. 28, 2601–2608 (2013).
Nellans, K. W., Kowalski, E. & Chung, K. C. The epidemiology of distal radius fractures. Hand Clin. 28, 113–125 (2012).
Asadollahi, S. & Keith, P. P. Flexor tendon injuries following plate fixation of distal radius fractures: a systematic review of the literature. J Orthop Traumatol. 14, 227–234 (2013).
Diamantopoulos, A. P. et al. The epidemiology of low- and high-energy distal radius fracture in middle-aged and elderly men and women in Southern Norway. PLoS One. 7, e43367 (2012).
Niver, G. E. & Ilyas, A. M. Carpal tunnel syndrome after distal radius fracture. Orthop Clin North Am. 43, 521–527 (2012).
Shahid, M. K. & Robati, S. The epidemiology and outcome of open distal radial fractures. J Orthop. 10, 49–53 (2013).
Liporace, F. A., Adams, M. R., Capo, J. T. & Koval, K. J. Distal radius fractures. J Orthop Trauma. 23, 739–748 (2009).
Matschke, S., Marent-Huber, M., Audige, L., Wentzensen, A. & Group LCPS. The surgical treatment of unstable distal radius fractures by angle stable implants: a multicenter prospective study. J Orthop Trauma. 25, 312–317 (2011).
Wilcke, M. K., Abbaszadegan, H. & Adolphson, P. Y. Wrist function recovers more rapidly after volar locked plating than after external fixation but the outcomes are similar after 1 year. Acta Orthop. 82, 76–81 (2011).
Hayes, A. J., Duffy, P. J. & McQueen, M. M. Bridging and non-bridging external fixation in the treatment of unstable fractures of the distal radius: a retrospective study of 588 patients. Acta Orthop. 79, 540–547 (2008).
Rozental, T. D. et al. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am. 91, 1837–1846 (2009).
Chung, K. C., Shauver, M. J. & Birkmeyer, J. D. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 91, 1868–1873 (2009).
Wei, J., Yang, T. B., Luo, W., Qin, J. B. & Kong, F. J. Complications following dorsal versus volar plate fixation of distal radius fracture: a meta-analysis. J Int Med Res. 41, 265–275 (2013).
Chappuis, J., Boute, P. & Putz, P. Dorsally displaced extra-articular distal radius fractures fixation: Dorsal IM nailing versus volar plating. A randomized controlled trial. Orthop Traumatol Surg Res. 97, 471–478 (2011).
Blythe, M., Stoffel, K., Jarrett, P. & Kuster, M. Volar versus dorsal locking plates with and without radial styloid locking plates for the fixation of dorsally comminuted distal radius fractures: A biomechanical study in cadavers. J Hand Surg Am. 31, 1587–1593 (2006).
Arora, R. et al. A comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 23, 237–242 (2009).
Peruzzi, M. et al. A network meta-analysis on randomized trials focusing on the preventive effect of statins on contrast-induced nephropathy. Biomed Res Int. 2014, 213239 (2014).
Sutton, A., Ades, A. E., Cooper, N. & Abrams, K. Use of indirect and mixed treatment comparisons for technology assessment. Pharmacoeconomics. 26, 753–767 (2008).
Liao, W. C. et al. Adjuvant treatments for resected pancreatic adenocarcinoma: a systematic review and network meta-analysis. Lancet Oncol. 14, 1095–1103 (2013).
Lu, G. & Ades, A. E. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 23, 3105–3124 (2004).
Dias, S., Sutton, A. J., Ades, A. E. & Welton, N. J. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making. 33, 607–617 (2013).
Dias, S., Welton, N. J., Caldwell, D. M. & Ades, A. E. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 29, 932–944 (2010).
van Valkenhoef, G. et al. Automating network meta-analysis. Res Synth Methods. 3, 285–299 (2012).
Salanti, G., Ades, A. E. & Ioannidis, J. P. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 64, 163–171 (2011).
Chaimani, A., Higgins, J. P., Mavridis, D., Spyridonos, P. & Salanti, G. Graphical tools for network meta-analysis in STATA. PLoS One. 8, e76654 (2013).
Abramo, A., Kopylov, P., Geijer, M. & Tagil, M. Open reduction and internal fixation compared to closed reduction and external fixation in distal radial fractures: a randomized study of 50 patients. Acta Orthop. 80, 478–485 (2009).
Aktekin, C. N. et al. Comparison between external fixation and cast treatment in the management of distal radius fractures in patients aged 65 years and older. J Hand Surg Am. 35, 736–742 (2010).
Atroshi, I. et al. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: a randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 77, 445–453 (2006).
Egol, K. et al. Bridging external fixation and supplementary Kirschner-wire fixation versus volar locked plating for unstable fractures of the distal radius: a randomised, prospective trial. J Bone Joint Surg Br. 90, 1214–1221 (2008).
Grewal, R., MacDermid, J. C., King, G. J. & Faber, K. J. Open reduction internal fixation versus percutaneous pinning with external fixation of distal radius fractures: a prospective, randomized clinical trial. J Hand Surg Am. 36, 1899–1906 (2011).
