Abstract
Study design:
An immunohistological assessment of substance P (SP), its NK1 receptor and claudin-5 in human spinal cord injury (SCI) tissue.
Objective:
To determine whether SP and NK1 receptor immunoreactivity are altered following human traumatic SCI.
Setting:
Australia.
Summary of background data:
SP has been implicated in the development of neurogenic inflammation and subsequent edema development following both traumatic brain injury and ischemic stroke. In these conditions, inhibition of its NK1 receptor has been shown to be neuroprotective as reflected in a reduction of edema and improved functional outcome. However, the role of SP following human SCI has not yet been assessed.
Methods:
Archived human SCI tissue was grouped according to survival times: control (no injury; n=5); immediate (death within an hour of the incident; n=6); 2–5 h (n=3); 3 days (n=5); 1 week (n=3); and 3–4 weeks (n=6). Sections were assessed for SP, its NK1 receptor and claudin-5 using immunohistochemical techniques.
Results:
Following SCI, dorsal horn SP immunoreactivity demonstrated a profound decrease compared with control tissue, indicating the loss of SP with SCI. A marked increase in perivascular NK1 staining was demonstrated after SCI compared with control levels. No obvious change in claudin-5 immunoreactivity was present immediately following injury, however, by 1 week post-SCI, decreased levels were noted.
Conclusion:
This study demonstrates that severe acute traumatic human SCI results in decreased SP and an immediate increase in NK1 receptor immunoreactivity, suggesting that there is a neurogenic inflammatory component following human SCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is an unexpected event that is both devastating and debilitating, commonly resulting in permanent physical disability. The highest incidence of SCI occurs in younger populations, resulting in an enormous financial burden to both individuals and society.1 Current treatments for SCI are largely ineffective with little functional benefit observed. As such, research into reducing injury and improving neurological function following SCI is of growing importance.
It has been well established that human SCI is characterized by severe hemorrhage and edema. Indeed, the presence of both hemorrhage and edema, as assessed by magnetic resonance imaging and computed tomography scanning, has been associated with poor functional outcome following human SCI.2 In addition, such studies demonstrated that functional outcome worsened when edema spread rapidly over multiple spinal cord segments,2 sometimes encompassing an additional vertebral segment each day.3 Such rostrocaudal spreading of edema results in further tissue damage and worsened functional outcome.4 Moreover, a study by Koyanagi et al.5 demonstrated that surgical decompression did not affect cord swelling. Thus, edema following SCI presents as a serious complication, with no effective treatment currently available.
Although the mechanisms associated with edema formation are unclear, substance P (SP) is a neuropeptide that has been recently implicated in edema formation through its ability to induce neurogenic inflammation.6, 7 SP illicits such a response through binding and activation of its primary receptor the NK1 receptor,8 resulting in increased vascular permeability and development of vasogenic edema. Recent experimental studies have demonstrated such a role for SP in both traumatic brain injury (TBI)9 and ischemic stroke,10 where increased SP expression was associated with increased blood–brain barrier (BBB) permeability and edema. Furthermore, inhibition of SP with an NK1 receptor antagonist reduced BBB permeability and edema development while improving functional outcome.9, 10 Although similar secondary injury processes occur following TBI, stroke and SCI, including the development of vasogenic edema,11 the role of SP as a mediator of neurogenic inflammation following SCI has not yet been established.
As such, the current study investigates the expression of SP, NK1 receptor and claudin-5 through immunohistochemical analysis following human SCI. Claudin-5 is an integral tight junction protein of the BBB and blood–spinal cord barrier (BSCB)12 whose altered expression may reflect a role for tight junction dysfunction in the development of vasogenic edema following SCI.
Materials and methods
Archived human spinal cord tissue was obtained from the SA brain bank (Adelaide, South Australia, Australia). In total, 23 patients with documented traumatic SCIs and 5 control cases with no trauma evident following post-mortem examination were included. All cases underwent comprehensive neuropathological analysis with macroscopic and microscopic assessment of all spinal cord segments following formalin fixation of the spinal cords. The SCI cases were grouped into survival times post-injury: immediate (death within an hour of the incident; n=6); 2–5 h (n=3); 3 days (n=5); 1 week (n=3) and 3–4 weeks (n=6).
