Abstract
Study design:
In the last years, there has been a change in the aetiology of spinal cord injury. There has been an increase in the number of elderly patients with spinal cord injuries caused by diseases or medical procedures.
Objective:
The aim of this study is to investigate the frequency of the occurrence of iatrogenic spinal cord injury in our unit. The secondary aim is to study what variables can be associated with a higher risk of iatrogenesis.
Methods:
A retrospective, descriptive, observational study of patients with acute spinal cord injury admitted from June 2009 to May 2014 was conducted. The information collected included the patient age, aetiology, neurological level and grade of injury when admitted and when discharged, cardiovascular risk factors, a previous history of depression and any prior treatment with anticoagulant or antiplatelet drugs. We applied a logistic regression. The grade of statistical significance was established as P<0.05.
Results:
In total, 265 patients were included. In 48 of the cases, the cause was iatrogenic (18.18%±4.6% IC). The most frequent level of injury was the thoracic level (48%). The main aetiology of spinal cord injury caused by iatrogenesis was surgery for degenerative spine disease, in patients under the age of 30 were treated with intrathecal chemotherapy.
Conclusions:
Iatrogenic spinal cord injury is a frequent complication. A statistically significant association between a patient history of depression and iatrogenic spinal cord injury was found as well as with anticoagulant and antiplatelet drug use prior to iatrogenic spinal cord injury.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a serious disease with a high socio-economic cost associated with the significant disability it causes and its associated high lifelong health expenses. It is a devastating disease with a frequency of occurrence of 12.1–57.8 cases per million.1
Our Spinal Cord Injuries Unit (SCIU) works as a reference centre for the treatment of acute SCI in the Comunitat Valenciana (5 004 844 inhabitants according to the National Institute of Statistics in 2014). This unit receives an average of 55 hospital admissions per year; patients with minor SCI are attended to on an outpatient basis.
In 2010, a study was carried out in our centre.2 We objectified a frequency of occurrence of iatrogenesis of 10.4%. In the current study, we wanted to know the current frequency of occurrence in our area and to analyse the possible associated risk factors.
In the last decade, the number of elderly patients with spinal cord injuries due to falls or medical conditions has increased. In our centre, the traumatic and the nontraumatic aetiology have been at 50% in the last 2 years. The points driving license scheme entered into force in the Spanish State on 1 July 2006 has proved effective in reducing accidents and increase road safety.3
It should be noted that there is a difference between iatrogenesis and medical malpractice. Iatrogenesis (iatros-doctor; genus-origin) concerns any negative change in a patient as a consequence of any medical act. In this study, we understand all medical interventions to be iatrogenic acts, whether therapeutic or diagnostic, that cause the deterioration of an existing SCI or the appearance of an SCI. Malpractice implies inattention or a mistake as a result of a miscalculation of the consequences of a medical action.
The main objectives of the study are as follows:
-
To calculate the frequency of the occurrence of iatrogenic spinal cord injuries in our area.
-
To identify the act that caused the iatrogenesis (surgical procedure, diagnostic or therapeutic technique or side effects).
The secondary objective is to determine which of the diverse variables that have been studied are statistically associated with the risk of suffering from iatrogenesis.
Materials and methods
This study is a retrospective, descriptive, observational study, in which the case histories of the patients who were admitted in our unit from 2009 to 2014 were examined to find those patients with iatrogenic spinal cord injuries.
Iatrogenesis cases were classified into the following three categories according to the causal act:
-
Surgical procedures: laminectomy,4 discectomy,5 arthrodesis,6 surgical correction of scoliosis,7 surgery due to aortic aneurysm.8
-
Techniques: anaesthetic9 and epidural analgesia, arterial chemoembolization, arteriograms, vertebroplasty.10
-
Pharmacological causes: spontaneous epidural haematoma in patients undergoing anticoagulation therapy11 or antiplatelet drug12 therapy (ASA/OAC) or toxic effects due to therapy with intrathecal chemotherapy.13, 14
Subjects
The inclusion criteria were as follows:
-
To have a spinal cord injury as a consequence of any medical action, whether therapeutic as diagnostic.
-
To demonstrate neurological deterioration according to the classification criteria of the American Spinal Injury Association (AIS)15 after the surgery in relation to the previous state of the patient.
