Abstract
Objectives:
To study the postural adaptations of subjects with incomplete spinal cord injury (iSCI) and non-injured subjects during overground walking on level and inclined surfaces.
Methods:
Six subjects with iSCI and seven non-injured subjects walked on an inclined surface (slope: 15%) and a level surface at their natural gait speed and at a slow gait speed (non-injured subjects only). Maximal stabilizing and minimal destabilizing forces were calculated to quantify dynamic balance during walking. Correlational analysis identified the variables that influence these stabilizing and destabilizing forces.
Results:
Subjects with iSCI and good sensorimotor recovery were similar to non-injured subjects with respect to maximal stabilizing and minimal destabilizing forces when they walked at the same speed. The MaxSF was mainly explained by the center of pressure speed and step length, whereas the minimal destabilizing force was moderately correlated with body mass and height.
Conclusion:
The influence of gait speed on balance should be considered with a group comparison. With regard to dynamic balance, highly functioning subjects with iSCI do not seem to be sufficiently challenged while walking at their preferred gait speed. Asking individuals with subtle impairments to walk faster following an iSCI may reveal postural adaptations and have an effect on balance abilities.
Similar content being viewed by others
Introduction
Recovering independent locomotion is a common goal of people following an incomplete spinal cord injury (iSCI).1 Within 1 year post injury, 80–100% of individuals with an American Spinal Injury Association (ASIA) Impairment Scale (AIS) D incomplete SCI (i.e., about 20% of the total SCI population 1 year post injury2) recover community ambulation.3, 4 However, clinical factors such as muscle weakness and reduced balance capacities may lead to low gait speed and biomechanical inefficiency that limit their ability to walk in the community.5, 6 Many people with SCI also require the use of assistive devices to walk safely.7, 8, 9
Poor postural control may partially explain the high incidence of falls in this population.10 Falls occur in about 40% of chronic patients with SCI.11 Balance requires not only integrity of sensorimotor function of the trunk and lower limbs but also muscle coordination to control the center of mass (CoM) in relation to the base of support (BoS) to prevent a fall.12 Following an iSCI, damaged sensorimotor pathways may lead to postural dysfunctions.5 Individuals with iSCI often present abnormal motor control (i.e., muscle co-contractions) and subsequent changes in gait parameters (i.e., increase in double time support and decrease in step length) and gait speed during level walking (Lw)13, 14 which are associated with decreased stability and greater risk of falls.15
Walking on an inclined surface requires additional postural and motor adaptations that can become challenging, if not impossible, for individuals with iSCI,5, 14 with uneven surfaces being a major cause of falls.11 During uphill walking (Uw), non-injured subjects increase their hip extensor and plantarflexor muscle activity during the stance-phase and at push-off, respectively.16 They also increase step length17, 18 and decrease gait speed and cadence.18 During downhill walking (Dw), these subjects increase their knee extensor power and knee flexion to control accelerations of the CoM.16 They also increase cadence17 and decrease step length.19
Of the few studies that have analyzed gait among individuals with iSCI while negotiating an inclined surface, it has been reported that they adopt strategies that differ from those of non-injured subjects.14 Leroux et al.13 reported that the use of walking aids to compensate for poor postural control in this population may limit the individual’s ability to adapt to walking on inclined surfaces. Walking with assistive devices often produces a more flexed trunk and pelvic posture that will prevent use of normal strategies (e.g., vertical trunk position in Dw13). This may lead to uncontrolled acceleration during Dw. Additional studies are needed to better document balance during unlevel and level surfaces and provide rehabilitation professionals with useful information when choosing the best surface to challenge postural control. The aim of this project was thus to study the postural adaptation of subjects with iSCI and non-injured subjects during Lw, Uw and Dw. The specific objectives were (i) to compare the balance strategies used in Lw, Uw and Dw among subjects with iSCI at natural gait speed (NGS) with non-injured subjects at NGS and at slow gait speed (SGS) and (ii) to identify factors that have an influence on balance using stabilizing and destabilizing forces20, 21 in both groups. Non-injured subjects performed the tasks at SGS to mimic the speeds attained by the iSCI group. The forces provide a laboratory quantification of the difficulty in maintaining balance during the analyzed task, in terms of posture (destabilizing force) and dynamics (stabilizing force).20 We hypothesized that subjects with iSCI would have greater difficulty maintaining balance (lower destabilizing and higher stabilizing forces), particularly during Dw, compared with non-injured subjects. We anticipated that these findings would be associated with greater differences in gait speed and step length compared with the non-injured group. We also expected non-injured participants to experience less difficulty maintaining balance while walking at their NGS. We also hypothesized that differences between groups will be less apparent when participants with iSCI were compared with non-injured subjects at matched gait speed.
