Abstract
Study design:
Case Report.
Objectives:
To report a case of spinal intradural abscess caused by hematogenous spread of Prevotella oralis and discuss the treatment.
Setting:
Department of Neurosurgery, Ankara Education and Research Hospital, Ankara, Turkey.
Method:
We report a 3-year-old child with progressive paraparesis who was diagnosed with an intradural spinal abscess, epidermoid cyst and dermal sinus. The patient was treated surgically followed by antimicrobial treatment.
Result:
Intraoperative abscess culture was positive for Prevotella oralis, which has not been reported before as a single isolate in literature. The patient’s neurologic status was significantly improved after surgical treatment.
Conclusion:
Prophylactic antimicrobial therapies should cover the anaerobic bacteria in spinal intradural abscess. Surgical decompression with laminectomy and duraplasty may be warranted to achieve immediate neurologic improvement in such cases.
Similar content being viewed by others
Introduction
Intradural spinal abscess is a rare entity and more commonly seen in adults.1 It is mainly caused by the hematogenous spread from a cardiopulmonary source.1 In children, intradural infection is more commonly caused by pre-existing congenital abnormalities in spinal column; however, hematogenous spread may occur from various sources.1
The most common cause of spinal infections are Staphylococcus aureus and beta hemolytic Streptococcus, whereas anaerobic Gram-negative bacilli (AGNB) are extremely rare.2 In this study, we reported the first case of spinal intradural abscess caused by the hematogenous spread of Prevotella oralis, an AGNB, which has not been described as a single isolate of the intradural abscess in literature.
Case report
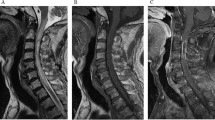
A 3-year-old girl was admitted with complaints of back pain, progressive weakness in the legs and difficulty in urination for 5 days. She had fever (38.6 °C) and laboratory investigations revealed a leukocytosis (14.200 per μl) and high number of leukocytes on urine examination. Her physical examination revealed no sign suggestive of dermal sinus tract, on the skin and no infection either of ear, mouth or teeth. The bilateral lower extremity muscle strength was graded as 3/5. Spinal magnetic resonance imaging (MRI) revealed a cystic lesion at the level of L4 and L5 with dermal sinus tract at L5–S1 disk space and hyperintense multiple cystic lesions on T2-weighed images from T11 to L3 vertebra levels (Figure 1). The patient underwent a L3–L5 en-block laminectomy with preservation of the facet joints. The intradural abscess was drained and the specimen was obtained by an aseptic needle. The cystic lesion and dermal sinus tract were excised. Extensive duraplasty using bovine pericardium was performed (Figure 2). Specimen was transported into both oxygen and oxygen-free gassed-out tubes for isolation of aerobic and anaerobic bacteria, respectively. Prevotella oralis was identified as a single isolate from the intraoperative cultures by the Minitek system. Histopathology evaluation was consisted with epidermoid cyst without any feature of infection within the specimen (Figure 3). Vancomycin (3 × 260 mg IV) and metronidazole (3 × 150 mg IV) therapies, which were administered preoperatively, were continued for 6 weeks. Paraparesis showed immediate improvement in the postoperative period. The patient was discharged after conducting normal neurological examination.
Discussion
Spinal intradural abscess is an extremely rare condition especially in pediatric cases.1 Although it is most likely associated with congenital spinal abnormalities; urogenital infections, infective endocarditis and infective pulmonary diseases can be a source of the spinal intradural abscess via hematogenous spread.1, 2 Dermal sinus is a frequently encountered congenital abnormality in such cases.1 The risk of infection is higher when the dermal sinuses are related with dermoid cyst rather then epidermoid cyst.1 However, in the presented case it was associated with epidermoid cyst. There was no sign of infection either at dermal sinus tract or epidermoid cyst during the operation and the postoperative histopathology examination revealed no feature of infection, but preoperative urine testing revealed abundant leukocytes. According to these findings, hematogenous spread from the urinary infection was presumed as a source of infection rather then the pre-existing congenital spinal abnormality.