Immunohistochemistry
Archived paraffin blocks of the lesion epicenter and adjacent spinal cord segments were used in this study. Five-micrometer-thick sections were cut for histological examination including assessment using hematoxylin and eosin staining to allow for observation of cellular changes within the lesioned area and the adjacent segments. Immunohistochemistry was used to identify the expression of SP (Santa Cruz Biotechnology, Dallas, TX, USA, Sc-9758; 1:2000; EDTA antigen retrieval), NK1 receptor (Thermo Scientific, Waltham, MA, USA, PA3-301; 1:16 000; citrate antigen retrieval) and claudin-5 (Invitrogen, Victoria, Australia, 32–2500; 1:2000; EDTA antigen retrieval). The SP (N-18) is an affinity-purified goat polyclonal antibody raised against a peptide corresponding to full-length mature of SP of human origin. The NK1 receptor antibody is an affinity-purified rabbit polyclonal antibody, which specifically corresponds to residues S(387) S R S D S K T M T E S F S F S S N V L S(407) of human NK1 receptor protein. The claudin-5 antibody is affinity purified from mouse ascites, which reacts specifically with the ∼22–24 kDa endogenous claudin-5 protein. Generated slides were scanned at high resolution using a Hamamatsu Nanozoomer (Hamamatsu, Hamamatsu, Japan), and viewed using the associated proprietary viewing software (NDP.view v1.1.27, Hamamatsu, Hamamatsu, Japan). Qualitative assessments were made using a ranking system ranging from 0 to 5, where 0=no immunoreactivity present, 1=very faint, 2=faint, 3=moderate, 4=dark and 5=very dark.
Statistical analysis
All data were assessed using a Kruskal–Wallis analysis of variance followed by Dunn’s multiple comparisons test.
Results
SCI case data
Case data are summarized in Table 1. There was a higher proportion of males in the study sample than females (males=21, females=3). The age of individuals was wide ranging (10–96 years) with a mean age of 47±25 years. The most common cause of injury was motor vehicle accidents (vehicle occupant or pedestrian), followed by falls. All causes were traumatic in nature except for one iatrogenic case that involved acute compression of the spinal cord during fusion surgery of the C1 and C2 vertebrae. The predominant type of primary injury was fracture dislocation and the most common level of injury was cervical.
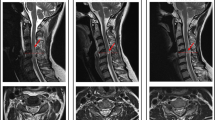
Morphological features of human SCI
Hematoxylin and eosin staining was used to assess general morphological features following human traumatic SCI (Figure 1). Immediately following injury, profound hemorrhage was observed diffusely throughout the swollen injury epicenter of the spinal cord, extending into the adjacent segments. There was extensive microvacuolation of the neuropil consistent with edema. At 3 days post-SCI, severe hemorrhagic necrosis and swelling were present within the injury epicenter and adjacent segments. Axonal swellings were apparent in the white matter regions within the injury epicenter and to a lesser extent within the adjacent segments. At 1 week post-SCI, the extent of hemorrhage and swelling diminished, however, an increase in tissue loss was observed with marked axonal swelling in the white matter. Within the adjacent segments, minimal hemorrhage was observed with localized areas of axonal swelling. By 3–4 weeks post-SCI, a substantial loss of tissue, because of reabsorption of necrotic tissue, was apparent with hemorrhage no longer present. Within the adjacent segments at this time, greater tissue loss within the white matter was observed when compared with the 1 week time point and cyst formation was present in some cases.
Hematoxylin and eosin stain—general morphological features. Immediately post-SCI severe hemorrhage was observed within the injury epicenter, which extended into the adjacent segments (black arrowheads indicate areas of hemorrhage). At 3 days post-SCI, severe hemorrhage was still evident within the injury epicenter and to a lesser extent within the adjacent segments. At 1 week post-SCI, moderate hemorrhage was still apparent with significant loss of tissue architecture. However, the adjacent segments demonstrated conserved tissue architecture with minimal hemorrhage and vacuolation of white matter. At 3–-4 weeks post-SCI, significant loss of tissue architecture was observed within the injury epicenter, with extensive white matter changes within the adjacent segments. Whole cross-sections: scale bar=2 mm; higher magnification: scale bar=200 μm.
SP response following human SCI
SP immunoreactivity following human traumatic SCI is summarized in Figure 2 and Table 2. In control cases, a high level of SP immunoreactivity was observed within lamina II and III of the dorsal horn region, which was expected given that SP stores are known to exist within this area. No difference in immunoreactivity was observed along the length of the spinal cord. Immediately following injury there was little change in SP immunoreactivity within the injury epicenter or along the adjacent segments when compared with control. Within 2–5 h of injury, the level of SP immunoreactivity began to decrease in the injury epicenter and also in the segments caudal and rostral to the injury. At 3 days post-injury, a decrease in SP immunoreactivity was still evident within the injury epicenter, however, the distal segments both rostral and caudal showed staining comparable to control levels. At 1 week post-injury, there was again a decrease in all segments of the spinal cord when compared with control immunoreactivity. Finally, at 3–4 weeks post-injury, a significant decrease in SP immunoreactivity was observed within the injury epicenter (P<0.01). Segments both caudal and rostral to the injury epicenter showed greater intensity of immunoreactivity than that of the injury epicenter most evident in the most distal segments.
