Abstract
Study design:
Longitudinal cohort study.
Objectives:
To estimate socioeconomic and work outcomes over 2 and a half years following spinal cord injury (SCI), and to compare those in receipt of compensation (Accident Compensation Corporation, ACC) and those not.
Setting:
People admitted to the two spinal units in 2007–2009 in New Zealand, where there is a unique no-fault compensation scheme for injury.
Methods:
Interviews were conducted at ∼6, 18 and 30 months after SCI and data collected on pre-SCI and post-SCI health and socioeconomic characteristics. Poisson regression, quantile regression and a linear mixed model regression were used to compare differences in outcomes.
Results:
Of the 162 eligible people, 118 (73%) participated and 91(77%) were followed to 30 months; 79% received ACC. Median personal income, self-reported standard of living and household income adequacy all fell slightly to 18 months and then stabilized at 30 months. At that time, 49% had returned to paid work. Among those not eligible for ACC, income fell to less than half the ACC group (P<0.006 after adjustment), and return to work was lower (29% versus 54%).
Conclusion:
The findings that most people retained their economic status and that return to work was relatively high appear to be due to the proportion entitled to the ACC no-fault compensation scheme for injury; with earnings-related compensation, a focus on rehabilitation to work and non-means-tested support services. This situation should mitigate against the downward spiral into poverty and further ill-health.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI), caused by trauma or non-traumatic disease processes, often results in life-long neurological deficits. For most people, the inability to work, at least temporarily, means they are at risk of losing their livelihoods and becoming unable to support a family. In New Zealand, we have estimated the incidence of SCI as 30/million/year, but age-adjusted rates are higher among Māori (the indigenous population), 46/million, and especially Pacific people, 70/million.1
Loss of employment and income consequent to SCI can lead to a decline in socioeconomic status, the amplification of disadvantage, and inability to meet the extra costs associated with disability.2, 3, 4 One purpose of social security systems is to protect against financial difficulties in times of unemployment due to illness and injury.5 This can be done through compensation for lost wages or government social welfare schemes providing ‘safety net’ benefits.
In New Zealand, the majority of people who sustain a SCI are eligible for compensation through the Accident Compensation Corporation (ACC). Thus, at least as an ideal, they are eligible for ‘comprehensive entitlement, complete rehabilitation and real compensation’, carried out through ‘community responsibility’ and with ‘administrative efficiency’ in line with the original principles of the scheme.6 People who sustain any kind of traumatic SCI or a ‘treatment injury’ (i.e., an adverse result of medical treatment) are eligible for compensation through ACC. Such compensation is not contingent on fault, type or place of injury and can include weekly payments of up to 80% of pre-injury income (if in employment pre-injury) during rehabilitation and longer term if return to work is not possible. In addition, there are lump-sum payments for serious injury and extra assistance, which is not means tested, with support services, home and vehicle modifications and rehabilitation.
Though SCI is usually caused by trauma, a range of disease processes can also cause spinal cord damage, including tumours, infections, toxic and ischaemic causes.7 Those who develop a non-traumatic SCI may be eligible, depending on family circumstances, for a means-tested government sickness or invalids benefit that provides some financial support. In New Zealand, benefits however, are only ∼50% of the adult minimum wage. Though New Zealand’s spinal units provide a full range of health and rehabilitation services for all inpatients, the extent of longer-term rehabilitation, health services and support, financial assistance and return-to-work support, after discharge largely depends on people being eligible for ACC.
We have previously examined socioeconomic consequences of these two main types of income support by comparing people who sustained an injury (covered by ACC) with people who had a first stroke (potentially eligible for means-tested benefits).8 This showed that, 1 year post event, decline in standard of living, on several measures, was markedly worse in the stroke group than in the matched injury group. Furthermore, return to work was greater among the injury group. However, the two groups had different health problems and were measured over slightly different time periods.
As well as examining socioeconomic outcomes overall for people with SCI in New Zealand (the majority of whom receive ACC), we now have the opportunity to further investigate the potential disparity in financial and social supports in a group with the same health problem, followed over the same period, and with outcomes extended to 2 years. The aim is to estimate socioeconomic outcomes over 2 years following SCI among people admitted to the two spinal units, and to compare outcomes for those in receipt of ACC and those not.