The exclusion criteria were as follows:
-Surgery due to tumour occurrence, considering that it is inevitable in these cases because it is necessary to carry out resection with healthy margins, with the exception of the cases of postoperative complications such as infections16 or technical failure.
Variables
For each of the patients, we checked their age, gender, department of origin, aetiological diagnosis, type of precipitating procedure of iatrogenesis, whether they had a history of dyslipidaemia (DLD), arterial hypertension (AH), diabetes mellitus (DM), a substance history, a history of depression or obesity17, 18 as well as whether they were previously administered therapy with ASA/OAC before the event and the level and grade of the injury when they were admitted and discharged. In the event that it was an iatrogenic case, we checked what type of iatrogenesis it was (surgical, technical or pharmacological).
Statistical methods
To calculate the frequency of occurrence of iatrogenesis, we divided the number of patients admitted due to iatrogenesis by the total of admissions. We calculated a 95% confidence interval.
To determine the type of relation existing between the variables studied and the risk of suffering from iatrogenesis, a logistic regression was applied.
The results were obtained through the statistical software R (version 3.1.2, Statistical Department from La Fe Hospital, Valencia, Spain).
Results
General information
A total of 264 cases were included in the study, while only 48 of them (18.18%±4.6%) met the iatrogenic SCI criteria. In total, 22 out of these 48 (45.8%) were males, whereas 26 (54.2%) were females. We calculated a mean age of 56.04 years with a s.d. of 21.81. The age range was between a minimum of 3 and a maximum of 82 years. An increase in the frequency of occurrence of iatrogenesis from the 7th decade of life is visible (Figure 1).
By specialty
In regard to the percentage of iatrogenic patients caused by specialties, the majority are concentrated in Orthopaedic Surgery and Traumatology (27.1%), and Neurosurgery (27.1%), followed by anaesthesia (12.5%), Cardiovascular Surgery (10.4%) and Haematology (10.4%). The remaining percentage comprised the rest of the specialties (12.5%).
By aetiology and cause
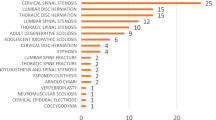
In total, 52.1% of the iatrogenesis cases were caused by surgical procedures, while 27.1% were caused by techniques and 20.8% were due to pharmacological causes. Figure 2 shows the frequency and the percentage of the cases according to the type of iatrogenesis shown.
Diseases
The disease that causes the most amount of iatrogenic intervention is degenerative spine disease procedures19 (31%), which is followed by intrathecal chemotherapy (12.5%), epidural anaesthesia (10.4%) and aortic aneurysm surgery (10.4%). We show the principal causes in Table 1.
Level and grade
The most frequent level of spinal cord injury was the thoracic level (nearly 50%). The most frequent grade of injury according to the AIS scale when the patients were admitted was grade C (43%), while the most frequent grade upon discharge was grade D (31%). Tables 2 and 3 show the grades and levels of injury of the patients who had been admitted due to iatrogenesis at admission and discharge.
By risk factor
The results obtained are shown below (Table 4). The variables ASA/OAC and history of depression show a statistically significant effect; the variables ASA/OAC and depression, with Odds Ratios of 5.73 and 3.24, respectively, could be considered risk factors in regards to iatrogenesis.
However, despite not being able to determine a statistically significant effect from the rest of variables, a trend is apparent; the variables dyslipidaemia and hypertension increase the risk of suffering from iatrogenesis. Finally, as shown in Table 3, a tendency for the variables age and obesity is also apparent; these variables are associated with Odds Ratios very close to 1 (0.99 and 1.12, respectively).
Discussion
In the study carried out 5 years ago by Alcanyis et al. in our same area, a 10% frequency of occurrence of iatrogenesis was observed. In our study, the frequency of occurrence of iatrogenesis was 18.18%. In our study, the most frequent iatrogenesis originating cause was surgery for canal stenosis. In our study, the most frequent grade of injury derived from iatrogenesis was grade D, while the most frequent degree of injury in Alcanyis study upon discharge was grade C. In both studies, the thoracic level predominated over the cervical or lumbar levels. Alcanyis et al. excluded the cases of neoplastic aetiology. In this study, we decided to include the cases caused by intrathecal CHT because of the amount of cases in which there had been a technical failure, toxic effect or postsurgical infection (12.5%).