Materials and methods
Participants
The inclusion criteria were (i) the ability to walk on an inclined pathway without holding the rails, using walking aids or requiring human assistance and (ii) a sufficient level of tolerance for physical exertion (>120 min with rest). Participants with other injuries in addition to the iSCI (including lower limb and head trauma) were excluded. Ethical approval was obtained from the Research Ethics Committee of the Centre de recherche interdisciplinaire en réadaptation (CRIR 395-1108). Each participant gave written consent before entering the study. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Clinical evaluation
Physical therapists from the SCI program at the Institut de réadaptation Gingras-Lindsay-de-Montréal performed the following clinical evaluations to describe the iSCI group under study. Motor scores of participants with SCI were obtained with the Lower Extremity Motor Score (LEMS) from the AIS scale. The neurological sensory score required the testing of four sensory modalities per dermatome (right/left light touch and right/left pin prick) with a maximal (normal) score of 112 on each side. Balance was clinically evaluated with the Berg Balance Scale3 and spasticity of the triceps surae was assessed using the Modified Ashworth Scale.22 Gait speeds were calculated during the laboratory assessment from the biomechanical data.
Equipment
The inclined pathway (Figure 1) was 3.65-m long by 1.20-m wide with an inclination of 8.5° (15%). Such a slope is sufficiently challenging for non-injured participants to alter ground reaction forces compared with level walking.17 There was a 1-m-long platform attached at the end of the pathway and handrails for security. Two AMTI force plates were embedded in the middle of the pathway and three in the ground to record forces and moments in three dimensions (OR6-6-1000, Advanced Mechanical Technology Inc., Watertown, MA, USA). There was no contact between the force plates and walkway in order to eliminate errors due to vibration. Ground reaction forces were recorded at a frequency of 600 Hz. Four synchronized motion analysis cameras (Optotrak model 3020; NDI Technology Inc., Waterloo, ON, Canada) captured the coordinates in three dimensions from 36 skin-fixed infrared light-emitting diodes placed on the legs, arms and trunk, at a sampling rate of 60 Hz. A six-marker probe was used to define 26 bony landmarks and to trace foot contours in order to locate joint articulations and the limits of the subjects’ BoS, respectively.
Procedure
The participants attended one 3-hour session at the Pathokinesiology laboratory. They walked uphill and downhill on the inclined pathway at NGS. As we did not have access to a safety harness on the inclined pathway and had asked participants to walk without touching the two handrails, trials at fast speed were not performed in this study. Non-injured subjects also walked at SGS (80% of NGS). These tasks were repeated for Lw. Each participant completed at least five trials for each condition, excluding the familiarization trials. Trials were recorded when the most-impaired (subjects with iSCI) or the non-dominant (non-injured subjects) foot contacted the force plate. The most-impaired lower limb was determined by the LEMS and the dominant lower limb was defined as the leg used to take a step following a destabilizing force applied at the pelvis in a standing position. Anthropometric measurements were taken for biomechanical calculation.