Prevotella oralis; a Gram-negative anaerobic bacterium, as an isolated microbiologic agent in spinal infections is not a well-known entity. Prevotella oralis is a major commensal on mucosal surfaces such as oral cavity, gastrointestinal and urinary tracts.3 For this reason, only specimen that were properly collected without contamination by the mucosal flora and inoculated in the oxygen-free tubes would be appropriate for isolation of this bacterium. Brook reviewed the 2033 specimens from 418 patients and found that the Prevotella oralis was isolated in 58 specimens. There was no spinal infection caused by the Prevotella oralis in that study.3 Goyal et al.2 reported an adult patient who had vertebral osteomyelitis and spinal epidural abscess due to Prevotella oralis. Simon et al. reported a 13-month-child patient who was operated for spinal intradural cyst, dermal sinus and spinal intradural abscess. The intraoperative cultures grew a mixed growth of anaerobic bacteria in their case.1 In the presented case, the specimen was obtained by an aseptic needle and inoculated to the appropriate tubes for anaerobic bacteriological investigation. To our knowledge, the presented case is the first report of a spinal intradural abscess caused by Prevotella oralis as a single isolate, in literature.
The treatment of spinal intradural abscess is immediate surgical drainage followed by intravenous antibiotic therapy.1, 2 Simon et al. reported that the degree of the neurological improvement was most likely associated with timing of surgery rather than length of antimicrobial treatment.1 It has been showed that the laminoplasty when compared with the laminectomy decreases the postoperative spinal deformity for treatment of intradural lesions, especially at the thoracolumbar junction, in pediatric cases.4 In the presented case we preferred to perform laminectomy and extensive duraplasty to ensure the effective decompression of the spinal cord. In the presented case rapid neurologic improvement was achieved immediately after operation and postoperative MRI showed no spinal deformity. Although we preserved the facet joints during the operation and the surgical intervention was at lumbar levels, the follow-up period is too short (6 months) to conclude that the spinal deformity would not have occurred in this patient. However, since the edema may not resolve until the specific antimicrobial therapy reaches the effective dose at the area of the infection, surgical decompression with this technique may improve long-term functional outcome in such cases.
Because the most common causative organism of spinal intradural abscess is Staphylococcus aureus and there is a high incidence of methicillin-resistance, Huang et al.5 recommended the use of vancomycin as an initial empirical antibiotic in treatment of acute bacterial spinal abscess. In the presented case we used the combination of vancomycin and metronidazole to ensure a wide-spectrum antimicrobial treatment, because the patient had rapidly progressive neurologic deficits. Although the postoperative culture was only positive for an anaerobic bacteria (Prevotella oralis), we did not discontinue the treatment of vancomycin to prevent superinfection of surgery related aerobic bacteria.
Conclusion
This is the first report of a spinal intradural abscess caused by Prevotella oralis as a single isolate. This case indicates that the prophylactic antimicrobial therapies should cover the anaerobic bacteria in spinal intradural abscess. Intraoperative specimen should be obtained properly and inoculated into specific tubes for appropriate bacteriological investigation. Surgical decompression with laminectomy and duraplasty should be considered to improve long-term functional outcome in case of spinal intradural abscess, which causes progressive neurologic deficits.
References
Simon JK, Lazareff JA, Diament MJ, Kennedy WA . Intramedullary abscess of the spinal cord in children: a case report and review of the literature. Pediatr Infect Dis J 2003; 22: 186–192.
Goyal H, Arora S, Mishra S, Jamil S, Shah U . Vertebral osteomyelitis and epidural abscesses caused by Prevotella oralis: a case report. Braz J Infect Dis 2012; 16: 594–596.
Brook I . Prevotella and Porphyromonas infections in children. J Med Microbiol. 1995; 42: 340–347.
McGirt MJ, Chaichana KL, Atiba A, Bydon A, Witham TF, Yao KC et al. Incidence of spinal deformity after resection of intramedullary spinal cord tumors in children who underwent laminectomy compared with laminoplasty. J Neurosur Pediatr 2008; 1: 57–62.
Huang PY, Chen SF, Chang WN, Lu CH, Chuang YC, Tsai NW et al. Spinal epidural abscess in adults caused by Staphylococcus aureus: clinical characteristics and prognostic factors. Clin Neurol Neurosurg 2012; 114: 572–576.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Karatay, M., Koktekir, E., Celik, H. et al. Spinal intradural abscess caused by hematogenous spread of Prevotella oralis in a 3-year-old child with an asymptomatic congenital spinal abnormality. Spinal Cord 53 (Suppl 1), S13–S15 (2015). https://doi.org/10.1038/sc.2014.197
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.197
This article is cited by
-
Exploring the signature gut and oral microbiome in individuals of specific Ayurveda prakriti
Journal of Biosciences (2021)