The prospective study of patients with spinal cord injuries carried out by O’Connor20 showed that 2% of the new cases of patients with spinal cord injuries were caused by surgical procedures. Augustis et al.21 a study from Sweden, calculated the frequency of occurrence of spinal cord injury in children. They detected a frequency of occurrence of 3.3% of spinal cord injuries after disc surgery due to deformation. In our study, 3 cases of patients under 16 with spinal cord injuries caused by intrathecal CHT are especially significant. The study of Bacher et al,22 carried out 15 years ago, demonstrated that iatrogenesis was associated with surgical procedures in discs (0.69%) with a mean patient age of 34.4 years.
There is no unanimity about the classification of iatrogenic spinal cord injury. In the revision carried out by New et al. they defended that there are two different work groups. One includes iatrogenesis as traumatic aetiology;23 the other includes it as nontraumatic. As a consequence, the series collected could present very heterogenetic samples and quite different results.
By age
Advanced age is independently associated with an increase of the volume of postoperative spontaneous epidural haematoma.24 Sebastiá et al.25 reported an increase in the age of the typical spinal cord injury patient in a 13-year retrospective study. They also detected a mean age of 45.9. In other studies1 of traumatic spinal cord injury, two age peaks were detected regarding the frequency of occurrence. In this study, we can see an increasing tendency with regard to age, with a maximum peak in the 7th decade of life. Our results coincide with the study by Alcanyis et al. with a mean age of 56, not finding a statistically significant relation between age and the risk of suffering from iatrogenesis.
By cardiovascular risk factor
There are multiple articles that could explain the alterations observed on the micro- and macrovascular scales of AH, DLD, DM and substance history. In their study, Chen et al.26 deduced that both the age and a prior arterial hypertension history are risk factors for iatrogenesis and that a prior history of diabetes mellitus is related to the increase of the risk of suffering from iatrogenesis. They obtained significant results for gender and AH.
Some studies27 have reported an increase in the frequency of occurrence of surgical wound infections of lumbar surgery due to tumours compared with non-tumour origin infections. Diabetes mellitus28 and the abuse of intravenous drugs are factors that increase the risk of postoperative infection.
Although statistical significance for AH, DM and DLD has not been demonstrated in our work, tendencies for these factors have been demonstrated.
The results of our study showed the statistically significant relation between depression history and iatrogenesis, a factor that has not been considered in other similar studies. Our results could also be related to age. It has been proven that the presence of chronic pain is directly related to depression.29 Depression has been catalogued by other authors as a risk factor for adverse medical results in patients with acute coronary syndrome.30 Pain due to degenerative spine disease is very difficult to treat and is increasingly observed associated with depressive states. It is unclear whether depression is responsible for a decrease in pain threshold or is a consequence of chronic pain. They are complex patients, often demanding a solution to their problem, forcing the doctor to adopt aggressive treatments.
Many studies31 and meta-analyses have proven that depression is a strong predictor of adverse results in heart diseases. According to Barth et al.32 depression symptoms and clinical depression have an unfavourable impact on the mortality of patients with coronary diseases, and depression must be considered a relevant risk factor in patients with any coronary disease.
More research is needed to identify and develop efficient interventions for patients with chronic pain before the depression begins to become an accompanying symptom; also, further investigations are necessary to solve the problem about whether depression is a causal risk factor for morbidity and cardiovascular mortality in these patients.
We did not observe differences between sexes, even though the study by Chen et al.26 demonstrated that surgery was safer in women than in men because of hormones such as oestrogen and progesterone, which have neuroprotective effects due to Bcl-2 secretion.
Another unique discovery from our study is the relation between the intake of anticoagulant or antiplatelet drugs and SCI. The treated patients have a 5-fold higher risk of suffering from SCI than those who do not take these drugs. It is known that the first cause of spinal epidural haematoma is idiopathic, followed by anticoagulant therapy.9 However, there are several articles that address this relation. Iatrogenic spinal epidural haematomas are frequently associated with alterations in coagulation.33 The patients treated with anticoagulant and antiplatelet drugs are usually elderly people.34 We hypothesise these patients may suffer a higher frequency of falls because they suffer from retarded coagulation, which could produce a larger haematoma in these patients (as in intracerebral haemorrhages35) than in patients who have not been treated, increasing the frequency of occurrence of SCI.
