Abstract
Study design
This is a narrative review of the literature on neurochemical biomarkers in spinal cord injury (SCI).
Objectives
The objective was to summarize the literature on neurochemical biomarkers in SCI and describe their use in facilitating clinical trials for SCI. Clinical trials in spinal cord injury (SCI) have been notoriously difficult to conduct, as exemplified by the paucity of definitive prospective randomized trials that have been completed, to date. This is related to the relatively low incidence and the complexity and heterogeneity of the human SCI condition. Given the increasing number of promising approaches that are emerging from the laboratory which are vying for clinical evaluation, novel strategies to help facilitate clinical trials are needed.
Methods
A literature review was conducted, with a focus on neurochemical biomarkers that have been described in human neurotrauma.
Results
We describe advances in our understanding of neurochemical biomarkers as they pertain to human SCI. The application of biomarkers from serum and cerebrospinal fluid (CSF) has been led by efforts in the human traumatic brain injury (TBI) literature. A number of promising biomarkers have been described in human SCI whereby they may assist in stratifying injury severity and predicting outcome.
Conclusions
Several time-specific biomarkers have been described for acute SCI and for chronic SCI. These appear promising for stratifying injury severity and potentially predicting outcome. The subsequent application within a clinical trial will help to demonstrate their utility in facilitating the study of novel approaches for SCI.
Similar content being viewed by others
Introduction
In 2007, an international panel, supported by multiple foundations, under the banner of International Campaign for Cures of Spinal Cord Injury Paralysis published a set of papers reviewing spinal cord injury (SCI) clinical trial methodology, and providing recommendations for future studies [1,2,3,4]. Almost a decade later, several foundations (see Funders) sponsored another meeting to address both new and persistent barriers to translational research success in SCI. One result of this coalition was establishment of a new initiative, the Spinal Trials Understanding, Design, and Implementation (STUDI) group, to consider and report on ways to improve participant recruitment, study protocol design and trial outcome measures, including electrophysiology, imaging and biomarkers. These reports are to be presented in a series of papers, including the current work, which specifically addresses recruitment issues and strategies for SCI clinical trials. The first paper of this series was published in the spring of 2019 and discussed the challenges to recruitment for clinical trials [1]. This paper addresses the importance of biomarkers in facilitating the conduct of clinical trials. This serves as an update to an excellent review of neurochemical biomarkers published in 2017 by Hulme et al. [2], with an additional focus on the use of biomarkers in clinical trials.
Clinical trials in acute traumatic SCI are challenged by the relatively low incidence of the injury and the limited sensitivity of functional outcome measures, thus creating a significant barrier to translational research. There are many aspects that contribute to the difficulty in conducting clinical trials to translate novel treatment to human SCI (tackled in the various STUDI manuscripts). The concept of identifying and using biomarkers in SCI clinical trials is related to some of the very fundamental challenges in human neurotrauma, where interventions are tested in a clinical population that is inherently quite heterogeneous and that experiences highly variable natural recovery. SCI biomarkers can help categorize and stratify patients’ initial severity of neurologic impairment and predict the extent of spontaneous/natural neurological and functional recovery. Biomarkers may also be used to track SCI progression and as measures of biological responses to treatment throughout the lifetime of a person with SCI. At present most of the available data refer to biomarkers during the acute phase after injury, and there is less information of biomarkers that might monitor the recovery and chronic phases. To this end, this paper will describe the basic principles behind the application of biomarkers for SCI and how such biomarkers may help to overcome these challenges. We will then describe ongoing work in the field of neurochemical biomarkers detected in biofluids (distinct from imaging biomarkers such as MRI measures which are covered in a separate paper). Finally, we will provide some practical recommendations for the SCI research community based on the current state of knowledge.
Why are biomarkers of SCI needed?
At first glance, it would be easy to question why biomarkers are even needed in SCI (specifically in complete SCI)—for even to a layperson, many of the neurologic deficits incurred from suffering an acute SCI are fairly obvious, and the prognosis for neurologic recovery is ostensibly poor. Historical data that documented the recovery of SCI in the rehabilitation setting reported very low rates of spontaneous recovery from “complete” paralysis, suggesting that prognosticating neurologic outcome after acute SCI was relatively straightforward [3]. If this were indeed true and spontaneous neurologic recovery was both modest and predictable, then it should be possible in acute clinical trials to discern the neurologic improvements that could be attributable to a novel drug treatment, for example. And yet, when looking back at the experience of the SCI field, only four large-scale clinical trials in acute SCI have ever been completed—three evaluating methylprednisolone and one evaluating GM-1 ganglioside. Despite the many decades over which these studies were run, the entire cohort of individuals with acute SCI enrolled in these four trials falls short of 2500. A number of more recent attempts to run acute clinical trials have ended prematurely, due to difficulties in enrolling participants and/or detecting a promising signal of efficacy. The STUDI series of papers addresses many of these difficulties. However, in the context of biomarkers, the first challenge is to address the limitations of the functional examination of neurologic impairment in SCI, which is indeed one of the primary motivations for identifying biomarkers in the acute phase of SCI. Aside from prediction of outcome, biomarkers that are sensitive to ongoing processes of recovery such as neural plasticity/sprouting would be extremely helpful in clinical trials as they could be used to biologically monitor treatment responses.
Currently, the best predictor of long term neurologic outcome is the initial extent of neurologic impairment, as measured with the International Standards for Neurological Classification of SCI (ISNCSCI) examination. The ISNCSCI examination represents the “gold standard” in assessing the neurologic impairment of a spinal cord injured individual. Performing a full ISNCSCI exam, however, is time-consuming and requires substantial training by the examiner in order to have consistent, reliable assessments. The ISNCSCI exam was not designed to be necessarily predictive of overall function, and it is well known that changes in american spinal injury association impairment scale (AIS) grade may not indicate meaningful changes in abilities to perform activities of daily living [4]. However, in the context of clinical trials, the ISNCSCI examination has served as the foundational outcome measure, with an improvement in AIS grade and/or an increase in motor score historically utilized as a manifestation of therapeutic efficacy. It should be acknowledged that, as a field, we are fortunate to have an international standard for the conduct of this clinical examination and a common language to communicate (and study) neurologic impairment. But our heavy reliance upon this clinical examination has many limitations and implications for the field, and has served as an obstacle to clinical trial execution (and thereby translational research).
Firstly, the ISNCSCI examination is impossible to perform in many acutely injured SCI patients. The examination is relatively time-consuming and relies on the conscious participation of the recently traumatized patient, who may present to the emergency room unconscious, intoxicated, sedated, intubated, and with multiple other injuries (including potentially a traumatic brain injury)—all of which may affect a patient’s ability to participate in an ISNCSCI examination. While a clinical trial might stratify acute SCI patients based on whether they present as AIS A, B, or C injuries, the distinction between the three grades may only be the presence of deep anal pain sensation on the rectal examination and the subtle ability to voluntarily flex a toe on the motor exam—findings that may be impossible to detect in an intubated polytrauma patient. It is true that the inability to precisely evaluate neurologic impairment and assign motor/sensory scores and AIS grade may not have a major impact on the immediate clinical decision making (for example, on whether or not surgery is indicated), but without a baseline severity of injury, these patients typically cannot be recruited into acute clinical trials. A conservative estimate indicates that about a third of all patients are rendered ineligible to participate in acute clinical trials based on these considerations [5]. So, right off the mark, the acute clinical trials are hamstrung by this recruitment limitation. A set of acute biomarkers that make it possible to stratify patients for admission to clinical trials would therefore be useful both for recruitment and for clinical care decisions.