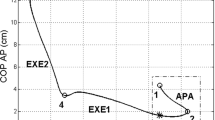
Data and statistical analyses
Gait cycles were time-normalized from 0 to 100% and averaged for each condition and each subject. Gait speed, cadence, step length and stance and swing-phase duration (gait cycle parameters) were analyzed. Maximal stabilizing force (MaxSF) and minimal destabilizing force (MinDF) were calculated using the equilibrium model of Duclos et al.20, 21 These data were collected when the most-impaired or non-dominant lower limb was in single support on the force plate, determined from kinematics based on the contralateral foot markers. The stabilizing force (SF) is the theoretical force required to cancel out the kinetic energy of the body over the distance between the current position of the center of pressure (CoP) and the limits of the BoS in the direction of the CoM velocity (Equation 1). The destabilizing force (DF) is the theoretical force needed to move the CoP to the limits of the BoS (Equation 2). A large SF and a small DF define a condition where balance is more difficult to maintain.20, 21 Hence, the MaxSF and the MinDF were analyzed as main outcome variables of maximal difficulty to maintain balance during the evaluated gait conditions.
Stabilizing force (in Newtons):

where mglobal is the body mass;  is the linear velocity of the body center of mass; and
is the linear velocity of the body center of mass; and  is the distance between the center of pressure and the limit of the potential base of support in the direction of
is the distance between the center of pressure and the limit of the potential base of support in the direction of  .
.
Destabilizing force (in Newtons):

where  is the ground reaction forces;
is the ground reaction forces;  is the normal unitary vector to ground surface;
is the normal unitary vector to ground surface;  is as defined in the previous equation.
is as defined in the previous equation.
The clinical characteristics, balance difficulty and spatiotemporal parameters were compared using paired-sample or independent-sample t-tests to determine significant differences between groups and conditions (alpha=0.05). Data were tested for normality (Shapiro-Wilk for each variable, P>0.05). The level of association between dependent variables (MaxSF and MinDF) and independent variables (height, body mass, center of pressure (CoP) speed, step length, step width, as well as stance and swing-phase duration) was analyzed with Pearson's correlation coefficients using all participants and trials. The CoP speed was measured at the moment corresponding to the MaxSF and MinDF. All statistical analyses were performed with SPSS Statistics 17.0.1 software (International Business Machines Corp., New York, NY, USA).
Results
Six male subjects with iSCI were recruited from the SCI program run by the Institut de réadaptation Gingras-Lindsay-de-Montréal and compared with seven age-matched non-injured subjects (2 females and 5 males; Table 1). Participants with SCI were classified as AIS D—that is, an incomplete motor lesion, with at least half the key muscles below the lesion capable of performing a full range-of-motion movement against gravity. Subject characteristics and gait cycle parameters are outlined in Table 1 and Table 2.
There were no significant differences in age (59 (standard deviation (SD) 7) years vs 56 (7) years, P=0.33), height (1.70 (0.09) vs 1.71 (0.09) m, P=0.69) or body mass (72.6 (11.1) vs 71.7 (10.6) kg, P=0.80) between the participants with iSCI and the non-injured participants, respectively (Table 2). The effects of the inclined pathway on gait cycle parameters and differences between groups are shown in Figure 2. Compared with NGS, non-injured subjects walking at SGS showed reduced gait speed (Lw: P<0.001; Uw: P=0.001 and Dw: P=0.006), cadence (Lw: P<0.001 and Uw: P<0.001) and step length (Lw: P<0.0018; Uw: P=0.004; Dw: P=0.007) with increased stance-phase (Lw: P=0.005; Uw: P=0.001; Dw: P=0.008) and swing-phase (Lw: P=0.086; Uw: P=0.007; Dw: P=0.012) durations (Figure 3). There were no significant differences for spatiotemporal parameters during Lw between non-injured subjects walking at NGS and subjects with iSCI (P>0.188) except for swing-phase duration (P=0.027). However, compared with non-injured subjects at NGS, subjects with iSCI presented a slower gait speed (Uw: P<0.001 and Dw: P=0.001), cadence (Uw: P=0.003) and step length (Uw: P=0.007; Dw: P=0.001), with increased stance-phase (Uw: P=0.011; Dw: P=0.030) but not swing-phase (Uw: P=0.87; Dw: P=0.83) duration while walking on the inclined pathway. There were no significant differences in most gait cycle parameters between subjects with iSCI and non-injured subjects at SGS for all conditions except that subjects with iSCI had a higher cadence during Lw (P=0.001) and a higher gait speed (1.13 (0.08) vs 0.89 (0.04) m/s, P=0.020), with longer stance (P=0.003) and swing (P=0.004) phases. The swing phase was also longer in the iSCI group than in the non-injured group at SGS during Uw (P=0.043) and Dw (P=0.032), the only parameters that differed on inclined pathways between these two groups.
