Abstract
Our study aims to estimate the prevalence of surgical site infections (SSI) following open reduction and internal fixation (ORIF) for mandibular fractures and to determine the effect of potential moderators on it. A systematic literature search (Medline and Scopus databases) was conducted independently by two reviewers. The pooled prevalence with 95% confidence intervals was estimated. Quality assessment as well as outlier and influential analysis were performed. Additionally, subgroup and meta-regression analysis were conducted in order the effect of categorical and continuous variables on the estimated prevalence to be investigated. In total, seventy-five eligible studies (comprising a sum of 5825 participants) were included in this meta-analysis. The overall prevalence of SSI following ORIF for mandibular fractures was estimated as high as 4.2% (95% CI 3.0–5.6%) with significant heterogeneity between studies. One study was identified to be critically influential. In the subgroup analysis, the prevalence was 4.2% (95% CI 2.2–6.6%) among studies conducted in Europe, 4.3% (95% CI 3.1–5.6%) among studies conducted in Asia and higher among those conducted in America (7.3%) (95% CI 4.7–10.3%). It is important for healthcare professionals to be aware of the etiology of these infections, despite the relatively low rate of SSI in these procedures. However, further, well-designed prospective and retrospective studies need to be conducted in order this issue to be fully clarified.
Similar content being viewed by others
Introduction
The fractures of the mandible are one of the most common types of facial traumas requiring surgical intervention1. They can be related to several types of injuries such as assaults and accidents2,3 and are mostly noticed in middle-aged males4. The most common fracture site is the condyle, accounting approximately for 25.0% to 35.0% of all mandibular fractures4. Severe fractured cases could be led to life-threatening situations such as airway obstruction and major hemorrhage5 and therefore, should be recognized and treated immediately.
The treatment is usually performed by oral and maxillofacial surgeons (OMFS) or other relevant surgical specialties in hospital settings, and can be either, closed, or open reduction and internal fixation (ORIF)2,3,5,6. ORIF is generally considered both effective and safe procedure. Yet, various perioperative events, such as inferior alveolar nerve injury, temporomandibular joint disorders, hemorrhage, surgical site infection (SSI), nonunion of the osseous segments, bone necrosis, soft tissue injury, malocclusion, abscess, and hardware exposure may occur7,8,9,10.
Surgical site infection (SSI), defined by CDC as a nosocomial infection following a surgical procedure that occurs near the surgical site within 30 days following surgery (or up to 90 when a medical implant is involved), is associated, according to several studies11,12, with significant poor surgical outcome as well as considerable personal and health care cost13. SSI can be classified as superficial incisional, deep incisional, and organ/space11. The reported rate of SSI following ORIF for mandibular fractures varies considerably in the scientific literature14,15,16,17. Therefore, the aim of the current study is to report a more precise estimation of the prevalence of SSI after ORIF for mandibular fractures, by meta analyzing the available data from the scientific literature.
Methods
Search strategy
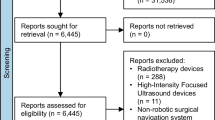
A literature search of Medline (PubMed search engine) and Scopus databases was conducted through an inception up to February 26, 2023, based on the PRISMA guidelines (Fig. 1)18. The PRISMA checklist can be found in Supplementary materials (Supplementary Table 1). The literature search was independently performed by two reviewers using a combination of the following keywords: “mandibular”, “mandible”, “jaw”, “fractures”, “open reduction and internal fixation”, “ORIF”, “surgical site infection”, “surgical wound infection”, “ssi”, “prevalence”, “incidence”, “rate”. The reference lists of all identified eligible studies were evaluated for potentially missed articles throughout the initial literature search. Following the aforementioned procedure, all studies were stored in the Zotero reference management software (version 6.0.18) and the duplicate citations were removed19. The remaining articles were independently screened by two investigators to identify the studies that met the inclusion criteria. The study selection was conducted in two stages. First, article titles and abstracts were reviewed and those that did not meet the inclusion/exclusion criteria were removed. Secondly, full texts of the remaining articles were retrieved and evaluated. If an absence in studies selection was notified, the final decision was reached by team consensus.
Criteria for study selection and data extraction
Articles that examined specifically the prevalence rates of SSI following ORIF procedures for mandibular fractures were included with no restriction on publication date. Case reports, case series with less than ten participants, review articles, randomized clinical trials20,21, animals studies, letters to the editor, books, expert opinion, conference abstracts, studies with no full-text available, studies not written in English, articles without adequate (at least one month postoperative) or unspecified follow-up period22,23,24,25,26,27,28, studies regarding pediatric population17,29, studies conducting in Africa30, articles with unspecified type of infection, studies regarding non mandibular fractures31, studies regarding solely SSI in population with comorbidities (e.g. diabetes melitus, autoimmune diseases), articles containing data derived from surveillance databases and articles investigating postoperative infections per fracture32,33,34,35 were excluded. In articles with overlapping populations, the most recent or most complete publication was considered eligible. The following variables were obtained from each study: the first author’s name, year of publication, study design, continent of origin, study period, total patients, fractures patients ratio, proportion of males, mean age, and patients with postoperative infections.
Quality assessment
Quality appraisal was independently performed by two investigators using the National Heart, Lung, and Blood Institute (NHLBI) Quality Assessment Tools. The NHLBI quality assessment tool for Observational Cohort and Cross-Sectional Studies was employed. Each study was assessed for potential flaws in accordance the methodology or the implementation of each survey that could jeopardize internal validity. For each of the fourteen questions, investigators could select one of the following answers: “yes”, “no”, “cannot determine” (e.g., data were unclear or contradictory) or “not reported” (e.g., missed data) or “not applicable” (e.g., not relevant question regarding this type of study). Study quality was defined as “low”, “moderate” or “high” risk of bias36.