Secondly there is a need for later stage biomarkers that monitor recovery and treatment effects. Even when the ISNCSCI examination can be performed and a baseline level of neurologic impairment assigned, neurologic recovery is not necessarily easy to predict, especially very early post injury, when acute clinical trials require a baseline evaluation. This therefore mandates that large numbers of subjects be enrolled in acute clinical trials in order to distinguish treatment effect from the sheer variation in spontaneous neurologic recovery [6]. Such recruitment can take many years to achieve sufficient power to assess treatment efficacy. Perhaps even more problematically, early-stage, small clinical trials that are primarily meant to assess feasibility and/or safety have difficulty detecting a “signal” of treatment efficacy because of this variability in neurologic recovery. This makes the subsequent decision to proceed to a large-scale definitive Phase 3 study much harder, as it may not be possible to determine whether the treatment had the desired biological or functional effect in small cohort of subjects recruited.
Thirdly, because the variation in spontaneous neurologic recovery is so high, it can be very difficult in small scale, early phase I or II trials of acute SCI to determine if there is an “efficacy signal”. For individuals “incomplete” injuries (AIS B, C, and D) who theoretically are best suited to novel therapies that might leverage the spared neurologic function, their recovery is particularly heterogeneous and difficult to predict accurately, and there may be ‘ceiling effects’ of detecting their neurologic improvement with the ISNCSCI exam. This may also be true—to a lesser extent—for individuals in the chronic phase of living with SCI, where subtle spontaneous changes may still occur. Without being able to detect a signal of therapeutic efficacy in small trials, decisions to go forward into an even lengthier and costlier definitive clinical trial are hampered by limited information about whether the therapeutic agent had the desired effect at the given dose and time window of administration. Having a biomarker of therapeutic effect would be very helpful in this regard for informing the clinical trial design. Of course, having such a biomarker of therapeutic effect in human SCI would require that the mechanism of action underlying the particular treatment was well established in preclinical models and then could be then directly interrogated in the clinical setting. The interrogation in humans is limited by the accessibility of human spinal cord tissue for direct observation, thus mandating the investigation of biofluids such as cerebrospinal fluid (CSF) or blood. Given the myriad of therapeutic approaches that can be considered for SCI, it is unlikely that there will be a single “biological surrogate outcome measure” for SCI; rather, a biomarker of therapeutic effect would need to be established based on the known (or hypothesized) mechanism of action of the specific treatment in question.
Given these described limitations of the ISNCSCI examination in the clinical trial setting, biomarkers would be helpful for clinical trials by: (1) objectively stratifying injury severity during the acute stage where neurologic assessment is often impossible to perform, (2) more accurately predicting the extent of neurologic recovery, and (3) serving as biological surrogate outcome measures for identifying therapeutic effect. Biomarkers may also serve as potential therapeutic targets. In other words, factors that are elevated in those with poor recovery may provide insights on pathways that should be neutralized, while factors that are elevated in those with good recovery may identify processes or biological responses that would be desirable to augment. An example would be the evaluation of inflammatory cytokines post injury and how they respond to an antiinflammatory treatment. This is true in the chronic as well as acute phase of SCI. As an adjunct to establishing these tools, the search for neurochemical biomarkers in human biofluids also has the additional broad translational motivation of characterizing and understanding the pathophysiologic effects of SCI in human patients, which assists in the identification of therapeutic targets.
While the limitations of the ISNCSCI examination in the very acute SCI setting provide the rational for biomarkers in the acute clinical trial setting, there may also be a role for biomarkers at more subacute or chronic time points, reflecting the fact that the injury responses are dynamic and definitely change over time. Biomarkers at more subacute and chronic time points could be helpful for identifying appropriate candidates for interventions that might, for example, encourage neuroplasticity, or reduce chronic neuroinflammation within the cord. However, there are currently more data available about neurochemical biomarkers in the acute setting than in the subacute or chronic setting simply because obtaining biological samples from individuals with SCI is practically much easier to do when they are within their acute hospitalization than when they are back in the community. While it might seem obvious, it should emphasized here that in discussing the potential utility of biomarkers in clinical trials or decision-making, their application is very time-specific. In this regard, the utility of a specific biomarker (or panel of biomarkers) is also quite dependent upon the clinical trial design, with some trials enrolling patients very soon after injury (i.e. the typical “neuroprotection” trial), whereby others trials (particularly for “neuro-regenerative” treatments) might enroll patients in the subacute stages of injury when the baseline neurologic status is more clearly defined. For acute clinical trials where a baseline must be established early, the biomarkers of injury severity and predictors of outcome are particularly important. For subacute and chronic clinical trials, biomarkers may be more helpful for discerning appropriate candidates and following the responses to treatment.
Neurochemical biomarkers—state of the art in neurotrauma
In the setting of neurotrauma, the identification and establishment of biomarkers in acute SCI is relatively underdeveloped as compared to that in acute traumatic brain injury (TBI). This is likely attributable to the much greater incidence of TBI and the routine acquisition of CSF from external ventricular drains—making it possible to identify biomarkers within the CSF and determine if they are detectable within the blood compartment. First, we will briefly discuss the state of TBI biomarker research to provide and overview of how the TBI field has progressed with regards to the identification of diagnostic and prognostic biomarkers. This will provide some context to the subsequent discussion on the state of SCI biomarker research. A comprehensive description of TBI biomarkers is beyond the scope of this paper, but if sought, the reader is directed to recent reviews on this topic [7]. In addition, biofluid-based biomarkers for neurotrauma can include protein, microRNA, circulating nucleic acids, metabolomic aned exosome/microvesicle-encapsulated biomarkers [7]. These markers in general represent molecules released from damaged cells and the acute inflammatory response (acute markers), molecules released during the cellular and immunological response while healing the injury (subacute) and longer-term responses which are mostly immunological. Since protein biomarkers are by far the most studied and advanced, the scope of this review will focus mainly on this class of neurochemical biomarkers.
Neurochemical biomarkers in TBI and potential application in SCI
Because the brain and spinal cord represent tissue of the central nervous system (CNS), there are important conceptual similarities in their responses to physical trauma with respect to the biomolecules that are released into the CSF and blood compartments. There are a number of protein biomarkers that are CNS-enriched or CNS-specific that have been shown to be potentially applicable in both human and/or animal models of TBI and SCI. These markers are conceptually promising as biomarkers of neurotrauma as they potentially reflect specific CNS injury sequelae, such as neuronal cell body or axonal injury, demyelination or myelin injury, and astrocyte integrity compromise (cell wounding, see below), cell death or astrogliosis (summarized in Table 1).
The identification of protein biomarkers in acute TBI has been accomplished through both broad mass spectrometry approaches [8,9,10,11,12] and also with more narrow, targeted approaches that evaluate specific biomarker candidates [12, 13]. For example, UCH-L1 (ubiquitin carboxy-terminal hydrolase L1) and GFAP (glial fibrillary acidic protein) have been routinely demonstrated as diagnostic biomarkers in human and animal TBI studies [14,15,16,17,18,19,20,21,22]. Importantly, the extensive study of UCH-L1 and GFAP in TBI has culminated in the FDA approval in February 2018 of a serum biomarker test for mild TBI (the “Brain Trauma Indicator”, Banyan Biomarkers, San Diego, CA) [23]. This test of combined UCH-L1 and GFAP not only can distinguish mild TBI from no injury controls, but can also distinguish those mild TBI subjects with CT-detectable pathoanatomical lesions from those that are CT normal [24].