Stabilizing and destabilizing forces
SF and DF for all conditions are shown in Figures 4 and 5, respectively. Non-injured subjects walking at SGS showed a lower MaxSF (Lw: P=0.006; Uw: P=0.004 and Dw: P=0.015) and a higher MinDF (Uw: P=0.031; Dw: P=0.004; Lw: P=0.047) compared with NGS for all conditions. There were no significant differences between non-injured subjects at NGS and subjects with iSCI during Lw (P>0.34). While walking on the inclined surface, subjects with iSCI showed a lower MaxSF (Uw: P=0.011; Dw: P=0.003) and a higher MinDF in Dw (P=0.020) and a trend in Uw (P=0.06), compared with non-injured subjects at NGS. There were no significant differences between groups when both walked at comparable speed for all conditions (P>0.07).
MaxSF (N) during level (Lw), uphill (Uw) and downhill (Dw) walking. The black line corresponds to subjects with SCI, the dark gray line to non-injured subjects at NGS and the light gray line to non-injured subjects at SGS. Diamonds correspond to the two slowest subjects with SCI, squares to the two fastest and triangles to the two average speed subjects.
MinDF (N) during level (Lw), uphill (Uw) and downhill (Dw) walking. The black line corresponds to subjects with SCI, the dark gray line to non-injured subjects at NGS and the light gray line to non-injured subjects at SGS. Diamonds correspond to the two slowest subjects with SCI, squares to the two fastest and triangles to the two average speed subjects.
Correlational analysis: factors associated with MaxSF and MinDF
Pearson's coefficients indicated correlations between MaxSF and gait characteristics for the entire group of participants under all conditions (Figure 6): The MaxSF was strongly correlated with the CoP speed (r=0.73, P<0.001), step length (r=0.63, P<0.001) and step width (r>0.66, P<0.001). These correlations were also found in each subgroup with correlation coefficients >0.50. MaxSF did not correlate with height and body mass (P=0.18 and P=0.18, respectively). MinDF correlations were significant but low with respect to body mass (r=0.46, P<0.001) and height (r=0.37, P=0.004) for the entire group of participants. These correlations were above 0.5 in each subgroup, except for body height in the healthy group at SGS (r<0.48, P>0.28).
Relationship between MaxSF (top) or MinDF (bottom) and velocity of the CoP speed (left), step length (center), step width (left) during level (squares, Lw), uphill (circles, Uw) and downhill (diamonds, Dw) walking in patients with SCI (black), non-injured participants at natural NGS (dark gray) and SGS (light gray).
Discussion
This study compared difficulty in maintaining balance among subjects with iSCI and non-injured subjects while walking on level and inclined surfaces. Subjects with iSCI recruited in this study walked slower than the non-SCI subjects on the inclined surface but not over level ground. It was therefore relevant to assess non-injured subjects walking both at NGS and SGS to take into account the influence of gait speed on balance and test how anthropometric and gait parameters are correlated with difficulty in maintaining balance. The study yielded findings that should be considered in gait rehabilitation for individuals with incomplete SCI (AIS D) and offers perspectives for further studies.
Effect of gait speed on balance
While walking at SGS, non-injured subjects showed a lower MaxSF and a higher MinDF compared with NGS. A smaller MaxSF and a higher MinDF indicate a situation in which balance is easier to maintain.20 Consequently, decreasing the speed of walking reduces the difficulty of maintaining balance. The relationship between gait speed and balance is still not completely understood in non-injured young and older adults. Whereas some authors proposed that self-selected gait speed is associated with greater stability of the head and trunk,23 others reported results that challenged this point of view during non-perturbed gait,24, 25 and clearly showed that the effect of speed is the opposite during trip and slip perturbations.15, 26 Our results indicate that reducing gait speed under conditions more demanding for balance, such as slopes, but in the absence of sudden perturbation, reduced the difficulty to maintain balance.