Grewal, R., Perey, B., Wilmink, M. & Stothers, K. A randomized prospective study on the treatment of intra-articular distal radius fractures: open reduction and internal fixation with dorsal plating versus mini open reduction, percutaneous fixation and external fixation. J Hand Surg Am. 30, 764–772 (2005).
Kreder, H. J. et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomised, controlled trial. J Bone Joint Surg Br. 87, 829–836 (2005).
Krishnan, J., Wigg, A. E., Walker, R. W. & Slavotinek, J. Intra-articular fractures of the distal radius: a prospective randomised controlled trial comparing static bridging and dynamic non-bridging external fixation. J Hand Surg Br. 28, 417–421 (2003).
Leung, F., Tu, Y. K., Chew, W. Y. & Chow, S. P. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radial fractures. A randomized study. J Bone Joint Surg Am. 90, 16–22 (2008).
McQueen, M. M. Redisplaced unstable fractures of the distal radius. A randomised, prospective study of bridging versus non-bridging external fixation. J Bone Joint Surg Br. 80, 665–669 (1998).
McQueen, M. M., Hajducka, C. & Court-Brown, C. M. Redisplaced unstable fractures of the distal radius: a prospective randomised comparison of four methods of treatment. J Bone Joint Surg Br. 78, 404–409 (1996).
Schmelzer-Schmied, N., Wieloch, P., Martini, A. K. & Daecke, W. Comparison of external fixation, locking and non-locking palmar plating for unstable distal radius fractures in the elderly. Int Orthop. 33, 773–778 (2009).
Westphal, T., Piatek, S., Schubert, S. & Winckler, S. Outcome after surgery of distal radius fractures: no differences between external fixation and ORIF. Arch Orthop Trauma Surg. 125, 507–514 (2005).
Wong, T. C. et al. Casting versus percutaneous pinning for extra-articular fractures of the distal radius in an elderly Chinese population: a prospective randomised controlled trial. J Hand Surg Eur Vol. 35, 202–208 (2010).
Wright, T. W., Horodyski, M. & Smith, D. W. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg Am. 30, 289–299 (2005).
Xu, G. G., Chan, S. P., Puhaindran, M. E. & Chew, W. Y. Prospective randomised study of intra-articular fractures of the distal radius: comparison between external fixation and plate fixation. Ann Acad Med Singapore. 38, 600–606 (2009).
Matzon, J. L., Kenniston, J. & Beredjiklian, P. K. Hardware-related complications after dorsal plating for displaced distal radius fractures. Orthopedics. 37, e978–982 (2014).
Florin, M., Arzdorf, M., Linke, B. & Auer, J. A. Assessment of stiffness and strength of 4 different implants available for equine fracture treatment: a study on a 20 degrees oblique long-bone fracture model using a bone substitute. Vet Surg. 34, 231–238 (2005).
Bahari-Kashani, M. et al. Outcomes of pin and plaster versus locking plate in distal radius intraarticular fractures. Trauma Mon. 17, 380–385 (2013).
Gloyer, M. A., Frei, H. C., Hotz, T. K. & Kach, K. P. Osteosynthesis of traumatic manubriosternal dislocations and sternal fractures with a 3.5/4.0 mm fixed-angle plate (LCP). Arch Orthop Trauma Surg. 131, 1261–1266 (2011).
Peng, B., Wang, J. & Mao, F. [Comparison of efficacy between the surgical treatment and plaster external fixation for treatment of unstable distal radius fractures]. Zhongguo Gu Shang. 26, 41–46 (2013).
Jeudy, J. et al. Treatment of complex fractures of the distal radius: a prospective randomised comparison of external fixation ‘versus’ locked volar plating. Injury. 43, 174–179 (2012).
Wang, J. et al. Open reduction and internal fixation versus external fixation for unstable distal radial fractures: a meta-analysis. Orthop Traumatol Surg Res. 99, 321–331 (2013).
Lakshmanan, P., Dixit, V., Reed, M. R. & Sher, J. L. Infection rate of percutaneous Kirschner wire fixation for distal radius fractures. J Orthop Surg (Hong Kong). 18, 85–86 (2010).
Gradl, G. et al. Non-bridging external fixation employing multiplanar K-wires versus volar locked plating for dorsally displaced fractures of the distal radius. Arch Orthop Trauma Surg. 133, 595–602 (2013).
Windolf, M., Schwieger, K., Ockert, B., Jupiter, J. B. & Gradl, G. A novel non-bridging external fixator construct versus volar angular stable plating for the fixation of intra-articular fractures of the distal radius—a biomechanical study. Injury. 41, 204–209 (2010).
Author information
Authors and Affiliations
Contributions
X.-D.Z. and X.-Z.T. wrote the main manuscript text, W.-J.Q., Y.-F.L., Y.-H.J. and W.X. collect the data, H.-L.Z. and G.-B.W. prepared all tables, Y.-Q.J. and S.-C.Z. prepared all figures, F.-F.Z. and H.-M.L. helped to draft the manuscript. All authors reviewed the manuscript
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Qiu, WJ., Li, YF., Ji, YH. et al. The comparative risk of developing postoperative complications in patients with distal radius fractures following different treatment modalities. Sci Rep 5, 15318 (2015). https://doi.org/10.1038/srep15318
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep15318
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.