One lesson from the TBI biomarker field is that, generally speaking, protein markers found in the CSF of patients with severe TBI are also detectable in the blood compartment (serum and plasma). Such protein markers include UCH-L1, GFAP, S100β, phosphorylated neurofilament heavy chain (pNF-H), myelin basic protein (MBP), alphaII-spectrin breakdown products (SBDP), and several others [7]. A number of these, including UCH-L1, GFAP, Tau, S100β, and SBDP/SNTF, are also detectable in serum at lower concentrations after mild TBI/concussion and have clinical diagnostic properties [24]. This is obviously of clinical significance because of the relative ease of obtaining blood samples in comparison to obtaining CSF samples in both TBI and SCI patients. There is no question that while the CSF may be more directly representative of the CNS injury, a blood-based test would be much preferred. In essence, identifying biological aspects that are specific to the CNS injury, then determining whether these can be detected in serum/plasma in concentrations that reflect injury severity and/or outcome has been central to the field of TBI biomarker research. These important lessons and findings in TBI biomarker work will also hopefully translate to SCI biomarker discovery and clinical validation studies. In principle there must be similarities between TBI and SCI given the underlying injury to neural tissue. However, in SCI the volume of CNS tissue affected is smaller than in the brain, leading to a smaller release of CNS material and a smaller effect of these on serum levels. At later stages the widespread changes to musculo-skeletal tissues after SCI will be dominant.
Biomarkers of Acute SCI
We and others have investigated blood and CSF from acute SCI patients in an effort to establish neurochemical biomarkers of acute SCI. CSF being closer in proximity to the injured spinal cord is intuitively more representative of the parenchymal injury. However, because CSF is not routinely collected in the clinical management of SCI (unlike in TBI where it is easily obtained in patients with external ventricular drains), human biomarker studies that examine CSF from SCI patients have been relatively limited and typically involve a fairly small number of patients.
An example of this is a paper by Yokobori et al. [25], where they conducted a literature review of biomarkers for SCI but also reported on seven acute SCI patients whose CSF was evaluated to measure UCH-L1, SBDP, MBP, and GFAP [25]. They reported that all four proteins were elevated transiently in the CSF, and there was a correlation between GFAP levels and SCI injury severity and recovery. Subsequent work from this same group employed a broader proteomics approach to biomarkers discovery in both rodent and human CSF samples. This work identified additional protein biomarker candidates such as transferrin, cathepsin D, triosephosphate isomerase-1, and astrocytic phosphoprotein PEA-15 that were found to be elevated in both rodent and human SCI [26]. PEA15 is also shown to be released from wounded mouse and human astrocytes in an in vitro trauma model associated with depletion from integrity-compromised astrocytes [11, 12]. Interestingly, PEA15 is also depleted acutely after mouse crush SCI injury followed by upregulation during subsequent reactive astrogliosis [11]. Since PEA15 is also elevated in in CSF and blood of moderate-to-severe TBI patients as well as within hours after injury in serum of mild TBI patients, this is another example of a biomarker of both SCI and TBI (Table 1, [12]).
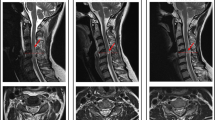
There has been considerable interest in CSF biomarkers of acute SCI in Vancouver, BC, Canada, that began with the initiation of a clinical trial of CSF drainage with intrathecal catheters after acute SCI (ClinicalTrials.gov: NCT01279811) [27]. CSF samples were obtained over 3 days and analyzed with ELISAs and Luminex bead assays to characterize the temporal pattern expression of a series of inflammatory cytokines (e.g. interleukin (IL)-6, IL--8, and monocyte chemotactic protein (MCP)-1) and structural proteins (tau, S100β, and GFAP) (Fig. 1a) [28]. At 24 h post injury, it was found that these proteins were distinct between AIS A, B, and C grades (Fig. 1b) and could be used in an ordinal logistic regression model to classify baseline AIS grade with an accuracy of 89%. In this study, the “baseline AIS grade” was determined by specifically trained spine research nurses based on the initial examination of the patient in the emergency room (i.e. before the patient went to the operating room and had the first sample of CSF drawn).
CSF biomarkers after acute SCI. a. CSF concentrations of inflammatory cytokines and neural/glial proteins over the first 3–5 days post injury. Note that the concentrations are very time dependent, with the greatest increases occurring immediately after injury, then subsiding back to baseline levels within days. This suggests that the proteins are largely released from cells damaged at the time of injury and “spilled” into the surrounding CSF. b. CSF biomarker concentrations at 24 h post injury are dependent upon injury severity. (From Kwon et al, J Neurotrauma 2010, permission granted by Mary Ann Liebert, Inc. New Rochelle, NY)
Subsequent studies that focused on the CSF collected around the 24-h postinjury time point revealed that these proteins were also distinct between those who improved (“converted”) an AIS grade and those who did not (Fig. 2) [29]. Using the inflammatory proteins and structural proteins in a prediction model could predict AIS grade conversion with an accuracy rate of 83.3%. Importantly, even amongst AIS A patients, the concentrations of the CSF biomarkers IL-6 and S100β were significantly different in those who did or did not improve over time, indicating that the biology (as represented by the CSF biomarkers at this 24 h time point) could distinguish recovery potential at 6 months post injury within this group with the same baseline severity of neurologic impairment. This finding indicates that even within the most severely injured “phenotype” of AIS A, there is considerable heterogeneity in terms of injury severity and neurologic prognosis that can be characterized biologically with neurochemical biomarkers. Certainly, the ability to predict outcome and identify patients with the potential to recover most likely with the current standards of care would be useful for early clinical trials to stratify their inclusion. Clinical trials with longer inclusion time windows may be able to utilize a baseline neurological examination at, for example, 72 h to 1 week post injury—in such cases, an early biomarker at 24 h may not be as useful. However, in acute clinical trials, such early biomarkers of injury severity are likely to play an important role.
CSF biomarkers are significantly higher in those who do not convert their AIS grade (NO) as compared to those who do (YES). The y-axis is a log 10 scale, so that a one-point difference is a 10× difference in concentration. Modified from Kwon et al. [29]
Based on the biomarkers, individuals who would be predicted to experience recovery might also be the most likely to benefit from novel treatments targeting a particular pathway. Conversely, for patients predicted by their biomarker profile to experience little spontaneous recovery with the current standards of care, therapeutic improvement from a novel treatment might be more clearly detectable—this may in fact be the most practical advantage of utilizing biomarkers in early clinical trials where the small sample size limits the ability to discern therapeutic effect. Acute cell injury/cell death released biomarkers that rise within minutes and early hours postinjury bear the potential to differentiate between tissue compromise and atrophy (see below; [12]). Such injury-defined biomarkers may be able to capture lateral white matter sparing that is critical for any degree of functional recovery later on.
While these studies describe the investigation of a discrete series of proteins within the CSF, there is also great interest in more broadly screening CSF (and blood) for other neurochemical biomarkers, to determine new diagnostic and prognostic biofluid injury signatures. For example, proteomic studies are emerging that report distinct patterns of protein release after neurotrauma in TBI and SCI [12, 26]. Such larger scale investigations of the proteome, metabolome, or genome may reveal ‘biomarker signatures’ that could be helpful for distinguishing injury severity, predicting outcome, or highlight targets for intervention that could be used as a biomarker of therapeutic response [30,31,32]. These ‘omic’ studies may also help to resolve which biomolecules could be studied in the blood rather than in CSF, although it is recognized that the detection of biomarkers is very challenging in serum/plasma samples due to the high abundance of nontrauma related proteins that require significant sample depletion and processing to detect low-abundant SCI associated biomarkers.