Statistical analysis
Statistical analysis was carried out using RStudio (version: 2022.12.0 + 353) software (RStudio Team37. The meta-analysis was conducted through metafor package38. The DerSimonian and Laird random-effects model was used to estimate the pooled prevalence and its respective 95% confidence intervals (CI). Freeman-Tukey double arscine transformation was performed39. Heterogeneity presence between studies was evaluated through visual inspection of the forest plot and by using the Cochran’s Q statistic and its respective p value. The Higgins I2 statistic and its respective 95% CI were used for quantifying the magnitude of true heterogeneity in effect sizes. An I2 value of 0–40%, 30–60%, 50–60% and 75–100% indicated not important, moderate, substantial and considerable heterogeneity, respectively. To determine if the potential outlying effect sizes were also influential, screening for externally studentized residuals with z-values larger than two in absolute value and leave-one-out diagnostics were performed40. Due to high heterogeneity remaining, subgroup and meta-regression analysis were performed. In the conducted subgroup analysis, the continent of origin was chosen as the categorical moderator on effect sizes. In the performed meta-regression analysis with continuous variables, the year of publication, the proportion of males and the mean age were assessed as moderators on effect sizes. Due to paucity of data (less than ten studies for each covariate) regarding the smoking status and other variables (e.g., duration of surgery, alcohol, obesity, surgeon level), these data were not included in this analysis41. Unless otherwise stipulated, the statistical significance was established at p = 0.05 (two-tailed). Tests to evaluate publication bias, such as Egger’s test42, Begg’s test43 and funnel plots, were developed in the context of comparative data. They assume studies with positive results are more frequently published than studies with negative results, however in a meta-analysis of proportions there is no clear definition or consensus about what a positive result is44. Therefore, publication bias in this current meta-analysis was assessed qualitatively.
Results
Results and characteristics of the included studies
In total, seventy-five studies (comprising a sum of 5825 participants) were finally included in this analysis. The descriptive characteristics of them are reported in Table 1. All articles were published from 1989 to 2022 (conducted from 1980 to 2020). Eighteen of them were of cohort design and the remaining ones of cross-sectional. Most of the studies were carried out in Asia, followed by America and Europe. The average percentage of males was 83.4% and the mean age of participants ranged from 22.4 to 42 years (median: 29.7 years). As per the quality assessment, eight studies were estimated as high quality6,7,46,48,52,85,92,102 and the remaining ones, as moderate (Supplementary materials, Supplementary Table 2).
Prevalence of SSI following ORIF for mandibular fractures
A random-effects model analysis yielded an initial overall SSI prevalence following ORIF of 4.5% (95% CI 3.2–6.0%) with considerable between studies heterogeneity I2 = 76% (95% CI 60.5–80.6%, p < 0.001) (Fig. 2). The influence diagnostics and the forest plot illustrating the results of the leave-one-out analysis is presented in Supplementary material (Supplementary Fig. 1, Fig. 2). As per them, the study conducted from Bouchard et al. identified as influential. After the exclusion of the aforementioned study the estimated prevalence was calculated at 4.2% (95% CI 3.0–5.6%) with substantial between studies remaining heterogeneity I2 = 72.3% (95% CI 51.0–75.0%) (p < 0.001).
Subgroup and meta-regression analysis
The forest plot of the subgroup analysis is illustrated in Supplementary material (Supplementary Fig. 3). The prevalence was 4.2% (95% CI 2.2–6.6%) among studies conducted in Europe, 4.3% (95% CI 3.1–5.6%) among studies conducted in Asia and higher among those conducted in America (7.3%) (95% CI 4.7–10.3%). Heterogeneity remained high in studies conducted in America and moderate in those conducted Europe and low among those conducted in Asia. According to the results of the test for subgroup differences a statistically significant finding was noted. In the meta-regression analysis with continuous variables, a statistically significant negative association between age and the odds of SSI after ORIF for mandibular fractures was observed, as illustrated in Supplementary material (Supplementary Table 1).
Discussion
To the best of our knowledge this is the first attempt to evaluate the prevalence of SSI after ORIF for mandibular fractures through a systematic review. Therefore, there are no published data available to compare our estimate with. According to the results of this study, the prevalence of SSI following ORIF for mandibular fractures is estimated at 4.2% (95%CI 3.0%-5.6%) with substantial heterogeneity. The subjectivity of the SSI’s diagnosis among medical doctors, the type of surgery and other potential risk factors such as diabetes, prolonged operative time, obesity, patients’ age, gender, additional procedures, smoking status, alcohol consumption, oral hygiene, perioperative warming and the lack of defined guidelines regarding the antibiotic protocol use may influence the prevalence of SSI following ORIF for mandibular fractures114,115,116,117,118,119. Moreover, significant heterogeneity is expected in prevalence and incidence estimates due to the type of this study (differences in the time and place where included studies were conducted). Therefore, high I2 in the context of proportional meta-analysis does not necessarily mean that data is inconsistent44. In the subgroup analysis, this prevalence varied by the continent of study’s origin, ranging from 4.2% (95% CI 2.2–6.6%) among European studies, to 7.3% (95% CI 4.7–10.3%) among American and 4.3% (95% CI 3.1–5.6%) among Asian ones. Regarding the statistically significant difference in subgroup analysis, due to lack of data, it was not possible to determine the factors associated with it. It is worth emphasizing again that the current studies are observational and have been conducted in different locations, times, and conditions. Additionally, the pathogens that can contaminate surgical wounds, the surgical practices or even the antibiotics used may vary from country to country. Similar, reduction in the prevalence of SSI was found in a recent meta-analysis120. However, this study does not provide a comprehensive representation since it utilizes data from multiple and in many cases unidentified surgical procedures. Regarding the influence of the age in meta-regression analysis, it should be noted that, on the one hand, the mean ages range from 22.4 to 42 years, which means that the majority of the patient related comorbidities (e.g., type 2 diabetes, which occurs above the age of 45121) commonly associated with aging are likely in their early stages or have not yet become evident, thereby implying that their potential influence on surgical outcomes remains limited. On the other hand, it is important to recognize that this result could be influenced by various confounding factors that require further investigation.
According to WHO in low- and middle-income countries, one out of ten patients (11.8%) develop an SSI after a surgical procedure122. ORIF for mandibular fractures can be consider a safe surgical procedure, regardless of the specific nature of this operation. In most SSI, the responsible pathogens originate from the patient's endogenous flora. The oral cavity consists of a unique environment coated with a plethora of bacteria, which form the bacterial biofilm. The oral microbiome can be categorized into two types: the core microbiome, which is common to all individuals and the variable microbiome, which is unique to individuals based on their lifestyle and physiological differences. The normal microbiome is formed by bacteria, fungi, viruses, archaea and protozoa. Among them, the most commonly isolated bacteria are Gram positive Cocci (e.g. Streptococcus, Peptostreptococcus), Gram positive Rods (e.g. Actinomyces, Lactobacillus), Gram negative Cocci (e.g. Moraxella, Veillonella), Gram negative Rods (e.g. Campylobacter, Fusobacterium)123. These bacteria are capable of contaminating oral wounds. In terms of the treatment used for mandibular fractures, Jazayeri et al.124 analyzed data from nine studies (involving 667 patients) found that ORIF is associated with a higher incidence of postoperative infection (relative risk, 3.6; 95% CI 3.9 to 13.8) compared to closed reduction. Regarding the plate and screw system (locking or nonlocking) used, Zhan et al.125 using data from three studies showed no statistical difference in infection rate between groups (Odds Ratio, 0.43; 95% CI 0.13–1.41; p = 0.17). And in another study conducted by Khavanin et al.126 the author based on the available retrospective studies found out that tooth extraction (which located in line of the fracture) during ORIF procedures was not associated with increased risk of SSI.