Reduction in step length was associated with higher stability,27 as was reduction in the risk of falls during perturbations,15 whereas stride frequency did not affect balance.27 Thus, gait adaptations associated with reduced gait speed likely contributed to the reduction of balance difficulty at SGS in the non-injured participants. Gait speed and the associated spatiotemporal parameters should therefore clearly be controlled when comparing groups with different self-selected speeds.
Balance difficulty in iSCI subjects compared with non-injured individuals
When comparing the group of iSCI subjects with the group of non-injured subjects performing at similar gait speed, no differences were observed between groups. Surprisingly, despite their sensorimotor deficits, subjects with iSCI (as a group) showed similar MaxSF and MinDF compared with non-injured subjects at SGS. We expected subjects with iSCI to have more difficulty, particularly during Dw.13 The mean group value did not reveal any difference, but high inter-subject variability, particularly for the MinDF during Dw, as shown in Figures 4 and 5, denoted variable balance difficulty in individuals with iSCI. Day et al.28 reported that instability was linked to increased variability in foot placement and that variability in gait was generally associated with fall risks in this population. Unfortunately, gait variability could not be evaluated with our experimental setup. One should note that our subjects with SCI presented high scores on the Berg Balance Scale (range 50–56) compared with the previous study by Day et al.28 (range 10–51). This may explain the absence of differences in comparison with non-injured subjects in light of the higher challenge offered by slope walking. Nevertheless, the reduced walking speed on the inclined surface in the iSCI group is certainly an important finding that supports difficulty in managing inclined surfaces.
We found that balance difficulty was the same between the groups when subjects walked overground at their respective self-selected speeds. However, when both groups were compared for Uw and Dw at a self-selected speed, individuals with iSCI showed lower cadence, step length, walking speed and longer stance-phase. The reduced step length and longer stance-phase, without unexpected perturbations, likely reduced balance difficulty in the iSCI group on the inclined surfaces. It is also likely that a lower gait speed in iSCI patients helped to keep the balance challenges at a manageable level, despite their remaining sensorimotor deficits. The gait characteristics selected by the participants with iSCI were thus likely reduced because of their muscle strength and sensory impairments, even if these impairments were mild, based on the clinical tests performed; these tests are known to present ceiling effects.3, 29 Our limited sample of high-functioning participants with iSCI did not allow us to explore the relationship between sensorimotor deficits and balance difficulties. In future studies, challenging balance with locomotion at a faster speed might thus reveal more deficits in high-functioning people with iSCI. Also, more challenging clinical tests such as the Community Balance and Mobility Scale, developed for such purposes in the brain injury field,30, 31 should probably be used to show any remaining balance deficits during gait after intensive rehabilitation following SCI.
Correlational analysis: factors associated with balance difficulty
The CoP speed and the step length and width influenced the MaxSF. Step length and width are clearly associated with CoM acceleration,32, 33 which might explain why it is associated with higher difficulty in maintaining dynamic balance.32 CoP speed has been shown to be lower in older adults compared with young non-injured adults, with the former walking at a lower preferred walking speed.34 CoP speed may be a marker of the participants’ ability to develop postural reactions to control CoM through CoP positioning.32 Because faster CoP speed was correlated with greater difficulty, it is possible that persons with less ability to rapidly move their CoP adapt their balance in order to make it easier to maintain. This is particularly evident in Figure 5, where most of the iSCI participants were at the lower left part of the scatterplots for the SF. This might also be related to reduced distal function due to the spinal cord lesion itself. Reduced distal function, which often results from the spinal cord lesion, was also the main difference observed during gait at matched speed on inclined surfaces between non-injured and iSCI participants.35
MinDF correlated to low body mass and height, which shows the moderate impact anthropometrics (rather than task-specific parameters) has on postural balance, at least for the tasks performed and the group of participants assessed in the present study.
Overall, these correlations revealed that step configuration and speed of movement are important for performing tasks at a higher speed or on a non-level surface and for maintaining balance.