Data from the Vancouver group show that biomarkers elevated in the CSF may also be elevated in the blood, but at levels several orders of magnitude lower, the challenge is in detecting biomarker signals within blood that are both specific to the injury and prominent enough to be detected over the systemic injury response of the human patient [28]. Kuhle et al. [33] reported in 27 acute SCI patients that serum neurofilament light chain concentrations were closely correlated with injury severity and that the minocycline treatment appeared to reduce these concentrations. This study importantly reveals the potential utility of using a biomarker as a surrogate measure of biological effect from a pharmacological treatment. Ahadi et al. [34] reported in 35 acute SCI patients that GFAP, pF-H, and neuron specific enolase (NSE) were elevated in the serum, and that GFAP levels were correlated with injury severity. In individuals with acute SCI, Bloom et al. identified elevated levels of inflammatory cytokines, macrophage migration inhibitory factor (MIF) and high mobility group box 1 (HMGB1), regardless of injury level or grade, which raises the concept that while some factors elevated acutely after SCI may have potentially importent biological effects, not all will necessarily serve as biomarkers of injury severity [35, 36].
At this stage, there is a paucity of data around comparative serum levels of the proteins that have been thus far identified in the CSF after acute SCI. This may relate in part to the relatively small “volumetric damage” of the injured spinal cord as compared to the injured brain in TBI patients. With a smaller volume of tissue damage in the spinal cord, there may not be sufficient concentrations of proteins released into the systemic circulation to be readily detected as a biomarker signal. Nonetheless, work to investigate blood biomarkers is definitely worthwhile and ongoing.
Biomarkers in chronic SCI
While there are 17,000 new persons with traumatic SCI each year in the US, there are more than 350,000 persons living with chronic SCI, typically defined as at least 1 year from initial injury [37]. There are currently 18 clinical trials of cells, drugs, and surgical interventions and 55 rehabilitation and technology to improve neurological and functional outcomes for people in the chronic phase of living with SCI (link to SCOPE tables updated March 2018). Similar to acute trials, the AIS grade based upon an ISNCSCI examination is typically part of the inclusion criteria for trials in the chronic phase of SCI.
In contrast to the acute trauma setting, scheduling of the ISNCSCI examination and obtaining a more reliable ISCNSCI exam is much easier in the chronic phase of SCI. However, people with the same AIS grade and neurological level of injury may have different neuropathologic patterns of injury, different biochemical profiles (Fig. 3), different genetic backgrounds, and different medication profiles, all of which may influence potential efficacy of therapeutic interventions. The biomarker profile in chronic phase people will be influenced greatly by events outside the spinal cord, for instance local infections, respiratory, and cardiovascular events. The confluence of all of these different factors of course confounds the interpretation of serum inflammatory biomarkers in the chronic condition, and undoubtedly contributes to the variability that is demonstrated in Fig. 3. This of course will be a significant challenge for the biomarker field in developing markers that are meaningful representations of the biology of the SCI at these chronic time points. Utilizing biomarkers in the chronic setting to test experimental interventions will need to accommodate variations in standard care treatments. For example, neuropathic pain is experienced by most persons living with SCI, but clinical responsiveness to available pain medications is poor and variable [38]. It is reasonable to suggest that SCI consumers would be better served by a personalized medicine approach whereby persons with elevated panels of biomarkers of pain were treated with drugs that were prescribed according to proposed mechanisms of pain generation.
Individuals with chronic SCI with the same AIS grade have heterogeneous levels of immune mediators. MIF, MIG, MCSF, and IL-3 were significantly elevated in individuals with chronic (≥1 year from initial injury) SCI as compared to uninjured individuals [43]. Here, we show the levels of immune mediators by AIS grade: A (n = 14), B (n = 0), C (n = 3), D (n = 5). Levels of (A) MIF P < 0.27 (B) MIG/CXCL9, P < 0.01 (C) MCSF, P < 0.03 (D) IL-3, P < 0.3 by AIS group. *P < 0.01. P values determined by Kruskal–Wallis test, with multiple comparisons. Symbols represent a single plasma sample from each subject. Data abstracted from Stein et al. [43]
Since CSF is rarely obtained for clinical purposes in the chronic phase of living with SCI, sera has been the most common biological fluid sampled. Kwon et al. [28] demonstrated that in persons with acute SCI, levels of inflammatory mediators in blood mirrored those in CSF, albeit at concentrations at least tenfold lower [28]. Given the pivotal role of systemic inflammation in promoting many of the medical consequences of SCI (e.g. neuropathic pain, type II diabetes, elevated risk of heart disease), the fact that many inflammatory mediators are directly neurotoxic at high levels, and the ease of obtaining sera from this population, most data on potential biomarkers in chronic SCI have focused on immune mediators in sera.
In a study examining the relationship of cytokine levels to pressure ulcers in persons with chronic SCI, circulating plasma levels of IL-6, IL-2R, and ICAM-1 were significantly elevated in participants with chronic SCI as compared to able-bodied controls [39]. In that study, cytokine levels were higher in participants with slow resolving pressure ulcers. In a later study implicating the IL-2 pathway, participants with chronic SCI had higher levels of IL-2 and TNFα than able-bodied controls [40]. Subsequently, persons with chronic SCI were shown to have higher levels of C reactive protein, but not IL-6 or TNFα, than able-bodied controls [41]. In a larger study, elevated serum levels of IL-6 and TNFα were confirmed, as significantly elevated as compared to able-bodied controls, but not IL-2, IL-4, or IL-10 [42]. Supporting the concept of inflammatory mediators as biomarkers, persons with SCI with the highest levels of IL-6 or IL-1RA had neuropathic pain, urinary tract infections, or pressure ulcers. As mentioned above, two potent pro-inflammatory cytokines that are present constitutively at high amounts in both neuronal and immune cell types, MIF and HMGB1, were found to be elevated in all participants with chronic SCI, regardless of injury severity or level [36, 43].
To date, there have been two independent functional genomics studies performed in persons with chronic SCI [44, 45]. The first was a study of leukocyte gene expression in 13 males with chronic SCI and 7 able-bodied men that showed elevated expression of autoimmune-promoting cytokines, A Proliferation-Inducing Ligand (APRIL), B-cell Activating Factor (BAFF) and B-cell Maturation Antigen (BCMA) [45]. The second functional genomics study in chronic SCI was of 31 individuals with SCI and 26 able-bodied individuals (males and females) identified broad changes in whole blood gene expression of persons with chronic SCI, including a dramatic reduction in NK cell genes and upregulation of proinflammatory genes [44]. Another interesting observation from this study was that several factors identified by Kwon et al. [28] as elevated in acute SCI were also elevated in persons with chronic SCI, such as S100A9, ENO2, and B2M [46]. This prompts the question of how biomarkers elevated acutely relate to biochemical changes made during or sustained through the chronic phase of SCI. Validating the potential impact of this approach on clinical care, this study also identified genes elevated in persons with chronic SCI that are targets of already FDA-approved drugs, such as JAK2 and the beta adrenergic receptor [44].
Emerging concepts in identifying “cell-specific” biomarkers of acute SCI
While the discussion to this point has primarily been around human TBI and SCI markers of injury, it is also acknowledged that in the development of biomarkers specific to SCI, an intuitive approach is to measure proteins that are specific to cells within the CNS. One emerging approach has been to examine astrocyte-specific proteins as biomarkers of acute SCI. Astrocytes are as abundant as neurons and make up a substantial protein mass in the CNS, which increase the chances for astrocyte and thereby CNS-specific protein detection in biofluids [47]. Levine and colleagues identified over 59 astroglial proteins with significant changes in fluid around traumatized mouse astrocytes using a targeted quantitative proteomic approach in a stretch-injury culture model [11, 48]. Aldolase C (ALDOC) and the astroctytic phosphoprotein 15 (PEA15) are depleted from injured astrocytes after SCI in perilesional astrocytes as examples, and both are elevated in fluids after trauma [11]. Selecting for astrocyte-enriched proteins from the trauma-release proteome yielded a small panel of new candidate neurotrauma biomarkers that include ALDOC, brain lipid binding protein (BLBP), also called brain fatty acid binding protein (FABP7), glutamine synthetase, PEA15 and small breakdown products (BDPs) of GFAP [12]. The temporal pattern of release of these astrocyte-specific proteins may provides insights into distinguishing stages of cell injury and cell death after trauma (Fig. 4). Recent data obtained from a swine contusion SCI model reveal significant CSF elevation of ALDOC and BLBP in addition to the known biomarker GFAP (Fig. 5). This analysis in pig SCI reveals a kinetic patterns of prolonged ALDOC elevation and rapid GFAP decline—a temporal profile similar to that seen in TBI patients [12, 49]. It is again worth pointing out here that the timing is very important in interpreting these biomarkers, such that biomarkers obtained very early (e.g. 12 h post injury) and at a subacute time frame (e.g. 72 h post injury) are likely to be very different and therefore should be only applied to the time frame at which they were measured.