Even if the prevalence of SSI may be considered low, SSI still remains one of the most frequent types of health care-associated infections. In order the impact of SSI to be minimized, it is mandatory that necessary preventive measures such as, screening for colonization, isolation of patients with multidrug resistant bacteria, decolonization, surgical site preparation, surgical hand preparation, wearing sterile protective equipment and hygiene and aseptic techniques to be followed122,127. To date, there is no consensus regarding the antibiotic regimen used; hence, specific guidelines in country level should be implemented by global organizations, in order inappropriate antibiotic prescribing and the devastating consequences of it, to be avoided. The excess prescription of broad-spectrum chemoprophylaxis leads to antimicrobial resistance, which poses a major threat to public health by increasing mortality around the world, especially in low resources settings. According to a recent systematic review regarding the antibiotics prophylaxis in maxillofacial trauma, preoperative antibiotics were related with lower infection rates while prolonged antibiotic regimens showed no significant benefit128. Moreover, de Jonge et al.129 combining data from fourteen studies (54,552 participants) found out that the administration of antibiotic prophylaxis for more than 120 min prior to the first incision or after the inception of the surgical procedure was associated with higher risk of SSI than administration less than 120 min. Tetanus prophylaxis should also be considered in open mandibular fractures. Pain control should be achieved with acetaminophen, NSAIDs, and/or opioids. Steroids and ice packs are useful for reducing edema3. It is important for healthcare professionals to be aware of the etiology of these infections. Consequently, it is imperative to conduct both prospective and retrospective studies, including observational and interventional approaches, to thoroughly investigate the correlation between SSI following ORIF for mandibular fractures and potential risk factors.
Study’s strengths and limitations
The main strength of the current study was the comprehensive methodology applied for the literature search, study selection, inclusion/exclusion criteria, screening for eligibility, quality assessment and pooling analysis of prevalence data from forty studies. However, the present study had several limitations. It should be noted that the unidentified heterogeneity remained substantial, therefore, the results should be interpreted with caution. The highly heterogenous outcomes across the included studies were expected due to the nature of this type of studies. The subjectivity of the SSI’s diagnosis among medical doctors and other potential risk factors such as diabetes, prolonged operative time, obesity, patients’ age, gender, additional procedures performed, smoking status, alcohol consumption, oral hygiene, perioperative warming, the type of surgery and the lack of defined guidelines regarding the antibiotic protocol used might bias the prevalence of SSI following ORIF for mandibular fractures. Due to limited data (less than ten studies for each covariate) regarding variables such as smoking status, duration of surgery, alcohol, obesity, surgeon level, these variables were excluded from this presented analysis. Moreover, only observational studies written in English language were included resulting in the occurrence of reporting bias. Consequently, the existing evidence may be constrained and lacking comprehensive representation due to the omission of studies composed in languages other than English (e.g. studies carried out and documented in countries where English is not the primary language and which possess limited resources). Only studies from Europe, America, and Asia were finally included in our analysis. Therefore, it is important to note again that the results should be interpreted cautiously due to the limited generalizability of the data and the potential underestimation or overestimation of the prevalence.
Data availability
Literature and Rstudio data are available from the corresponding author on reasonable request.
References
Ludi, E. K., Rohatgi, S., Zygmont, M. E., Khosa, F. & Hanna, T. N. Do radiologists and surgeons speak the same language? A retrospective review of facial trauma. Am. J. Roentgenol. 207(5), 1070–1076. https://doi.org/10.2214/AJR.15.15901 (2016).
Pickrell, B., Serebrakian, A. & Maricevich, R. Mandible fractures. Semin. Plast. Surg. 31(02), 100–107. https://doi.org/10.1055/s-0037-1601374 (2017).
Yuen, H.-W., Hohman, M. H. & Mazzoni, T. Mandible fracture. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK507705/ (2021).
Gerbino, G., Boffano, P. & Bosco, G. F. Symphyseal mandibular fractures associated with bicondylar fractures: A retrospective analysis. J. Oral Maxillofac. Surg. 67(8), 1656–1660. https://doi.org/10.1016/j.joms.2009.03.069 (2009).
Ferneini, E. M. Mandibular fractures. J. Oral Maxillofac. Surg. 79(12), 2603–2605. https://doi.org/10.1016/j.joms.2021.08.264 (2021).
Moreno, J. C., Fernández, A., Ortiz, J. A. & Montalvo, J. J. Complication rates associated with different treatments for mandibular fractures. J. Oral Maxillofac. Surg. 58(3), 273–280. https://doi.org/10.1016/S0278-2391(00)90051-X (2000).
Gutta, R. et al. Outcomes of mandible fracture treatment at an academic tertiary hospital: A 5-year analysis. J. Oral Maxillofac. Surg. 72(3), 550–558. https://doi.org/10.1016/j.joms.2013.09.005 (2014).
Jin, K.-S. et al. Fracture patterns and causes in the craniofacial region: An 8-year review of 2076 patients. Maxillofac. Plast. Reconstr. Surg. 40(1), 29. https://doi.org/10.1186/s40902-018-0168-y (2018).
Nakamura, S., Takenoshita, Y. & Oka, M. Complications of miniplate osteosynthesis for mandibular fractures. J. Oral Maxillofac. Surg. 52(3), 233–238. https://doi.org/10.1016/0278-2391(94)90289-5 (1994).
Ravikumar, C. & Bhoj, M. Evaluation of postoperative complications of open reduction and internal fixation in the management of mandibular fractures: A retrospective study. Indian J. Dent. Res. Off. Publ. Indian Soc. Dent. Res. 30(1), 94–96. https://doi.org/10.4103/ijdr.IJDR_116_17 (2019).