Participants and methods
A longitudinal cohort study of people with a first diagnosis of SCI in New Zealand was undertaken. Details of this study have been described elsewhere1 but a brief overview is provided below.
Study population and recruitment
The study recruited people aged 16–64 years admitted to either of New Zealand’s two spinal units following acute impairment between July 2007 and August 2009. People were ineligible for the study if: the clinical team identified cognitive or communication problems precluding an interview; prognosis of death within 6 months; they were not New Zealand residents; or they had no neurological damage at the time of recruitment. Interviews were intended to occur 4 months after the SCI with eligible participants; second and third follow-up interviews were scheduled for 12 and 24 months after SCI.
Pre-SCI characteristics
Pre-SCI socio-demographic characteristics were collected at the first interview using questions from the 2006 Census.9 People were asked their personal income in the year before SCI. Self-reported material standard of living was asked on a five-point scale: high, fairly high, medium, fairly low and low (grouped as ‘high/fairly high’; ‘medium-low’). Whether their household income was adequate to meet everyday needs such as accommodation, food and clothing was asked using a four-point scale: More than enough, enough, just enough and not enough (grouped as ‘more than enough/enough’; ‘just enough/not enough’).10
Post-SCI health status
Nurses collected information on participants’ American Spinal Injury Association (AISA) Impairment Scale (AIS)11 at discharge from the unit (A=most severe to D=least severe).
Participants rated difficulty in five dimensions of the EQ-5D general health status measure (mobility, self-care, usual activities, pain/discomfort, anxiety/depression).12, 13 Responses were ‘no’; ‘some’; or ‘extreme’ problems (the last two grouped as ‘any problems’). We asked an additional question, in the EQ-5D format, about cognition.14, 15
Outcome measures
Economic
Questions about personal income, standard of living and household income adequacy were asked at the second and third interviews (as for pre-SCI).
Work
At each interview, participants were asked to describe their current work situation from a list: full-time work (⩾30 h per week); part-time work (<30 h per week); receiving a benefit; no benefit; student; homemaker; retired (the last four grouped as ‘other’).16 Return-to-work was defined as those in paid work (full- or part-time) pre-SCI, and who were back in paid work at the second or third interview.
Statistical analyses
Chi-squared tests were used to compare characteristics of participants who completed all three interviews and those who did not.
Comparison of demographic, pre-SCI variables, EQ-5D and AIS between the ACC and non-ACC groups used: Poisson regression where the outcome was binary, ordered logistic regression for ordered variables (for example, age group and AIS), and multinomial logistic regression for variables with more than two levels that were not ordered (for example, education and employment). Quantile regression was used to compare median incomes. Age and sex were adjusted for in all models.
Poisson regression with robust standard errors17 was used to compare the difference in the outcomes of work, standard of living and income adequacy at second and third interviews. Quantile regression was used to compare median incomes at second and third interviews. For measuring change over time, to account for the same people being measured at two different times (pre-SCI and at third interview—scheduled for 24 months post SCI), a linear mixed model regression was used.18 Age, sex and AIS were also adjusted for in these models.
Analysis was undertaken using Stata 12.19
Ethical approval
The study was approved by the New Zealand Health and Disability Multi-region Ethics Committee (MEC07/09/117).
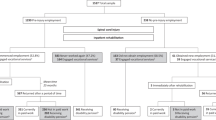
Results
Over 2 years, 186 people aged 16–64 years were admitted to the two spinal units of whom 24 were ineligible. Of the 162 eligible people, 118 participated (73% response rate); 15 declined and 29 were non-contactable. We have previously reported that participants were less likely to be of Māori and Pacific ethnicity than non-participants.1 The mean time from date of SCI to first interview was 6.5 months (median 6.4; inter-quartile range (IQR) 4.8–7.6 months). Of the 118 participants completing the first interview, 103 (87%) were followed-up to the second interview (mean 16.6 months; median 16.5; IQR 15.0–17.6 months—hereafter referred to as 18-month interview), and 91 (77%) to the third interview (mean 31.5 months; median 30.2; IQR 29.2–32.8 months—referred to as 30-month interview). Of the 27 who did not complete all three interviews, 2 people died, 4 declined, 1 left the country, 4 could not be contacted and for 16 people the reason was unclear. A significantly greater proportion of those with more severe AIS (P=0.03) and those of Māori, Pacific or Asian ethnicity did not complete all three interviews (P=0.01) (Table 1). No other statistically significant differences were observed.