Limits of the study
It is not possible to know the frequency of occurrence of each of the procedures carried out because most of them took place in other hospitals, and we do not have the information on all the surgeries performed in the other hospitals. We studied the risk factors individually.
It is probable that all the variables were not collected in the data collection process because it was not possible to find them. Throughout the study period, there was a change from paper-based case histories to computer-based case histories. The digitalized documents were revised, but some of the case histories were partially incomplete.
Regarding the risk factors involved, there are studies that examine each of them independently, but not the way they increase when some of them combine, which happens in most cases. This should be taken into account in future studies.
Conclusions
There are some conclusions that can be drawn from this study: the frequency of occurrence of iatrogenesis in this study is higher than that in others where non-surgical patients are not considered. Pharmacological iatrogenesis represents an important percentage that should be considered when prescribing anticoagulant and antiplatelet drugs because they are statistically associated with the risk of epidural haematoma. A statistically significant association between a personal history of depression and iatrogenic SCI has been found.
The results obtained in this study may be a casual discovery, but they should be considered in future studies. More research is needed to identify and develop efficient interventions in patients with risk factors who are going to undergo surgery.
Data Archiving
There were no data to deposit.
References
van den Berg MEL, Castellote JM, Mahillo-Fernandez I, de Pedro-Cuesta J . Incidence of spinal cord injury worldwide: a systematic review. Neuroepidemiology 2010; 34: 184–192.
Alcanyis-Alberola M, Giner-Pascual M, Salinas-Huertas S, Gutiérrez-Delgado M . Iatrogenic spinal cord injury: an observational study. Spinal Cord 2011; 49: 1188–1192.
World Health Organization. Effect on road traffic injuries of criminalizing road traffic offences: a time -series study. WHO: Geneva, Switzerland. http://www.who.int/bulletin/volumes/89/6/10-082180/en/. Accessed on 13 March 2017.
Cramer DE, Maher PC, Pettigrew DB, Kuntz C . Major neurologic deficit immediately after adult spinal surgery: incidence and etiology over 10 years at a single training institution. J Spinal Disord Tech 2009; 22: 565–570.
Ayhan S, Nelson C, Gok B, Petteys RJ, Wolinsky J-P, Witham TF et al. Transthoracic surgical treatment for centrally located thoracic disc herniations presenting with myelopathy: a 5-year institutional experience. J Spinal Disord Tech 2010; 23: 79–88.
Robaina-Padrón FJ . [Controversies about instrumented surgery and pain relief in degenerative lumbar spine pain. Results of scientific evidence]. Neurocirugia 2007; 18: 406–413.
Diab M, Smith AR, Kuklo TR . Spinal Deformity Study Group. Neural complications in the surgical treatment of adolescent idiopathic scoliosis. Spine 2007; 32: 2759–2763.
Etz CD, Luehr M, Kari FA, Bodian CA, Smego D, Plestis KA et al. Paraplegia after extensive thoracic and thoracoabdominal aortic aneurysm repair: does critical spinal cord ischemia occur postoperatively? J Thorac Cardiovasc Surg 2008; 135: 324–330.
Jusué-Torres I, Ortega-Zufiria JM, Tamarit-Degenhardt M, Navarro Torres R, López-Serrano R, Riqué-Dormido J et al. [Iatrogenic cervical epidural hematoma: case report and review of the literature]. Neurocirugia 2011; 22: 332–336.
Sietsma MS, Heerspink FOL, Ploeg WT, Jutte PC, Veldhuizen AG . [Kyphoplasty as treatment for osteoporotic vertebral compression fractures: relatively safe, but still no evidence of functional improvement; a review of the literature]. Ned Tijdschr Geneeskd 2008; 152: 944–950.
Kirazli Y, Akkoc Y, Kanyilmaz S . Spinal epidural hematoma associated with oral anticoagulation therapy. Am J Phys Med Rehabil 2004; 83: 220–223.
Karabatsou K, Sinha A, Das K, Rainov N . Nontraumatic spinal epidural hematoma associated with clopidogrel. Zentralbl Neurochir 2006; 67: 210–212.
Joseph PJ, Reyes MR . Dorsal column myelopathy following intrathecal chemotherapy for acute lymphoblastic leukemia. J Spinal Cord Med 2014; 37: 107–113.