CDC/OID/NCEZID/DHQP. 9 Surgical site infection (SSI) event. [Online] Available at: https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf (2016).
Young, P. Y. & Khadaroo, R. G. Surgical site infections. Surg. Clin. N. Am. 94(6), 1245–1264. https://doi.org/10.1016/j.suc.2014.08.008 (2014).
Badia, J. M. et al. Impact of surgical site infection on healthcare costs and patient outcomes: A systematic review in six European countries. J. Hosp. Infect. 96(1), 1–15. https://doi.org/10.1016/j.jhin.2017.03.004 (2017).
Ardary, W. C. Prospective clinical evaluation of the use of compression plates and screws in the management of mandible fractures. J. Oral Maxillofac. Surg. 47(11), 1150–1153. https://doi.org/10.1016/0278-2391(89)90004-9 (1989).
Guimond, C., Johnson, J. V. & Marchena, J. M. Fixation of mandibular angle fractures with a 2.0-mm 3-dimensional curved angle strut plate. J. Oral Maxillofac. Surg. 63(2), 209–214. https://doi.org/10.1016/j.joms.2004.03.018 (2005).
Kanno, T. et al. Surgical treatment of comminuted mandibular fractures using a low-profile locking mandibular reconstruction plate system. Ann. Maxillofac. Surg. 4(2), 144. https://doi.org/10.4103/2231-0746.147103 (2014).
Kopp, R. W., Crozier, D. L., Goyal, P., Kellman, R. M. & Suryadevara, A. C. Decade review of mandible fractures and arch bar impact on outcomes of nonsubcondylar fractures: Mandible fracture management and outcomes. Laryngoscope 126(3), 596–601. https://doi.org/10.1002/lary.25671 (2016).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ https://doi.org/10.1136/bmj.n71 (2021).
www.zotero.org. (n.d.). Zotero | Your personal research assistant. [Online] Available at: https://www.zotero.org [Accessed 15 Dec. 2022].
Kaushik, S., Ali, I., Dubey, M. & Bajpai, N. 2 mm conventional miniplates with three-dimensional strut plate in mandibular fractures. Ann. Maxillofac. Surg. 10(1), 10. https://doi.org/10.4103/ams.ams_73_19 (2020).
Singh, A. et al. Experience with resorbable plates for fixation of mandible fracture. A prospective study of 10 cases. J. Pharm. Bioallied Sci. 14(5), 845. https://doi.org/10.4103/jpbs.jpbs_22_22 (2022).
Dewi, F., Henry, A. & Bhatia, S. Postoperative radiographs after open reduction and internal fixation of mandibular fractures: Clinical need or unnecessary radiation?. Br. J. Oral Maxillofac. Surg. 54(3), 312–315. https://doi.org/10.1016/j.bjoms.2015.12.019 (2016).
Guy, W. M. et al. ‘Repairing angle of the mandible fractures with a strut plate. JAMA Otolaryngol. Head Neck Surg. 139(6), 592 (2013).
Janaphan, K., Hashem, I., Smith, C., Holmes, S. & Chatzopoulou, D. Periodontal disease as a primary cause of surgical site infection in fractures of the mandible: Is smoking a confounding variable?. Br. J. Oral Maxillofac. Surg. 60(10), 1424–1429. https://doi.org/10.1016/j.bjoms.2022.08.001 (2022).
Kong, T. H., Chung, K. J. & Kim, Y. H. Analysis of the risk factors influencing complications in surgical treatment of mandibular fractures: A retrospective study. J. Cranio Maxillofac. Surg. 50(12), 929–933. https://doi.org/10.1016/j.jcms.2022.12.001 (2022).
Melo, A. R., de Aguiar Soares Carneiro, S. C., Leal, J. L. F. & do Egito Vasconcelos, B. C. Fracture of the atrophic mandible: Case series and critical review. J. Oral Maxillofac. Surg. 69(5), 1430–1435. https://doi.org/10.1016/j.joms.2010.05.078 (2011).
Özer, C., Tamer, Y., Bayram, B. & Pektaş, Z. Ö. Modified Blair approach for the treatment of mandibular condyle fractures. J. Craniofac. Surg. 33(7), 2231–2234. https://doi.org/10.1097/SCS.0000000000008571 (2022).
Schaefer, E. H. & Caterson, E. J. Antibiotic selection for open reduction internal fixation of mandible fractures. J. Craniofac. Surg. 24(1), 85–88. https://doi.org/10.1097/SCS.0b013e318275ef21 (2013).
Colletti, G. et al. Extraoral approach to mandibular condylar fractures: Our experience with 100 cases. J. Cranio Maxillofac. Surg. 42(5), e186–e194. https://doi.org/10.1016/j.jcms.2013.08.005 (2014).
El-Anwar, M. W. & Sweed, A. H. Simple percutaneous transbuccal approach for management of mandibular angular fracture. J. Craniofac. Surg. 28(4), 1035–1037. https://doi.org/10.1097/SCS.0000000000003539 (2017).
Venugopal, M., Sinha, R., Menon, P., Chattopadhyay, P. & Roy Chowdhury, S. Fractures in the maxillofacial region: A four year retrospective study. Med. J. Armed Forces India 66(1), 14–17. https://doi.org/10.1016/S0377-1237(10)80084-X (2010).
Bouchard, C. & Perreault, M.-H. Postoperative complications associated with the retromandibular approach: A retrospective analysis of 118 subcondylar fractures. J. Oral Maxillofac. Surg. 72(2), 370–375. https://doi.org/10.1016/j.joms.2013.08.014 (2014).
Koirala, U. & Subedi, S. Retromandibular transparotid approach for subcondylar mandibular fracture: A retrospective study. Dent. Traumatol. 37(2), 314–320. https://doi.org/10.1111/edt.12626 (2021).
Laughlin, R. M., Block, M. S., Wilk, R., Malloy, R. B. & Kent, J. N. Resorbable plates for the fixation of mandibular fractures: A prospective study. J. Oral Maxillofac. Surg. 65(1), 89–96. https://doi.org/10.1016/j.joms.2005.10.055 (2007).
Saman, M., Kadakia, S. & Ducic, Y. Postoperative maxillomandibular fixation after open reduction of mandible fractures. JAMA Facial Plast. Surg. 16(6), 410–413. https://doi.org/10.1001/jamafacial.2014.543 (2014).
NIH. Study Quality Assessment Tools | National Heart, Lung, and Blood Institute (NHLBI). [Online] Nih.gov. Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Accessed 15 Dec. 2022] (2009).