Release stages of astrocyte injury biomarkers. Traumatic shear and stretch forces inflict acutely membrane disruption, cell wounding, as well as cell death, with lysis, both cause astrocyte protein release. Protracted astrocyte cell death leads to additional delayed protein release. Surviving traumatized astrocytes can become reactive
Kinetic profile of astrocyte injury biomarkers in CSF after swine contusion SCI. Shown are Immunoblot optical densities (OD) of biomarkers GFAP, aldolase C (ALDOC) and brain lipid binding protein (BLBP) in CSF of contused (red) and sham (gray) swine. Plotted are temporal profiles of medians and 68% confidence intervals (±1 SEM) at baseline (BS), 20 min (min), 2.7 h (h), 2 and 7 days (d) post SCI on log-spaced axes. Mixed repeated measures ANOVA (unequal variances) document significant differences between sham and SCI (gray/red asterisks) as well as over time (red and gray asterisks on lines). Largest effect sizes (1.2–2.1) occur acutely after SCI for all three biomarkers (GFAP and ALDOC at 20 min and for BLBP at 2.7 h post SCI)
Neurochemical biomarkers in SCI: Where to from here?
There is mounting evidence that the investigation of biofluids such as blood and CSF can reveal neurochemical biomarkers that provide insights into the biology of SCI. Such biomarkers provide objective measures of injury severity, predictors of neurologic recovery, potential surrogate outcome measures for interventions, and possible therapeuutic targets. The question then becomes “how do we apply this to facilitate clinical trials in SCI?”.
It should be acknowledged at the outset that while the biomarkers reviewed in this paper show promise, none have undergone formal validation studies and so they remain investigational in nature. But to advance the field, it is necessary for future clinical trials—particularly early-stage trials—to at least start collecting such biofluids for the evaluation of biomarkers. It is clear that clinical trials will continue to depend upon the ISNCSCI examination for recruitment and stratification of subjects for clinical trials; there are no neurochemical biomarkers that could currently supplant this clinical examination. However, neurochemical biomarkers could certainly be measured in order to help balance treatment groups and interpret neurologic recovery in early-stage clinical trials. For example, in the Kwon et al. [29] study, the combination of inflammatory (IL-6, IL-8, and MCP-1) and ‘structural’ (tau, S100β, and GFAP) biomarkers in CSF could be used within a prediction model to correctly predict the failure to convert the AIS grade with an accuracy of over 90%]. While this still requires independent prospective validation, the measurement and analysis of these proteins could provide an investigator with important insights into whether the observed neurologic improvement in a clinical trial was related to the therapeutic intervention or to spontaneous recovery.
In addition to this, the collection of biofluids in clinical trials will allow for the testing of secondary hypotheses around mechanisms of action and potentially identify neurochemical biomarkers that are reflective of the treatment response. This too would facilitate early-stage clinical trials in both the acute and chronic phases of SCI. Of course, it is recognized that in order to do this, investigators must be encouraged and supported to collect biofluids in interventional SCI clinical trials and either develop their specific assays or establish collaborations for biomarker analysis. This would be the logical “next step” from prospective observational SCI studies such as the Canadian Multicenter CSF Pressure and Biomarker Study, “CAMPER” (ClinicalTrials.gov NCT01279811), the Biomarkers of Spontaneous Recovery from Traumatic Spinal Cord Injury, “SCI-MARK” (NCT02731027), and Transforming Research and Clinical Knowledge in SCI, “TRACK-SCI”, where biofluid collection occurs for the characterization of human biology after SCI and the identification/validation of neurochemical biomarkers.
Alongside these efforts, there are still questions to be addressed to establish useful neurochemical biomarkers for SCI:
1. Are combinations of biomarkers better than one single biomarker?
In theory, a combination of biomarkers that represents a “signature” of an injury “phenotype” would be a stronger biomarker tool than a single protein, metabolite, or gene, although this has yet to empirically proven. To some extent, efforts to date have been hindered by the typically small sample sizes in acute SCI, and so statistical methods to establish relationships between the biomarker being studied and clinical outcome generally utilize multiple biomarker candidates. For example, the UCLA team utilized factor analysis to decipher two distinct biomarker signatures in clinical neurotrauma biofluid data [12]. This is not to say, however, that in the end, two or three of the “strongest” biomarkers will form a clinically applicable biomarkers tool, as UCH-L1 and GFAP have done for distinguishing mild from severe TBI.
2. Should biomarkers be used as continuous variables or should there be arbitrary cut-off values to define separate categories?
This will to some extent depend upon the nature of the clinical “phenotype” that is being associated with the biomarker in question. One theoretical example would be the determination of the baseline severity of neurologic impairment in an individual who presents as a “complete” AIS A injury. Clearly, there is a degree of mechanical force that—when imparted violently to the spinal cord—causes sufficient parenchymal disruption so as to result in a complete AIS A SCI. Tripling this mechanical force may increase the parenchymal disruption, but the end result will be no different from a functional standpoint (still AIS A). Distinguishing these two injuries with biomarkers may be feasible; for example, we have shown that IL-6 and S100b were significantly higher in AIS A individuals who improved their AIS grade as compared to AIS individuals who did not. But whether there could be a “cut-off” applied whereby certain concentrations of IL-6 and S100β in the CSF at 24 h post injury could be utilized to distinguish two “classes” of AIS A individuals with different chances of neurologic recovery is yet to be seen. Again, this comes back to the notion that the use of neurochemical biomarkers remains investigational at this time, with none being clinically validated.
3. Will biomarkers be useful across different time points post injury?
Given that the pathophysiologic responses to cord injury change over time, it is pretty clear at this point in time that a biomarker of acute injury that might help in stratifying the injury severity of an obtunded, multi-trauma SCI patient is unlikely to be applicable to a chronically injured individual (and vice versa). Furthermore, while biomarkers of acute injury might be focused on damage to the spinal cord parenchyma and be utilized in clinical trials of neuroprotective interventions, useful biomarkers of chronic injury might be focused on secondary issues such as bone loss or muscle atrophy and be utilized in clinical trials to restore these tissues.
Despite the many questions that still remain, the translational importance of biomarkers should stimulate further efforts to collect biofluids from SCI patients and establish clinically useful tools to facilitate the validation of novel therapies in SCI. Given the huge cost of running clinical trials, it is understandable that investigators may be discouraged from adding biofluid collection component to their interventional studies, particularly when there is not yet a “validated” neurochemical biomarker. This will require some compromise at the level of funding/granting agencies where there must be acknowledgment of the early state of the biomarker field, but at the same time recognition of the translational importance biomarkers for facilitating interventional trials and the need to evolve from an entire generation of trials that have depended solely upon the neurologic examination of the patient (with all its aforementioned limitations). If we as a field cannot get past this, we will surely continue to witness the excruciatingly slow progress of clinical trials in SCI. Ultimately, a combination of neurochemical and imaging biomarkers may pave the way to a better understanding of a given patient’s injury and the ability to personalize his/her treatment.