Kwong Y-L, Yeung DYM, Chan JCW . Intrathecal chemotherapy for hematologic malignancies: drugs and toxicities. Ann Hematol 2009; 88: 193–201.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med 2011; 34: 535–546 [Internet].
Abdul-Jabbar A, Takemoto S, Weber MH, Hu SS, Mummaneni PV, Deviren V et al. Surgical site infection in spinal surgery: description of surgical and patient-based risk factors for postoperative infection using administrative claims data. Spine 2012; 37: 1340–1345.
Danish SF, Wilden JA, Schuster J . Iatrogenic paraplegia in 2 morbidly obese patients with ankylosing spondylitis undergoing total hip arthroplasty. J Neurosurg Spine 2008; 8: 80–83.
Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine 2007; 6: 291–297.
Djurasovic M, Glassman SD, Carreon LY, Dimar JR . Contemporary management of symptomatic lumbar spinal stenosis. Orthop Clin North Am 2010; 41: 183–191.
O’Connor RJ, Murray PC . Review of spinal cord injuries in Ireland. Spinal Cord 2006; 44: 445–448.
Augutis M, Levi R . Pediatric spinal cord injury in Sweden: incidence, etiology and outcome. Spinal Cord 2003; 41: 328–336.
Bacher T, Schiltenwolf M, Niethard FU, Paeslack V . The risk of paraplegia through medical treatment. Spinal Cord 1999; 37: 172–182.
New PW, Rawicki HB, Bailey MJ . Nontraumatic spinal cord injury: demographic characteristics and complications. Arch Phys Med Rehabil 2002; 83: 996–1001.
Sokolowski MJ, Garvey TA, Perl J, Sokolowski MS, Cho W, Mehbod AA et al. Prospective study of postoperative lumbar epidural hematoma: incidence and risk factors. Spine 2008; 33: 108–113.
Sebastià-Alcácer V, Alcanyis-Alberola M, Giner-Pascual M, Gomez-Pajares F . Are the characteristics of the patient with a spinal cord injury changing? Spinal Cord 2014; 52: 29–33.
Chen Q, Li F, Wu W . Risk factors of iatrogenic spinal cord injury in spinal surgery: a multicenter retrospective study. Int J Neurosci 2012; 122: 606–610.
Omeis IA, Dhir M, Sciubba DM, Gottfried ON, McGirt MJ, Attenello FJ et al. Postoperative surgical site infections in patients undergoing spinal tumor surgery: incidence and risk factors. Spine 2011; 36: 1410–1419.
McKinley W, Merrell C, Meade M, Brooke K, DiNicola A . Rehabilitation outcomes after infection-related spinal cord disease: a retrospective analysis. Am J Phys Med Rehabil 2008; 87: 275–280.
Carroll LJ, Cassidy JD, Côté P . Depression as a risk factor for onset of an episode of troublesome neck and low back pain. Pain 2004; 107: 134–139.
Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations. Circulation 2014; 129: 1350–1369.
Freedland KE, Carney RM . Depression as a risk factor for adverse outcomes in coronary heart disease. BMC Med 2013; 11: 131.
Barth J, Schumacher M, Herrmann-Lingen C . Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med 2004; 66: 802–813.
Groen RJM . Non-operative treatment of spontaneous spinal epidural hematomas: a review of the literature and a comparison with operative cases. Acta Neurochir 2004; 146: 103–110.
Groen RJ, van Alphen HA . Operative treatment of spontaneous spinal epidural hematomas: a study of the factors determining postoperative outcome. Neurosurgery 1996; 39: 494–508 discussion 508–9.
Lauer A, Pfeilschifter W, Schaffer CB, Lo EH, Foerch C . Intracerebral haemorrhage associated with antithrombotic treatment: translational insights from experimental studies. Lancet Neurol 2013; 12: 394–405.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Montalva-Iborra, A., Alcanyis-Alberola, M., Grao-Castellote, C. et al. Risk factors in iatrogenic spinal cord injury. Spinal Cord 55, 818–822 (2017). https://doi.org/10.1038/sc.2017.21
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2017.21
This article is cited by
-
Neurological injury as a complication of spinal surgery: incidence, risk factors, and prognosis
Spinal Cord (2020)
-
Prospective epidemiological update on traumatic spinal cord injury in Ireland
Spinal Cord Series and Cases (2019)