RStudio Desktop. Available at: https://posit.co/download/rstudio-desktop/ (2022).
Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. https://doi.org/10.18637/jss.v036.i03 (2010).
Miller, J. J. The inverse of the Freeman–Tukey double arcsine transformation. Am. Stat. 32(4), 138–138. https://doi.org/10.1080/00031305.1978.10479283 (1978).
Viechtbauer, W. & Cheung, M.W.-L. Outlier and influence diagnostics for meta-analysis. Res. Synth. Methods 1(2), 112–125. https://doi.org/10.1002/jrsm.11 (2010).
Handbook-5-1.cochrane.org. (n.d.). 9.6.5.1 Ensure that there are adequate studies. [Online] Available at: https://handbook-5-1.cochrane.org/chapter_9/9_6_5_1_ensure_that_there_are_adequate_studies_to_justify.htm [Accessed 27 Dec. 2022].
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109), 629–634. https://doi.org/10.1136/bmj.315.7109.629 (1997).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4), 1088–1101 (1994).
Barker, T. H. et al. Conducting proportional meta-analysis in different types of systematic reviews: A guide for synthesisers of evidence. BMC Med. Res. Methodol. 21(1), 189. https://doi.org/10.1186/s12874-021-01381-z (2021).
Sargent, L. A. & Green, J. F. Plate and screw fixation of selected condylar fractures of the mandible. Ann. Plast. Surg. 28(3), 235–241. https://doi.org/10.1097/00000637-199203000-00006 (1992).
Stone, I. E., Dodson, T. B. & Bays, R. A. Risk factors for infection following operative treatment of mandibular fractures. Plast. Reconstr. Surg. 91(1), 64–68. https://doi.org/10.1097/00006534-199301000-00008 (1993).
Zachariades, N. ‘Complications of treatment of mandibular fractures with compression plates. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 79(2), 150–153 (1995).
Widmark, G., Bågenholm, T., Kahnberg, K.-E. & Lindahl, L. Open reduction of subcondylar fractures. Int. J. Oral Maxillofac. Surg. 25(2), 107–111. https://doi.org/10.1016/S0901-5027(96)80052-X (1996).
Herford, A. S. & Ellis, E. Use of a locking reconstruction bone plate/screw system for mandibular surgery. J. Oral Maxillofac. Surg. 56(11), 1261–1265. https://doi.org/10.1016/S0278-2391(98)90605-X (1998).
Eckelt, U. & Hlawitschka, M. Clinical and radiological evaluation following surgical treatment of condylar neck fractures with lag screws. J. Cranio Maxillofac. Surg. 27(4), 235–242. https://doi.org/10.1016/S1010-5182(99)80035-3 (1999).
Bolourian, R., Lazow, S. & Berger, J. Transoral 2.0-mm miniplate fixation of mandibular fractures plus 2 weeks’ maxillomandibular fixation: A prospective study. J. Oral Maxillofac. Surg. 60(2), 167–170. https://doi.org/10.1053/joms.2002.29813 (2002).
Ellis, E. Outcomes of patients with teeth in the line of mandibular angle fractures treated with stable internal fixation. J. Oral Maxillofac. Surg. 60(8), 863–865. https://doi.org/10.1053/joms.2002.33852 (2002).
Kim, Y.-K. & Kim, S.-G. Treatment of mandible fractures using bioabsorbable plates. Plast. Reconstr. Surg. 110(1), 25–31. https://doi.org/10.1097/00006534-200207000-00006 (2002).
Suzuki, T., Kawamura, H., Kasahara, T. & Nagasaka, H. Resorbable poly-l-lactide plates and screws for the treatment of mandibular condylar process fractures: A clinical and radiologic follow-up study. J. Oral Maxillofac. Surg. 62(8), 919–924. https://doi.org/10.1016/j.joms.2004.01.016 (2004).
Barry, C. P. & Kearns, G. J. Superior border plating technique in the management of isolated mandibular angle fractures: A retrospective study of 50 consecutive patients. J. Oral Maxillofac. Surg. 65(8), 1544–1549. https://doi.org/10.1016/j.joms.2006.10.069 (2007).
Tiwana, P. S., Kushner, G. M. & Alpert, B. Lag screw fixation of anterior mandibular fractures: A retrospective analysis of intraoperative and postoperative complications. J. Oral Maxillofac. Surg. 65(6), 1180–1185. https://doi.org/10.1016/j.joms.2006.11.046 (2007).
Zix, J., Lieger, O. & Iizuka, T. Use of straight and curved 3-dimensional titanium miniplates for fracture fixation at the mandibular angle. J. Oral Maxillofac. Surg. 65(9), 1758–1763. https://doi.org/10.1016/j.joms.2007.03.013 (2007).
Bell, R. B. & Wilson, D. M. Is the use of arch bars or interdental wire fixation necessary for successful outcomes in the open reduction and internal fixation of mandibular angle fractures?. J. Oral Maxillofac. Surg. 66(10), 2116–2122. https://doi.org/10.1016/j.joms.2008.05.370 (2008).
Biglioli, F. & Colletti, G. Transmasseter approach to condylar fractures by mini-retromandibular access. J. Oral Maxillofac. Surg. 67(11), 2418–2424. https://doi.org/10.1016/j.joms.2009.04.066 (2009).
Bui, P., Demian, N. & Beetar, P. Infection rate in mandibular angle fractures treated with a 2.0-mm 8-hole curved strut plate. J. Oral Maxillofac. Surg. 67(4), 804–808. https://doi.org/10.1016/j.joms.2008.08.034 (2009).
Burm, J. S. & Hansen, J. E. The use of microplates for internal fixation of mandibular fractures. Plast. Reconstr. Surg. 125(5), 1485–1492. https://doi.org/10.1097/PRS.0b013e3181d51244 (2010).
Downie, J. J., Devlin, M. F., Carton, A. T. M. & Hislop, W. S. Prospective study of morbidity associated with open reduction and internal fixation of the fractured condyle by the transparotid approach. Br. J. Oral Maxillofac. Surg. 47(5), 370–373. https://doi.org/10.1016/j.bjoms.2008.11.002 (2009).
Bindra, S., Choudhary, K., Sharma, P., Sheorain, A. & Sharma, C. B. Management of mandibular sub condylar and condylar fractures using retromandibular approach and assessment of associated surgical complications. J. Maxillofac. Oral Surg. 9(4), 355–362. https://doi.org/10.1007/s12663-010-0133-5 (2010).