Human SP immunoreactivity following SCI within the dorsal horn region. High immunoreactivity was observed within the dorsal horn of control human sections. No change in SP immunoreactivity was observed immediately following injury. However, by 3 days post-injury, a decrease was apparent within the dorsal horn region. The greatest decrease in SP immunoreactivity was observed at 3–4 weeks post-injury, most notably within the injury epicenter, although apparent along all segments of the spinal cord. Rostral and Caudal images are both 1 segment away from the injury epicenter. Arrows indicate region of immunoreactivity within the dorsal horn. Scale bar=250 μm.
NK1 receptor immunoreactivity following human SCI
NK1 receptor immunoreactivity following human SCI is summarized in Figure 3 and Table 3. The control human spinal cord sections showed a low basal level of staining prominent in the perivascular region. Immediately following SCI there was a profound increase in perivascular NK1 receptor immunoreactivity both within the injury epicenter and in the adjacent segments when compared with controls. At 2–5 h post-SCI, there was a slight decrease within the injury epicenter, and a further decrease observed at 3 days post-SCI for all levels of spinal cord. At 1 week post-SCI, a slight increase in NK1 receptor immunoreactivity within the injury epicenter was observed. In addition, a slight increase was observed in both rostral segments when compared with control levels. By 3–4 weeks post-SCI, all segments demonstrated immunoreactivity comparable to control, except the injury epicenter, which was slightly decreased. No significant differences were observed at any time point or at any level of the spinal cord tissue.
NK1 receptor immunoreactivity following human SCI—perivascular. All images are within the injury epicenter of the spinal cord. Faint NK1 receptor immunoreactivity was present within the perivascular region in control cases. A marked increase in immunoreactivity was observed immediately following SCI when compared with control. NK1 receptor immunoreactivity then decreased slightly at 3 days post-SCI, although remained above control levels. At 3–4 weeks post-SCI, NK1 receptor immunoreactivity was slightly decreased when compared with control. Arrows indicate perivascular immunoreactivity. Scale bar=50 μm.
Claudin-5 expression following human SCI
As an integral member of the BSCB protein family, claudin-5 immunoreactivity was assessed to determine if its expression is altered following traumatic SCI (Figure 4 and Table 4). The control sections demonstrated pronounced intense perivascular immunoreactivity. Immediately post-injury and at 3 days post-injury all segments of spinal cord remained comparable to control immunoreactivity. However, by 1 week post-injury a decrease in claudin-5 immunoreactivity was noted within the injury epicenter and adjacent segments. This decrease remained apparent at 3–4 weeks with a significant decrease observed within the injury epicenter (P<0.05).
Claudin-5 immunoreactivity following human SCI. Control spinal cord sections demonstrated intense claudin-5 immunoreactivity. Immediately, and at 3 days post-injury, no difference in claudin-5 immunoreactivity was observed when compared with control intensity. At 3–4 weeks post-SCI, a marked reduction in immunoreactivity was apparent. Arrows indicate perivascular immunoreactivity. Scale bar=50 μm.
Discussion
Given that human SCI occurs in an uncontrolled environment, the results of the present study must be interpreted in light of the varying severity, post-mortem times and demographics of obtained cases. In an attempt to reduce such variability, cases were grouped according to survival time points and it was assumed that most cases represent the severe end of the injury spectrum given that all tissue was post-mortem. The assessed human cases demonstrated significant primary tissue damage, which manifests as severe hemorrhage and necrosis with loss of tissue architecture. Such tissue damage was greatest within the injury epicenter with extension in a rostrocaudal manner to the adjacent segments. The observed pathological features demonstrated time-dependent differences with the greatest hemorrhage seen early following SCI. Maximal tissue loss was seen at 3–4 weeks following injury. These pathological features correlate with the clinical findings of acute severe SCI.13
Although a number of research studies have investigated the role of SP in a variety of different conditions,7 no research has investigated the role of SP as a mediator of neurogenic inflammation following human SCI. The current study demonstrates that SP is found predominantly within the Rexed lamina I and II (substantiagelatinosa) of the human dorsal horn, consistent with previous reports of SP expression within the human spinal cord.14 Assessment of the injured spinal cord segments revealed a significant decrease in SP immunoreactivity over time within the injury epicenter and the adjacent segments of the spinal cord. Such diminished SP immunoreactivity is likely due in part to the tissue loss observed at this time. Nonetheless, reduced SP persisted in areas of conserved tissue and as such suggests the release and subsequent depletion of the SP stores within the dorsal horn. Changes in the expression of SP have similarly been observed following disorders such as pain sensitivity.15 A depletion of SP stores from the substantia gelatinosa was observed in people affected with diminished pain sensitivity.15 Such a finding demonstrates that peripheral injury can alter the stores of SP within the spinal cord. Our present results are the first to demonstrate depletion of SP from the dorsal horn because of a direct injury to the spinal cord in humans.