References
Blight AR, Hsieh J, Curt A, Fawcett JW, Guest JD, Kleitman N, et al. The challenge of recruitment for neurotherapeutic clinical trials in spinal cord injury. Spinal Cord. 2019;57:348–59.
Hulme CH, Brown SJ, Fuller HR, Riddell J, Osman A, Chowdhury J, et al. The developing landscape of diagnostic and prognostic biomarkers for spinal cord injury in cerebrospinal fluid and blood. Spinal Cord 2017;55:114–25.
Marino RJ, Ditunno JF Jr., Donovan WH, Maynard F Jr. Neurologic recovery after traumatic spinal cord injury: data from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil 1999;80:1391–6.
van Middendorp JJ, Hosman AJ, Pouw MH, Van de Meent H. ASIA impairment scale conversion in traumatic SCI: is it related with the ability to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord 2009;47:555–60.
Lee RS, Noonan VK, Batke J, Ghag A, Paquette SJ, Boyd MC, et al. Feasibility of patient recruitment into clinical trials of experimental treatments for acute spinal cord injury. J Clin Neurosci 2012;19:1338–43.
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007;45:190–205.
Wang KK, Yang Z, Zhu T, Shi Y, Rubenstein R, Tyndall JA, et al. An update on diagnostic and prognostic biomarkers for traumatic brain injury. Expert Rev Mol Diagn. 2018;18:165–80.
Kobeissy FH, Ottens AK, Zhang Z, Liu MC, Denslow ND, Dave JR, et al. Novel differential neuroproteomics analysis of traumatic brain injury in rats. Mol Cell Proteom. 2006;5:1887–98.
Azar S, Hasan A, Younes R, Najdi F, Baki L, Ghazale H, et al. Biofluid proteomics and biomarkers in traumatic brain injury. Methods Mol Biol 2017;1598:45–63.
Shen S, Loo RR, Wanner IB, Loo JA. Addressing the needs of traumatic brain injury with clinical proteomics. Clin Proteom. 2014;11:11.
Levine J, Kwon E, Sondej M, Paez P, Czerwieniec G, Ao Y, et al. Traumatically injured astrocytes release a proteomic signature modulated by STAT3 dependent cell survival. GLIA 2016;64:668–94.
Halford J, Shen S, Itamura K, Levine J, Chong AC, Czerwieniec G, et al. New astroglial injury-defined biomarkers for neurotrauma assessment. J Cereb Blood Flow Metab. 2017;37:3278–99.
Lorente L. Biomarkers associated with the outcome of traumatic brain injury patients. Brain Sci. 2017;7:1–11.
Wang KK, Yang Z, Sarkis G, Torres I, Raghavan V. Ubiquitin C-terminal hydrolase-L1 (UCH-L1) as a therapeutic and diagnostic target in neurodegeneration, neurotrauma and neuro-injuries. Expert Opin Ther targets. 2017;21:627–38.
Papa L, Lewis LM, Silvestri S, Falk JL, Giordano P, Brophy GM, et al. Serum levels of ubiquitin C-terminal hydrolase distinguish mild traumatic brain injury from trauma controls and are elevated in mild and moderate traumatic brain injury patients with intracranial lesions and neurosurgical intervention. J Trauma Acute Care Surg. 2012;72:1335–44.
Zhang YP, Zhu YB, Duan DD, Fan XM, He Y, Su JW, et al. Serum UCH-L1 as a novel biomarker to predict neuronal apoptosis following deep hypothermic circulatory arrest. Int J Med Sci. 2015;12:576–82.
Liu MC, Akinyi L, Scharf D, Mo J, Larner SF, Muller U, et al. Ubiquitin C-terminal hydrolase-L1 as a biomarker for ischemic and traumatic brain injury in rats. Eur J Neurosci. 2010;31:722–32.
Papa L, Silvestri S, Brophy GM, Giordano P, Falk JL, Braga CF, et al. GFAP out-performs S100beta in detecting traumatic intracranial lesions on computed tomography in trauma patients with mild traumatic brain injury and those with extracranial lesions. J Neurotrauma. 2014;31:1815–22.
Lumpkins KM, Bochicchio GV, Keledjian K, Simard JM, McCunn M, Scalea T. Glial fibrillary acidic protein is highly correlated with brain injury. J Trauma. 2008;65:778–82. discussion82-4
Metting Z, Wilczak N, Rodiger LA, Schaaf JM, van der Naalt J. GFAP and S100B in the acute phase of mild traumatic brain injury. Neurology. 2012;78:1428–33.
Pelinka LE, Kroepfl A, Schmidhammer R, Krenn M, Buchinger W, Redl H, et al. Glial fibrillary acidic protein in serum after traumatic brain injury and multiple trauma. J Trauma. 2004;57:1006–12.
Vos PE, Jacobs B, Andriessen TM, Lamers KJ, Borm GF, Beems T, et al. GFAP and S100B are biomarkers of traumatic brain injury: an observational cohort study. Neurology. 2010;75:1786–93.
FDA authorizes marketing of first blood test to aid in the evaluation of concussion in adults [press release]. February 14, 2018.
Bazarian JJ, Biberthaler P, Welch RD, Lewis LM, Barzo P, Bogner-Flatz V, et al. Serum GFAP and UCH-L1 for prediction of absence of intracranial injuries on head CT (ALERT-TBI): a multicentre observational study. Lancet Neurol. 2018;17:782–9.
Yokobori S, Zhang Z, Moghieb A, Mondello S, Gajavelli S, Dietrich WD, et al. Acute diagnostic biomarkers for spinal cord injury: review of the literature and preliminary research report. World Neurosurg. 2015;83:867–78.
Moghieb A, Bramlett HM, Das JH, Yang Z, Selig T, Yost RA, et al. Differential neuroproteomic and systems biology analysis of spinal cord injury. Mol Cell Proteom. 2016;15:2379–95.
Kwon BK, Curt A, Belanger LM, Bernardo A, Chan D, Markez JA, et al. Intrathecal pressure monitoring and cerebrospinal fluid drainage in acute spinal cord injury: a prospective randomized trial. J Neurosurg Spine. 2009;10:181–93.
Kwon BK, Stammers AM, Belanger LM, Bernardo A, Chan D, Bishop CM, et al. Cerebrospinal fluid inflammatory cytokines and biomarkers of injury severity in acute human spinal cord injury. J Neurotrauma. 2010;27:669–82.
Kwon BK, Streijger F, Fallah N, Noonan VK, Belanger LM, Ritchie L, et al. Cerebrospinal fluid biomarkers to stratify injury severity and predict outcome in human traumatic spinal cord injury. J neurotrauma. 2017;34:567–80.
Tigchelaar S, Streijger F, Sinha S, Flibotte S, Manouchehri N, So K, et al. Serum microRNAs reflect injury severity in a large animal model of thoracic spinal cord injury. Sci Rep. 2017;7:1376.
Streijger F, Skinnider MA, Rogalski JC, Balshaw R, Shannon CP, Prudova A, et al. A targeted proteomics analysis of cerebrospinal fluid after acute human spinal cord injury. J Neurotrauma. 2017;34:2054–68.
Wu Y, Streijger F, Wang Y, Lin G, Christie S, Mac-Thiong JM, et al. Parallel metabolomic profiling of cerebrospinal fluid and serum for identifying biomarkers of injury severity after acute human spinal cord injury. Sci Rep. 2016;6:38718.