Chen, C.-T., Feng, C.-H., Tsay, P.-K., Lai, J.-P. & Chen, Y.-R. Functional outcomes following surgical treatment of bilateral mandibular condylar fractures. Int. J. Oral Maxillofac. Surg. 40(1), 38–44. https://doi.org/10.1016/j.ijom.2010.09.002 (2011).
Hochuli-Vieira, E., Ha, T. K. L., Pereira-Filho, V. A. & Landes, C. A. Use of rectangular grid miniplates for fracture fixation at the mandibular angle. J. Oral Maxillofac. Surg. 69(5), 1436–1441. https://doi.org/10.1016/j.joms.2010.06.182 (2011).
Li, Z. & Li, Z.-B. Clinical characteristics and treatment of multiple site comminuted mandible fractures. J. Cranio Maxillofac. Surg. 39(4), 296–299. https://doi.org/10.1016/j.jcms.2010.04.009 (2011).
Benech, A., Arcuri, F., Baragiotta, N., Nicolotti, M. & Brucoli, M. Retroauricular transmeatal approach to manage mandibular condylar head fractures. J. Craniofac. Surg. 22(2), 641–647. https://doi.org/10.1097/SCS.0b013e318207f495 (2011).
Gokkulakrishnan, S., Singh, S., Sharma, A. & Shahi, A. K. An analysis of postoperative complications and efficacy of 3-D miniplates in fixation of mandibular fractures. Dent. Res. J. 9(4), 414 (2012).
Höfer, S. H., Ha, L., Ballon, A., Sader, R. & Landes, C. Treatment of mandibular angle fractures—Linea obliqua plate versus grid plate. J. Cranio Maxillofac. Surg. 40(8), 807–811. https://doi.org/10.1016/j.jcms.2012.02.021 (2012).
Kim, B.-K., Kwon, Y.-D., Ohe, J. Y., Choi, Y.-H. & Choi, B.-J. Usefulness of the retromandibular transparotid approach for condylar neck and condylar base fractures. J. Craniofac. Surg. 23(3), 712–715. https://doi.org/10.1097/SCS.0b013e31824dbb35 (2012).
Zhou, J.-H. & Ren, C.-Q. A preauricular long-corniform approach for open reduction and internal fixation of mandibular condylar fractures. J. Cranio Maxillofac. Surg. 41(5), 359–366. https://doi.org/10.1016/j.jcms.2012.10.017 (2013).
Kang, D. R. & Zide, M. The 7-hole angle plate for mandibular angle fractures. J. Oral Maxillofac. Surg. 71(2), 327–334. https://doi.org/10.1016/j.joms.2012.09.015 (2013).
Lee, T., Sawhney, R. & Ducic, Y. Miniplate fixation of fractures of the symphyseal and parasymphyseal regions of the mandible: A review of 218 patients. JAMA Facial Plast. Surg. 15(2), 121–125. https://doi.org/10.1001/jamafacial.2013.307 (2013).
Singh, R. P., Carter, L. M. & Whitfield, P. H. Antimicrobial prophylaxis in open reduction and internal fixation of compound mandibular fractures: A collaborative regional audit of outcome. Br. J. Oral Maxillofac. Surg. 51(5), 444–447. https://doi.org/10.1016/j.bjoms.2012.08.019 (2013).
Pal, U. S., Singh, R. K., Dhasmana, S., Das, S. & Das, S. K. Use of 3-D plate in displaced angle fracture of mandible. Craniomaxillofac. Trauma Reconstr. 6(1), 25–29. https://doi.org/10.1055/s-0032-1332211 (2013).
Rao, J. K. D., Gehlot, N. & Siwach, V. Evaluation of retro mandibular approach to open reduction and internal fixation of condylar fractures: A cross-sectional study. J. Maxillofac. Oral Surg. 13(4), 488–494. https://doi.org/10.1007/s12663-013-0559-7 (2014).
Prasad, R., Thangavelu, K. & John, R. The role of 3D plating system in mandibular fractures: A prospective study. J. Pharm. Bioallied Sci. 5(5), 10. https://doi.org/10.4103/0975-7406.113280 (2013).
Yabe, T., Tsuda, T., Hirose, S. & Ozawa, T. Preauricular transparotid approach to mandibular condylar fractures without dissecting facial nerves. J. Craniofac. Surg. 24(4), 1365–1367. https://doi.org/10.1097/SCS.0b013e318285d9a3 (2013).
Yazdani, J. et al. Mandibular angle fractures: Comparison of one miniplate vs. two miniplates. Trauma Mon. 18(1), 17–20. https://doi.org/10.5812/traumamon.9865 (2013).
Chhabaria, G. et al. Evaluation of 2.0-mm titanium three-dimensional curved angle strut plate in the fixation of mandibular angle fractures—A prospective clinical and radiological analysis. Craniomaxillofac. Trauma Reconstr. 7(2), 119–125. https://doi.org/10.1055/s-0034-1371002 (2014).
Song, S. W., Burm, J. S., Yang, W. Y. & Kang, S. Y. Microplate fixation without maxillomandibular fixation in double mandibular fractures. Arch. Craniofac. Surg. 15(2), 53. https://doi.org/10.7181/acfs.2014.15.2.53 (2014).
Spinzia, A. et al. Open reduction and internal fixation of extracapsular mandibular condyle fractures: A long-term clinical and radiological follow-up of 25 patients. BMC Surg. 14(1), 68. https://doi.org/10.1186/1471-2482-14-68 (2014).
Pilanci, Ö., Basaran, K., Ceran, F. & Kuvat, S. V. Functional outcomes of preauricular underparotid retrograde approach for mandibular condyle fractures. J. Craniofac. Surg. 25(3), 1078–1081. https://doi.org/10.1097/SCS.0000000000000514 (2014).
Rahpeyma, A., Khajehahmadi, S. & Mehni, S. B. Treatment of mandibular fractures by two perpendicular mini-plates. Iran. J. Otorhinolaryngol. 26(74), 31 (2014).
Bhatt, K., Arya, S., Bhutia, O., Pandey, S. & Roychoudhury, A. Retrospective study of mandibular angle fractures treated with three different fixation systems. Natl. J. Maxillofac. Surg. 6(1), 31. https://doi.org/10.4103/0975-5950.168229 (2015).