Two groups—those who received ACC compensation, and those who did not, were identified. The ACC group (n=93) included all those with injury as the SCI cause and were covered by ACC at the first interview or by the time of the 18-month interview (n=89), those who were unsure of the cause of their injury but received cover from ACC (n=2), and those with a non-traumatic SCI but covered by ACC (n=2). Although covered by ACC, 24 (26%) did not receive earnings-related compensation, mostly because they were not employed at the time of their SCI (n=16). Four people did not receive earnings-related compensation but received a lump-sum payment.
The non-ACC group (n=25) included all those with non-traumatic cause not covered by ACC at the first interview or by the 18-month interview (n=23), and those with injury as the cause but not covered by ACC (n=2) (for example, resident outside New Zealand at the time of injury).
Receipt of private income protection insurance was reported by eight people in the ACC group and two people in the non-ACC group.
Pre-SCI characteristics
Of the total study population, three-quarters were men, 67% were of European ethnicity, 55% were married or living with a partner and 83% were in paid employment (Table 2). A greater proportion of the non-ACC group were older (difference statistically significant after adjusting for sex; P=0.006). The non-ACC group also had a greater proportion of women, Pacific and Asian people (differences not statistically significant after adjustment; P=0.08 and P=0.14, respectively). No other appreciable differences were observed for other pre-SCI variables.
Post-SCI health characteristics
A greater proportion of the non-ACC group (64%) had AIS=‘D’ compared with the ACC group (50%), although the difference was not statistically significant after adjusting for age and sex (P=0.13) (Table 2). The two groups were very similar at the first interview for each of the EQ-5D health status variables (Figure 1). After 18 months, a greater proportion of the non-ACC group reported problems with usual activities, anxiety/depression and pain/discomfort (P=0.04); only the latter was statistically significant after adjusting for age and sex. After 30 months, the groups were similar in all but cognitive status, with a greater proportion of the non-ACC group reporting problems (53%) compared with the ACC group (24%) (P=0.02).
Outcomes
Economic outcomes
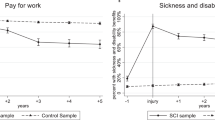
The proportion of the total study population reporting a ‘medium-low’ standard of living increased slightly from 47% pre-SCI to 56% at 18 months and 50% at 30 months. The proportion reporting ‘just/not enough’ income increased more, from 28% pre-SCI to 44% at 18 months and 40% at 30 months. The decline in both standard of living and income adequacy was greater for the non-ACC group, and was greatest at 18 months; the difference narrowing at 30 months for standard of living (Figure 2).
After adjusting for age, sex and AIS, risk of reporting ‘medium-low’ standard of living at 18 months for the non-ACC group was statistically significantly higher than the ACC group (adjusted relative risk (ARR)=1.16; 95% confidence interval (95%CI)=1.01–1.35) and for ‘just/not enough’ income (ARR=1.18; 95%CI=1.00–1.40) (Table 3). This was similar at 30 months after SCI, but statistically significant only for ‘just/not enough’ income (ARR=1.22; 95%CI=1.02–1.46; Table 3). After adjusting for ethnicity, the 18-month risk for ‘medium-low’ standard of living (ARR=1.13; 95%CI=0.98–1.29) and ‘just/not enough’ income (ARR=1.14; 95%CI=0.96–1.35) changed only slightly.