It has been well established that SP exerts its effects on target cells via binding to the NK1 receptor.8 Furthermore, it has been demonstrated that the process of neurogenic inflammation is mediated by such binding.16 Indeed, in experimental models of TBI9 and ischemic stroke,10 inhibition of the NK1 receptor abated neurogenic inflammation thereby reducing BBB disruption and edema formation. Furthermore, depletion of SP via administration of capsaicin similarly demonstrated reduced BBB disruption and edema formation following TBI.16 Localization of the NK1 receptor within the spinal cord has been extensively investigated in rats using in situ hybridization17 and immunocytochemistry techniques.18 These studies demonstrated the highest density of NK1 binding sites in Laminae I-II of the dorsal horn, intermediolateral cell column and lamina X. Also noted was moderate labelling of the ventral horn regions. Until now, no research has been performed to confirm such localization within the human spinal cord.
In contrast to experimental research, our results demonstrate little NK1 immunoreactivity within the dorsal horn region of the human spinal cord, with moderate immunoreactivity observed within the ventral horn neurons and the intermediolateral cell column. The vasculature of the white matter was comprehensively investigated to determine the possible role of SP as a mediator of neurogenic information. NK1 receptor immunoreactivity markedly increased immediately following injury within the injury epicenter and the adjacent segments. Thereafter, a gradual decrease was observed in all segments with immunoreactivity in the longer surviving cases comparable to control sections. These findings suggest that increased NK1 receptor immunoreactivity occurs in response to injury. Indeed, previous studies have demonstrated that exposure to a SP releasing stimulus increases expression of the NK1 receptor.19 This provides further support for the notion that the SP loss observed was in part due to SP release from the dorsal horn region. The binding of SP to the NK1 receptor mediates rapid endocytosis and internalization of the receptor.8 Therefore, the decreased NK1 receptor immunoreactivity in the longer surviving cases is likely due to increased SP binding given the observed depletion of SP immunostaining over time.
The genesis of edema following human SCI is thought to be vasogenic in nature given the reported presence of protein extravasation within the spinal cord tissue.11 However, this could not be accurately assessed in our post-mortem material. Claudin-5 is a major constituent of CNS endothelial cell tight junctions12 and as such was assessed to visualize the integrity of the BSCB within the human tissue. Claudin-5 immunoreactivity remained unchanged along the entire length of the spinal cord in the first 3 days following human SCI. However, a decrease was observed at 1 week and 3–4 weeks post-SCI, particularly, within the injury epicenter and immediate adjacent segments. This decrease may reflect a decline in tight junction integrity at these time points, or alternatively may be a reflection of continued tissue loss. No changes in claudin-5 were seen in the early phases post-SCI when BSCB has been found to be most disrupted, indicating that tight junction dysfunction is not responsible for the early large-molecule extravasation following SCI. Mechanical disruption of the BSCB or increased protein transcytosis across the endothelial cells may account for this early protein extravasation. Consistent with this view, claudin-5-deficient mice died within 1 day of birth with no macroscopic abnormalities or edema apparent, despite increased permeability to small molecules being evident.20 As such, although claudin-5 is an integral tight junction protein of the BSCB, tight junction dysfunction is unlikely to significantly contribute to early BSCB disruption following SCI. Nonetheless, decreased claudin-5, and thus tight junction integrity, is apparent after 1 week.
Conclusion
The current study demonstrates decreased SP immunoreactivity associated with an increase in NK1 receptor immunoreactivity, suggesting that there is a neurogenic inflammatory component following human SCI. These events may be associated with an increase in permeability of the BSCB in the absence of tight junction failure. Whether there is potential for an NK1 receptor antagonist to reduce acute BSCB permeability and edema formation after SCI warrants further investigation.
Data archiving
There were no data to deposit.
References
Tator CH, Duncan EG, Edmonds VE, Lapczak LI, Andrews DF . Changes in epidemiology of acute spinal cord injury from 1947–1981. Surg Neurol 1993; 40: 207–215.