Kuhle J, Gaiottino J, Leppert D, Petzold A, Bestwick JP, Malaspina A, et al. Serum neurofilament light chain is a biomarker of human spinal cord injury severity and outcome. J Neurol Neurosurg Psychiatry. 2015;86:273–9.
Ahadi R, Khodagholi F, Daneshi A, Vafaei A, Mafi AA, Jorjani M. Diagnostic value of serum levels of GFAP, pNF-H, and NSE compared with clinical findings in severity assessment of human traumatic spinal cord injury. Spine 2015;40:E823–30.
Bank M, Stein A, Sison C, Glazer A, Jassal N, McCarthy D, et al. Elevated circulating levels of the pro-inflammatory cytokine macrophage migration inhibitory factor in individuals with acute spinal cord injury. Arch Phys Med Rehabil. 2015;96:633–44.
Papatheodorou A, Stein A, Bank M, Sison CP, Gibbs K, Davies P, et al. High-Mobility Group Box 1 (HMGB1) Is elevated systemically in persons with acute or chronic traumatic spinal cord injury. J Neurotrauma. 2017;34:746–54.
Center NSCIS. Facts and figures at a glance. Birmingham, AL: University of Alabama; 2018.
Siddall PJ, Middleton JW. A proposed algorithm for the management of pain following spinal cord injury. Spinal Cord 2006;44:67–77.
Segal JL, Gonzales E, Yousefi S, Jamshidipour L, Brunnemann SR. Circulating levels of IL-2R, ICAM-1, and IL-6 in spinal cord injuries. Arch Phys Med Rehabil. 1997;78:44–7.
Hayes KC, Hull TC, Delaney GA, Potter PJ, Sequeira KA, Campbell K, et al. Elevated serum titers of proinflammatory cytokines and CNS autoantibodies in patients with chronic spinal cord injury. J Neurotrauma. 2002;19:753–61.
Frost F, Roach MJ, Kushner I, Schreiber P. Inflammatory C-reactive protein and cytokine levels in asymptomatic people with chronic spinal cord injury. Arch Phys Med Rehabil. 2005;86:312–7.
Davies AL, Hayes KC, Dekaban GA. Clinical correlates of elevated serum concentrations of cytokines and autoantibodies in patients with spinal cord injury. Arch Phys Med Rehabil. 2007;88:1384–93.
Stein A, Panjwani A, Sison C, Rosen L, Chugh R, Metz C, et al. Pilot study: elevated circulating levels of the proinflammatory cytokine macrophage migration inhibitory factor in patients with chronic spinal cord injury. Arch Phys Med Rehabil. 2013;94:1498–507.
Herman P, Stein AB, Gibbs K, Korsunsky I, Gregersen P, Bloom O. Persons with chronic spinal cord injury have decreased NK cell and increased TLR/inflammatory gene expression. J Neurotrauma. 2018;35:1819–29.
Saltzman JW, Battaglino RA, Salles L, Jha P, Sudhakar S, Garshick E, et al. B-cell maturation antigen, a proliferation-inducing ligand, and B-cell activating factor are candidate mediators of spinal cord injury-induced autoimmunity. J Neurotrauma 2013;30:434–40.
Streijger F, So K, Manouchehri N, Gheorghe A, Okon EB, Chan RM, et al. A direct comparison between norepinephrine and phenylephrine for augmenting spinal cord perfusion in a porcine model of spinal cord injury. J Neurotrauma. 2018;35:1345–57.
Azevedo FA, Carvalho LR, Grinberg LT, Farfel JM, Ferretti RE, Leite RE, et al. Equal numbers of neuronal and nonneuronal cells make the human brain an isometrically scaled-up primate brain. J Comp Neurol. 2009;513:532–41.
Wanner IB. An in vitro trauma model to study rodent and human astrocyte reactivity. Methods Mol Biol. 2012;814:189–219.
Saghazadeh A, Rezaei N. The role of timing in the treatment of spinal cord injury. Biomed Pharmacother. 2017;92:128–39.
Liu MC, Akinyi L, Scharf D, Mo J, Larner SF, Muller U, et al. Ubiquitin C-terminal hydrolase-L1 as a biomarker for ischemic and traumatic brain injury in rats. The European journal of neuroscience. 2010;31:722–32.
Papa L, Lewis LM, Silvestri S, Falk JL, Giordano P, Brophy GM, et al. Serum levels of ubiquitin C-terminal hydrolase distinguish mild traumatic brain injury from trauma controls and are elevated in mild and moderate traumatic brain injury patients with intracranial lesions and neurosurgical intervention. The journal of trauma and acute care surgery. 2012;72:1335–44.
Papa L, Brophy GM, Welch RD, Lewis LM, Braga CF, Tan CN, et al. Time Course and Diagnostic Accuracy of Glial and Neuronal Blood Biomarkers GFAP and UCH-L1 in a Large Cohort of Trauma Patients With and Without Mild Traumatic Brain Injury. JAMA Neurol. 2016;73:551–60.
Agoston DV, Elsayed M. Serum-based protein biomarkers in blast-induced traumatic brain injury spectrum disorder. Frontiers in neurology. 2012;3:107.
Liu M, Zhang C, Liu W, Luo P, Zhang L, Wang Y, et al. A novel rat model of blast-induced traumatic brain injury simulating different damage degree: implications for morphological, neurological, and biomarker changes. Frontiers in cellular neuroscience. 2015;9:168.
Berger RP, Pierce MC, Wisniewski SR, Adelson PD, Clark RS, Ruppel RA, et al. Neuron-specific enolase and S100B in cerebrospinal fluid after severe traumatic brain injury in infants and children. Pediatrics. 2002;109:E31.
Pouw MH, Kwon BK, Verbeek MM, Vos PE, van Kampen A, Fisher CG, et al. Structural biomarkers in the cerebrospinal fluid within 24 h after a traumatic spinal cord injury: a descriptive analysis of 16 subjects. Spinal cord. 2014;52:428–33.
Cao F, Yang XF, Liu WG, Hu WW, Li G, Zheng XJ, et al. Elevation of neuron-specific enolase and S-100beta protein level in experimental acute spinal cord injury. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2008;15:541–4.
Loy DN, Sroufe AE, Pelt JL, Burke DA, Cao QL, Talbott JF, et al. Serum biomarkers for experimental acute spinal cord injury: rapid elevation of neuron-specific enolase and S-100beta. Neurosurgery. 2005;56:391–7. discussion -7
Ahadi R, Khodagholi F, Daneshi A, Vafaei A, Mafi AA, Jorjani M. Diagnostic Value of Serum Levels of GFAP, pNF-H, and NSE Compared With Clinical Findings in Severity Assessment of Human Traumatic Spinal Cord Injury. Spine. 2015;40:E823–30.
Svetlov SI, Prima V, Glushakova O, Svetlov A, Kirk DR, Gutierrez H, et al. Neuro-glial and systemic mechanisms of pathological responses in rat models of primary blast overpressure compared to "composite" blast. Frontiers in neurology. 2012;3:15.
Okonkwo DO, Yue JK, Puccio AM, Panczykowski DM, Inoue T, McMahon PJ, et al. GFAP-BDP as an acute diagnostic marker in traumatic brain injury: results from the prospective transforming research and clinical knowledge in traumatic brain injury study. J Neurotrauma. 2013;30:1490–7.
Yang Z, Bramlett HM, Moghieb A, Yu D, Wang P, Lin F, et al. Temporal Profile and Severity Correlation of a Panel of Rat Spinal Cord Injury Protein Biomarkers. Molecular neurobiology. 2018;55:2174–84.