Pandey, V., Bhutia, O., Nagori, S. A., Seith, A. & Roychoudhury, A. Management of mandibular angle fractures using a 1.7 mm 3-dimensional strut plate. J. Oral Biol. Craniofac. Res. 6(1), 36–41. https://doi.org/10.1016/j.jobcr.2015.11.001 (2016).
Tracy, K. & Gutta, R. Are embrasure wires better than arch bars for intermaxillary fixation?. J. Oral Maxillofac. Surg. 73(1), 117–122. https://doi.org/10.1016/j.joms.2014.08.020 (2015).
Aslan, C. Mandibula subkondil ve yüksek ramus kırıklarına retromandibular transparotid yaklaşım: İki nokta fiksasyonu. Turk. J. Trauma Emerg. Surg. https://doi.org/10.5505/tjtes.2015.21774 (2015).
Balaji, S. M. Modified endaural approach for the treatment of condylar fractures: A review of 75 cases. Indian J. Dent. Res. 27(3), 305. https://doi.org/10.4103/0970-9290.186235 (2016).
Domingo, F. et al. A single-center retrospective review of postoperative infectious complications in the surgical management of mandibular fractures: Postoperative antibiotics add no benefit. J. Trauma Acute Care Surg. 81(6), 1109–1114. https://doi.org/10.1097/TA.0000000000001232 (2016).
Odom, E. B. & Snyder-Warwick, A. K. Mandible fracture complications and infection: The influence of demographics and modifiable factors. Plast. Reconstr. Surg. 138(2), 282e–289e. https://doi.org/10.1097/PRS.0000000000002385 (2016).
Spinelli, G., Lazzeri, D., Arcuri, F., Valente, D. & Agostini, T. Management of mandibular angle fractures by two conventional 2.0-mm miniplates: A retrospective study of 389 patients. Craniomaxillofac. Trauma Reconstr. 9(3), 206–210. https://doi.org/10.1055/s-0036-1582457 (2016).
Yadav, S., Mittal, H., Dhupar, V., Akkara, F. & Sachdeva, A. Transoral approach alone in single miniplate osteosynthesis of angle fracture—Our experience. Natl. J. Maxillofac. Surg. 7(1), 71. https://doi.org/10.4103/0975-5950.196136 (2016).
Bouchard, C. & Mansouri, M. Open reduction with internal fixation of mandibular angle fractures: A retrospective study. J. Can. Dent. Assoc. 83(h3), 1488–2159 (2017).
Bruneau, S., Courvoisier, D. S. & Scolozzi, P. Facial nerve injury and other complications following retromandibular subparotid approach for the management of condylar fractures. J. Oral Maxillofac. Surg. 76(4), 812–818. https://doi.org/10.1016/j.joms.2017.11.003 (2018).
Monnazzi, M. S., Gabrielli, M. A. C., Gabrielli, M. F. R. & Trivellato, A. E. Mandibular angle fractures: A comparative study between one- and two-plate fixation. Dent. Traumatol. 33(2), 121–125. https://doi.org/10.1111/edt.12312 (2017).
Rastogi, S. et al. Treatment of mandibular angle fractures with single three-dimensional locking miniplates without maxillomandibular fixation: How much fixation is required?. Craniomaxillofac. Trauma Reconstr. 10(3), 188–196. https://doi.org/10.1055/s-0037-1600904 (2017).
Ribeiro-Junior, P. D., Vago, T. M., da Silva, W. S., Padovan, L. E. M. & Tiossi, R. ‘Mandibular angle fractures treated with a single miniplate without postoperative maxillomandibular fixation: A retrospective evaluation of 50 patients. CRANIO® 36(4), 234–242. https://doi.org/10.1080/08869634.2017.1330799 (2018).
Lim, H.-Y., Jung, T.-Y. & Park, S.-J. Evaluation of postoperative complications according to treatment of third molars in mandibular angle fracture. J. Korean Assoc. Oral Maxillofac. Surg. 43(1), 37. https://doi.org/10.5125/jkaoms.2017.43.1.37 (2017).
Ferreira e Costa, R. F., Oliveira, M. R., Gabrielli, M. A. C., Pereira-Filho, V. A. & Vieira, E. H. ‘Postoperative complications associated with different fixation methods of isolated mandibular angle fractures. J. Craniofac. Surg. 29(6), 1569–1573. https://doi.org/10.1097/SCS.0000000000004484 (2018).
Van Hevele, J. & Nout, E. Complications of the retromandibular transparotid approach for low condylar neck and subcondylar fractures: A retrospective study. J. Korean Assoc. Oral Maxillofac. Surg. 44(2), 73. https://doi.org/10.5125/jkaoms.2018.44.2.73 (2018).
Balasundram, S. et al. A 4-year multicentre audit of complications following ORIF treatment of mandibular fractures. J. Maxillofac. Oral Surg. 19(2), 289–297. https://doi.org/10.1007/s12663-019-01204-1 (2020).
Choi, T. J., Chung, Y. H., Cho, J. Y. & Burm, J. S. The use of microplates for internal fixation of comminuted mandibular fractures. Ann. Plast. Surg. 82(1), 55–61. https://doi.org/10.1097/SAP.0000000000001623 (2019).
Rao, E. et al. Principle of lag-screw fixation in mandibular trauma. J. Int. Soc. Prev. Community Dent. 9(3), 282. https://doi.org/10.4103/jispcd.JISPCD_64_19 (2019).
Sudheer, R., Chakravarthy, B. D., Vura, N. & Rajasekhar, G. Management of angle mandible fractures by 3D rectangular grid plate: A prospective study. J. Maxillofac. Oral Surg. 19(3), 420–424. https://doi.org/10.1007/s12663-019-01286-x (2020).
Bhardwaj, B., Singh, J. & Mahajan, S. Transbuccal approach in management of mandible angle fracture. Indian J. Otolaryngol. Head Neck Surg. 72(4), 457–462. https://doi.org/10.1007/s12070-020-01904-y (2020).
Bhargava, D., Sharma, Y. & Beena, S. Infinitesimal peri-angular pterygomasseteric transectioning approach (IPPTA) for the base fractures of the mandibular condyle: A preliminary study. J. Maxillofac. Oral Surg. 20(4), 657–664. https://doi.org/10.1007/s12663-020-01446-4 (2021).
Felix, K. & Singh, M. The retromandibular transparotid approach for reduction and internal fixation of mandibular condylar fractures. Ann. Maxillofac. Surg. 10(1), 168. https://doi.org/10.4103/ams.ams_193_19 (2020).