Bozzo A, Marcoux J, Radhakrishna M, Pelletier J, Goulet B . The role of magnetic resonance imaging in the management of acute spinal cord injury. J Neurotrauma 2011; 28: 1401–1411.
Leypold BG, Flanders AE, Burns AS . The early evolution of spinal cord lesions on MR imaging following traumatic spinal cord injury. AJNR Am J Neuroradiol 2008; 29: 1012–1016.
Sharma HS . Early microvascular reactions and blood-spinal cord barrier disruption are instrumental in pathophysiology of spinal cord injury and repair: novel therapeutic strategies including nanowired drug delivery to enhance neuroprotection. J Neural Transm 2011; 118: 155–176.
Koyanagi I, Iwasaki Y, Isu T, Akino M, Abe H . Significance of spinal cord swelling in the prognosis of acute cervical spinal cord injury. Paraplegia 1989; 27: 190–197.
Campos MM, Calixto JB . Neurokinin mediation of edema and inflammation. Neuropeptides 2000; 34: 314–322.
Harrison S, Geppetti P . Substance p. Int J Biochem Cell Biol 2001; 33: 555–576.
O'Connor TM, O'Connell J, O'Brien DI, Goode T, Bredin CP, Shanahan F . The role of substance P in inflammatory disease. J Cell Physiol 2004; 201: 167–180.
Donkin JJ, Nimmo AJ, Cernak I, Blumbergs PC, Vink R . Substance P is associated with the development of brain edema and functional deficits after traumatic brain injury. J Cereb Blood Flow Metab 2009;; 29: 1388–1398.
Turner RJ, Helps SC, Thornton E, Vink R . A substance P antagonist improves outcome when administered 4 h after onset of ischaemic stroke. Brain Res 2011; 1393: 84–90.
Olsson Y, Ahlgren S, Farooque M, Holtz A, Li GL, Yu WR . Pathophysiology of spinal cord trauma: observations on vasogenic oedema and axonal injuries in human and experimental material. Neuropathol Appl Neurobiol 1996; 22: 518–520.
Morita K, Sasaki H, Furuse M, Tsukita S . Endothelial claudin: claudin-5/TMVCF constitutes tight junction strands in endothelial cells. J Cell Biol 1999; 147: 185–194.
Norenberg MD, Smith J, Marcillo A . The pathology of human spinal cord injury: defining the problems. J Neurotrauma 2004; 21: 429–440.
Przewlocki R, Gramsch C, Pasi A, Herz A . Characterization and localization of immunoreactive dynorphin, alpha-neo-endorphin, Met-enkephalin and substance P in human spinal cord. Brain Res 1983; 280: 95–103.
Pearson J, Brandeis L, Cuello AC . Depletion of substance P-containing axons in substantia gelatinosa of patients with diminished pain sensitivity. Nature 1982; 295: 61–63.
Nimmo AJ, Cernak I, Heath DL, Hu X, Bennett CJ, Vink R . Neurogenic inflammation is associated with development of edema and functional deficits following traumatic brain injury in rats. Neuropeptides 2004; 38: 40–47.
Maeno H, Kiyama H, Tohyama M . Distribution of the substance P receptor (NK-1 receptor) in the central nervous system. Brain Res Mol Brain Res 1993; 18: 43–58.
Nakaya Y, Kaneko T, Shigemoto R, Nakanishi S, Mizuno N . Immunohistochemical localization of substance P receptor in the central nervous system of the adult rat. J Comp Neurol 1994; 347: 249–274.
Mantyh PW . Neurobiology of substance P and the NK1 receptor. J Clin Psychiatry 2002; 63 (Suppl 11)): 6–10.
Nitta T, Hata M, Gotoh S, Seo Y, Sasaki H, Hashimoto N et al. Size-selective loosening of the blood-brain barrier in claudin-5-deficient mice. J Cell Biol 2003; 161: 653–660.
Acknowledgements
We acknowledge the financial support of the Neil Sachse Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Leonard, A., Manavis, J., Blumbergs, P. et al. Changes in substance P and NK1 receptor immunohistochemistry following human spinal cord injury. Spinal Cord 52, 17–23 (2014). https://doi.org/10.1038/sc.2013.136
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.136
Keywords
This article is cited by
-
A multi-staged neuropeptide response to traumatic brain injury
European Journal of Trauma and Emergency Surgery (2022)
-
When the Nervous System Turns Skeletal Muscles into Bones: How to Solve the Conundrum of Neurogenic Heterotopic Ossification
Current Osteoporosis Reports (2020)