In conclusion, no differences in MaxSF and MinDF were observed between subjects with iSCI and non-injured subjects walking at SGS. Limitations of this study are the group size and that the equilibrium model used in this study evaluates mainly the mechanical aspects of balance, based on body position and displacements. The influence of gait speed on balance was demonstrated and should be considered when both groups are compared at different gait speeds. In addition, greater balance difficulty at NGS compared with SGS in the non-injured subjects might reflect their ability to remain balanced despite the higher difficulty of the task. Therefore, links between the variables used to assess balance and sensorimotor capacities should be evaluated in further studies. Finally, according to the results of this study, it seems that subjects with iSCI are not sufficiently challenged while walking on a level surface at a self-selected gait speed. Rehabilitation specialists should consider training their patients to walk faster in order to increase their balance abilities and use varied surfaces to further challenge their dynamic balance.
References
Scivoletto G, Romanelli A, Mariotti A, Marinucci D, Tamburella F, Mammone A et al. Clinical factors that affect walking level and performance in chronic spinal cord lesion patients. Spine 2008; 33: 259–264.
Spiess MR, Muller RM, Rupp R, Schuld C, van Hedel HJ . Conversion in ASIA impairment scale during the first year after traumatic spinal cord injury. J Neurotrauma 2009; 26: 2027–2036.
Lemay JF, Nadeau S . Standing balance assessment in ASIA D paraplegic and tetraplegic participants: concurrent validity of the Berg Balance Scale. Spinal Cord 2010; 48: 245–250.
Scivoletto G, Di Donna V . Prediction of walking recovery after spinal cord injury. Brain Res Bull 2009; 78: 43–51.
Barbeau H, Nadeau S, Garneau C . Physical determinants, emerging concepts, and training approaches in gait of individuals with spinal cord injury. J Neurotrauma 2006; 23: 571–585.
Franceschini M, Rampello A, Agosti M, Massucci M, Bovolenta F, Sale P et al. Walking performance: correlation between energy cost of walking and walking participation. New statistical approach concerning outcome measurement. PLoS ONE 2013; 8: e56669.
Waters RL, Adkins RH, Yakura JS, Sie I . Motor and sensory recovery following incomplete paraplegia. Archives of Physical Medicine and Rehabilitation 1994; 75: 67–72.
Waters RL, Adkins RH, Yakura JS, Sie I . Motor and sensory recovery following incomplete tetraplegia. Arch Phys Med Rehab 1994; 75: 306–311.
Gil-Agudo A, Pérez-Rizo E, Del Ama-Espinosa A, Crespo-Ruiz B, Pérez-Nombela S, Sánchez-Ramos A et al. Comparative biomechanical gait analysis of patients with central cord syndrome walking with one crutch and two crutches. Clin Biomech 2009; 24: 551–557.
Brotherton SS, Krause JS, Nietert PJ . Falls in individuals with incomplete spinal cord injury. Spinal cord 2007; 45: 37–40.
Phonthee S, Saengsuwan J, Siritaratiwat W, Amatachaya S . Incidence and factors associated with falls in independent ambulatory individuals with spinal cord injury: a 6-month prospective study. Phys Ther 2013; 93: 1061–1072.
Horak FB . Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing 2006; 35: ii7–ii11.
Leroux A, Fung J, Barbeau H . Postural adaptation to walking on inclined surfaces: II strategies following spinal cord injury. Clin Neurophys 2006; 117: 1273–1282.
Leroux A, Fung J, Barbeau H . Adaptation of the walking pattern to uphill walking in normal and spinal-cord injured subjects. Exp Brain Res 1999; 126: 359–368.
Espy DD, Yang F, Bhatt T, Pai YC . Independent influence of gait speed and step length on stability and fall risk. Gait Posture 2010; 32: 378–382.
Lay AN, Hass CJ, Gregor RJ . The effects of sloped surfaces on locomotion: a kinematic and kinetic analysis. J Biomech 2006; 39: 1621–1628.
McIntosh AS, Beatty KT, Dwan LN, Vickers DR . Gait dynamics on an inclined walkway. J Biomech 2006; 39: 2491–2502.