Ramaraj, P. N. et al. Variations in the retromandibular approach to the condyle-transparotid versus anteroparotid transmasseteric: A prospective clinical comparative study. J. Stomatol. Oral Maxillofac. Surg. 121(1), 14–18. https://doi.org/10.1016/j.jormas.2019.06.008 (2020).
Bhagat, M. J. A. et al. Application of anatomically designed 2-dimensional V plate in management of mandible fracture: A pilot study. J. Maxillofac. Oral Surg. 21(4), 1363–1368. https://doi.org/10.1007/s12663-021-01558-5 (2022).
Singla, S. et al. Management of mandibular angle fractures using single Y-shaped titanium miniplate at the superior border: A prospective clinical study. Indian J. Otolaryngol. Head Neck Surg. 74(S3), 4495–4499. https://doi.org/10.1007/s12070-020-02342-6 (2022).
Kumar, P. et al. Evaluation of mini-preauricular incision in the surgical management of condylar fracture. Cureus https://doi.org/10.7759/cureus.31725 (2022).
Laganà, F., Arcuri, F., Spinzia, A. & Bianchi, B. Analysis of the high submandibular approach: A critical reapprasail of a transfacial access to the mandibular skeleton. J. Craniofac. Surg. 34(1), e15–e19. https://doi.org/10.1097/scs.0000000000008892 (2022).
Martin, E. T. et al. Diabetes and risk of surgical site infection: A systematic review and meta-analysis. Infect. Control Hosp. Epidemiol. 37(1), 88–99. https://doi.org/10.1017/ice.2015.249 (2016).
Cheng, H. et al. Prolonged operative duration increases risk of surgical site infections: A systematic review. Surg. Infect. 18(6), 722–735. https://doi.org/10.1089/sur.2017.089 (2017).
Peng, X.-Q. et al. Risk factors for surgical site infection after spinal surgery: A systematic review and meta-analysis based on twenty-seven studies. World Neurosurg. 123, e318–e329. https://doi.org/10.1016/j.wneu.2018.11.158 (2019).
Mantoani, C. C. et al. Perioperative blood transfusion and occurrence of surgical site infection: An integrative review. AORN J. 110(6), 626–634. https://doi.org/10.1002/aorn.12861 (2019).
de Brito Poveda, V., Oliveira, R. A. & Galvão, C. M. Perioperative body temperature maintenance and occurrence of surgical site infection: A systematic review with meta-analysis. Am. J. Infect. Control 48(10), 1248–1254. https://doi.org/10.1016/j.ajic.2020.01.002 (2020).
Owens, C. D. & Stoessel, K. Surgical site infections: Epidemiology, microbiology and prevention. J. Hosp. Infect. 70(Suppl 2), 3–10. https://doi.org/10.1016/S0195-6701(08)60017-1 (2008).
Mengistu, D. A. et al. Global incidence of surgical site infection among patients: Systematic review and meta-analysis. Inq. J. Health Care Organ. Provis. Financ. 60, 004695802311625. https://doi.org/10.1177/00469580231162549 (2023).
Centers for Disease Control and Prevention. Type 2 diabetes. [Online] Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/diabetes/basics/type2.html (2021).
www.who.int. Global guidelines for the prevention of surgical site infection, 2nd ed. [Online] Available at: https://www.who.int/publications/i/item/global-guidelines-for-the-prevention-of-surgical-site-infection-2nd-ed (2018).
Deo, P. N. & Deshmukh, R. Oral microbiome: Unveiling the fundamentals. J. Oral Maxillofac. Pathol. JOMFP 23(1), 122–128 (2019).
Jazayeri, H. E. et al. Comparative benefits of open versus closed reduction of condylar fractures: A systematic review and meta-analysis. Plast. Reconstr. Surg. 151(4), 664e672e. https://doi.org/10.1097/prs.0000000000010009 (2022).
Zhan, S., Jiang, Y., Cheng, Z. & Ye, J. A meta-analysis comparing the 2.0-mm locking plate system with the 2.0-mm nonlocking plate system in treatment of mandible fractures. J. Craniofac. Surg. 25(6), 2094–2097. https://doi.org/10.1097/scs.0000000000001018 (2014).
Khavanin, N. et al. Management of teeth in the line of mandibular angle fractures treated with open reduction and internal fixation: A systematic review and meta-analysis. Plast. Reconstr. Surg. 144(6), 1393–1402. https://doi.org/10.1097/prs.0000000000006255 (2019).
Papanikolopoulou, A. et al. Ventilator-associated pneumonia, multidrug-resistant bacteremia and infection control interventions in an intensive care unit: Analysis of six-year time-series data. Antibiotics 11(8), 1128. https://doi.org/10.3390/antibiotics11081128 (2022).
Milic, T., Raidoo, P. & Gebauer, D. Antibiotic prophylaxis in oral and maxillofacial surgery: A systematic review. Br. J. Oral Maxillofac. Surg. 59(6), 633–642. https://doi.org/10.1016/j.bjoms.2020.09.020 (2021).
de Jonge, S. W. et al. ‘Timing of preoperative antibiotic prophylaxis in 54,552 patients and the risk of surgical site infection: A systematic review and meta-analysis. Medicine https://doi.org/10.1097/MD.0000000000006903 (2017).
Funding
This study received partial funding from the Special Account for Research Grants of the National and Kapodistrian University of Athens, on behalf of Maria Kantzanou. The remaining portion of the funding was provided by Maria Kantzanou.
Author information
Authors and Affiliations
Contributions
E.K.: study conception and design, literature search, data analysis, quality assessment, statistical meta-analysis, interpretation of results and manuscript writing. G.K.: literature search, data analysis, interpretation of results, manuscript editing, quality assessment and professional opinion. M.K.: literature search, data analysis, interpretation of results, manuscript writing and professional opinion. Ma.K.: critical revision of the manuscript, professional opinion and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kostares, E., Kostare, G., Kostares, M. et al. Prevalence of surgical site infections after open reduction and internal fixation for mandibular fractures: a systematic review and meta-analysis. Sci Rep 13, 11174 (2023). https://doi.org/10.1038/s41598-023-37652-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-37652-6
This article is cited by
-
Prevalence of lingual sensory impairment following bilateral sagittal split osteotomy: a systematic review and meta-analysis
Oral and Maxillofacial Surgery (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.