Pelsers MM, Hanhoff T, Van der Voort D, Arts B, Peters M, Ponds R, et al. Brain- and heart-type fatty acid-binding proteins in the brain: tissue distribution and clinical utility. Clinical chemistry. 2004;50:1568–75.
Pike BR, Flint J, Dutta S, Johnson E, Wang KK, Hayes RL. Accumulation of non-erythroid alpha II-spectrin and calpain-cleaved alpha II-spectrin breakdown products in cerebrospinal fluid after traumatic brain injury in rats. Journal of neurochemistry. 2001;78:1297–306.
Mondello S, Robicsek SA, Gabrielli A, Brophy GM, Papa L, Tepas J, et al. alphaII-spectrin breakdown products (SBDPs): diagnosis and outcome in severe traumatic brain injury patients. J Neurotrauma. 2010;27:1203–13.
Brophy GM, Pineda JA, Papa L, Lewis SB, Valadka AB, Hannay HJ, et al. alphaII-Spectrin breakdown product cerebrospinal fluid exposure metrics suggest differences in cellular injury mechanisms after severe traumatic brain injury. J Neurotrauma. 2009;26:471–9.
Papa L, Robertson CS, Wang KK, Brophy GM, Hannay HJ, Heaton S, et al. Biomarkers improve clinical outcome predictors of mortality following non-penetrating severe traumatic brain injury. Neurocritical care. 2015;22:52–64.
Siman R, Giovannone N, Hanten G, Wilde EA, McCauley SR, Hunter JV, et al. Evidence That the Blood Biomarker SNTF Predicts Brain Imaging Changes and Persistent Cognitive Dysfunction in Mild TBI Patients. Frontiers in neurology. 2013;4:190.
Anderson KJ, Scheff SW, Miller KM, Roberts KN, Gilmer LK, Yang C, et al. The phosphorylated axonal form of the neurofilament subunit NF-H (pNF-H) as a blood biomarker of traumatic brain injury. J Neurotrauma. 2008;25:1079–85.
Al Nimer F, Thelin E, Nystrom H, Dring AM, Svenningsson A, Piehl F, et al. Comparative Assessment of the Prognostic Value of Biomarkers in Traumatic Brain Injury Reveals an Independent Role for Serum Levels of Neurofilament Light. PloS ONE. 2015;10:e0132177.
Shahim P, Gren M, Liman V, Andreasson U, Norgren N, Tegner Y, et al. Serum neurofilament light protein predicts clinical outcome in traumatic brain injury. Scientific reports. 2016;6:36791.
Rostami E, Davidsson J, Ng KC, Lu J, Gyorgy A, Walker J, et al. A Model for Mild Traumatic Brain Injury that Induces Limited Transient Memory Impairment and Increased Levels of Axon Related Serum Biomarkers. Frontiers in neurology. 2012;3:115.
Kumar RG, Diamond ML, Boles JA, Berger RP, Tisherman SA, Kochanek PM, et al. Acute CSF interleukin-6 trajectories after TBI: associations with neuroinflammation, polytrauma, and outcome. Brain, behavior, and immunity. 2015;45:253–62.
Woodcock T, Morganti-Kossmann MC. The role of markers of inflammation in traumatic brain injury. Frontiers in neurology. 2013;4:18.
Berger RP, Beers SR, Richichi R, Wiesman D, Adelson PD. Serum biomarker concentrations and outcome after pediatric traumatic brain injury. J Neurotrauma. 2007;24:1793–801.
Zhang Z, Zoltewicz JS, Mondello S, Newsom KJ, Yang Z, Yang B, et al. Human traumatic brain injury induces autoantibody response against glial fibrillary acidic protein and its breakdown products. PloS ONE. 2014;9:e92698.
Wang KK, Yang Z, Yue JK, Zhang Z, Winkler EA, Puccio AM, et al. Plasma Anti-Glial Fibrillary Acidic Protein Autoantibody Levels during the Acute and Chronic Phases of Traumatic Brain Injury: A Transforming Research and Clinical Knowledge in Traumatic Brain Injury Pilot Study. J Neurotrauma. 2016;33:1270–7.
Yang Z, Zhu T, Weissman AS, Jaalouk E, Rathore DS, Romo P, et al. Autoimmunity and Traumatic Brain Injury. Curr Phys Med Rehabil Rep. 2017;5:8.
Yang Z, Wang P, Morgan D, Lin D, Pan J, Lin F, et al. Temporal MRI characterization, neurobiochemical and neurobehavioral changes in a mouse repetitive concussive head injury model. Scientific reports. 2015;5:11178.
Rubenstein R, Chang B, Davies P, Wagner AK, Robertson CS, Wang KK. A novel, ultrasensitive assay for tau: potential for assessing traumatic brain injury in tissues and biofluids. Journal of neurotrauma. 2015;32:342–52.
Rubenstein R, Chang B, Yue JK, Chiu A, Winkler EA, Puccio AM, et al. Comparing Plasma Phospho Tau, Total Tau, and Phospho Tau-Total Tau Ratio as Acute and Chronic Traumatic Brain Injury Biomarkers. JAMA Neurol. 2017;74:1063–72.
Mondello S, Gabrielli A, Catani S, D'Ippolito M, Jeromin A, Ciaramella A, et al. Increased levels of serum MAP-2 at 6-months correlate with improved outcome in survivors of severe traumatic brain injury. Brain injury. 2012;26:1629–35.
Yang J, Korley FK, Dai M, Everett AD. Serum neurogranin measurement as a biomarker of acute traumatic brain injury. Clinical biochemistry. 2015;48:843–8.
Korley FK, Diaz-Arrastia R, Wu AH, Yue JK, Manley GT, Sair HI, et al. Circulating Brain-Derived Neurotrophic Factor Has Diagnostic and Prognostic Value in Traumatic Brain Injury. J Neurotrauma. 2016;33:215–25.
Funding
Funding for the STUDI (Spinal Trials Understanding, Design, and Implementsation) Group was provided by American Spinal Injury Association, (ASIA), Christopher & Dana Reeve Foundation, (CDRF), Craig H. Neilsen Foundation (CHN), International Foundation for Research in Paraplegia (IRP), International Spinal Research Trust (ISRT), Rick Hansen Institute (RHI), Spinal Cord Outcomes Partnership Endeavor (SCOPE), and Wings for Life (WFL).
Author information
Authors and Affiliations
Contributions
BKK was responsible for manuscript assembly and also contributed individually to the paper. All remaining authors (OB, IW, AC, JF, JS, KKW) contributed indivually to the paper. BKK is the Canada Research Chair in Spinal Cord Injury and holds the Dvorak Chair in Spine Trauma.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
This review article includes papers in which human volunteers were studied and assumes that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of the research.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kwon, B.K., Bloom, O., Wanner, IB. et al. Neurochemical biomarkers in spinal cord injury. Spinal Cord 57, 819–831 (2019). https://doi.org/10.1038/s41393-019-0319-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0319-8
This article is cited by
-
The Role of Tumor Necrosis Factor Following Spinal Cord Injury: A Systematic Review
Cellular and Molecular Neurobiology (2023)
-
Glial fibrillary acidic protein is a robust biomarker in cerebrospinal fluid and peripheral blood after traumatic spinal cord injury: a prospective pilot study
Acta Neurochirurgica (2023)
-
Traumatic brain injury biomarkers in pediatric patients: a systematic review
Neurosurgical Review (2022)
-
Therapy of spinal cord injury by zinc modified gold nanoclusters via immune-suppressing strategies
Journal of Nanobiotechnology (2021)
-
MicroRNA-139-5p Promotes Functional Recovery and Reduces Pain Hypersensitivity in Mice with Spinal Cord Injury by Targeting Mammalian Sterile 20-like Kinase 1
Neurochemical Research (2021)