Ferraro RA, Pinto-Zipp G, Simpkins S, Clark M . Effects of an inclined walking surface and balance abilities on spatiotemporal gait parameters of older adults. J Geriatr Phys Ther 2013; 36: 31–38.
Leroux A, Fung J, Barbeau H . Postural adaptation to walking on inclined surfaces: I. Normal strategies. Gait Posture 2002; 15: 64–74.
Duclos C, Desjardins P, Nadeau S, Delisle A, Gravel D, Brouwer B et al. Destabilizing and stabilizing forces to assess equilibrium during everyday activities. J Biomech 2009; 42: 379–382.
Duclos C, Mieville C, Gagnon D, Leclerc C . Dynamic stability requirements during gait and standing exergames on the wii fit(R) system in the elderly. J Neuroeng Rehabil 2012; 9: 28.
Haas BM, Bergstrom E, Jamous A, Bennie A . The inter rater reliability of the original and of the modified Ashworth scale for the assessment of spasticity in patients with spinal cord injury. Spinal Cord 1996; 34: 560–564.
Latt M, Menz H, Fung V, Lord S . Walking speed, cadence and step length are selected to optimize the stability of head and pelvis accelerations. Exp Brain Res 2008; 184: 201–209.
Kang HG, Dingwell JB . Effects of walking speed, strength and range of motion on gait stability in healthy older adults. J Biomech 2008; 41: 2899–2905.
Bruijn SM, van Dieën JH, Meijer OG, Beek PJ . Is slow walking more stable? J Biomech 2009; 42: 1506–1512.
Pavol MJ, Owings TM, Foley KT, Grabiner MD . Mechanisms leading to a fall from an induced trip in healthy older adults. J Gerontol 2001; 56: M428–M437.
Hak L, Houdijk H, Beek PJ, van Dieen JH . Steps to take to enhance gait stability: the effect of stride frequency, stride length, and walking speed on local dynamic stability and margins of stability. PLoS One 2013; 8: e82842.
Day KV, Kautz SA, Wu SS, Suter SP, Behrman AL . Foot placement variability as a walking balance mechanism post-spinal cord injury. Clin Biomech 2012; 27: 145–150.
Steeves JD, Lammertse D, Curt A, Fawcett JW, Tuszynski MH, Ditunno JF et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP panel: clinical trial outcome measures. Spinal Cord 2007; 45: 206–221.
Howe JA, Inness EL, Venturini A, Williams JI, Verrier MC . The Community Balance and Mobility Scale-a balance measure for individuals with traumatic brain injury. Clin Rehab 2006; 20: 885–895.
Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C . Exercise for improving balance in older people. Cochrane Database of Systematic Reviews 2011; 8: CD004963.
Winter DA . Human balance and posture control during standing and walking. Gait Posture 1995; 3: 193–214.
Kuo AD, Donelan JM . Dynamic principles of gait and their clinical implications. Phys Ther 2010; 90: 157–174.
Chiu M-C, Wu H-C, Chang L-Y, Wu M-H . Center of pressure progression characteristics under the plantar region for elderly adults. Gait Posture 2013; 37: 408–412.
Desrosiers E, Duclos C, Nadeau S . Gait adaptation during walking on an inclined pathway following spinal cord injury. Clin Biomech 2014; 29: 500–505.
Acknowledgements
This work was financed by the Sensorimotor Rehabilitation Research Team (SMRRT; Strategic initiative, Canadian Institutes of Health Research—CIHR). ED was supported by a summer scholarship from the COPSÉ program (Faculty of Medicine, Université de Montréal) and by the Fonds de Recherche du Québec-Santé (FRQ-S).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Desrosiers, É., Nadeau, S. & Duclos, C. Balance during walking on an inclined instrumented pathway following incomplete spinal cord injury. Spinal Cord 53, 387–394 (2015). https://doi.org/10.1038/sc.2014.215
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.215
This article is cited by
-
Evaluation of an ankle–foot orthosis effect on gait transitional stability during ramp ascent/descent
Medical & Biological Engineering & Computing (2022)
-
Introducing a psychological postural threat alters gait and balance parameters among young participants but not among most older participants
Experimental Brain Research (2017)