The median personal income for the total study population declined from NZ$40 000 pre-SCI to $38 760 at 18 months; increasing to $41 176 at 30 months. For the non-ACC group, median income declined by 45% over 30 months (from $36 500 to $19 938) compared with a 15% increase in the ACC group (from $40 000 to $45 900) (Figure 3). The difference at 30 months in median income between the ACC and non-ACC groups after adjustment for age, sex and AIS was statistically significant (P=0.006). The difference between the groups in change over time from pre-SCI to 30 months did not reach statistical significance (P=0.55). Among Māori and Pacific, income was lower at baseline ($31 902 compared with $42 000 for other ethnicities) but did not decrease over the 30 months.
Sub-analyses of standard of living, income adequacy and median personal income, undertaken of 91 participants completing all three interviews, showed the same pattern over the three interview times and the statistical significance between the groups did not change from analyses undertaken with participants who completed 6-month (n=118), 18-month (n=103) and 30-month (n=91) interviews (data not shown).
Work outcomes
Of the 103 participants who completed the 18-month interview, 84 were in paid work pre-SCI; 35 (42%) had returned to work by 18 months. Of the ACC group, 42% had returned to work compared with 39% of the non-ACC group. While the relative risk (adjusted for age, sex and AIS) of returning to work was less for the non-ACC group, this was not statistically significant (ARR=0.88; 95%CI=0.45–1.70).
Of the 91 participants who completed the 30-month interview, 75 people were in paid work pre-SCI and 37 (49%) had returned to work. Fifty-four per cent of the ACC group had returned to work compared with 29% of the non-ACC group. The adjusted likelihood of return to work was 43% less for the non-ACC group compared with the ACC group, but this was not statistically significant (ARR=0.57; 95%CI=0.27–1.19). When return-to-work at 30 months was also adjusted for cognitive status at 30 months, the ARR barely changed (ARR=0.58; 95%CI=0.27–1.24).
For Māori and Pacific, 82% were employed before SCI, similar to other ethnicities (84%) but the proportions returning to work at 18 months and 30 months were lower than for other ethnicities: 32% versus 45% and 44% versus 53%, respectively.
Discussion
Among a cohort of people admitted to the two spinal units in New Zealand and followed for 30 months, personal income, reported standard of living and household income adequacy all decreased slightly to 18 months and then stabilized. The effect was similar for Māori and Pacific people, though their pre-SCI standard of living was lower. By 18 months, 42% of people who were employed before SCI had returned to paid work; 49% by 30 months. Among Māori and Pacific people, of whom a similar proportion (versus other ethnicities) were employed before SCI, the proportions who returned to work were lower. Among those who received compensation through ACC, median personal income remained similar to 30 months, whereas among those not eligible for ACC, personal income fell to 18 months and then decreased more steeply to 30 months so that their median income was less than half that of the ACC group. At 18 and 30 months, the ARR of reporting ‘just/not enough’ household income was ∼20% higher in the non-ACC group compared with the ACC group. The difference was less for the measure of standard of living at 30 months. Return to work was higher among those who received ACC, after adjustment for functional impairment at 30 months, but numbers were small and the difference was not statistically significant.
There have been many studies of return to work among people with SCI, though few studies have specifically examined standard of living after SCI, irrespective of work. Levi et al.20 compared a prevalent sample of SCI survivors with a population sample in Sweden, and found that people with SCI had similar access to material resources but had fewer financial reserves. Most people (71%) received a sick pension, which is obviously set at a level that avoids severe hardship. Several reviews of return to work outcomes have been published in the last 10 years.21, 22, 23, 24 Return to work varies widely, from 21 to 67%,22 with employment rates increasing with time since SCI. Rates are higher in Europe and Australia than in North America.24 Predictors of return to work in the United States include: younger age at injury, higher levels of education and white versus minority ethnicity.21, 22 Less severe SCI and higher functional independence are predictors of return to work among those with low levels of education, but no longer predict return to work among those with the highest level of education.25 In the United States, among those who do return to work, women, African Americans and those with less than a college degree earn less, thus compounding the disparities in return to work.25 Studies of income have been restricted to earnings and have not included income from other sources.25, 26, 27 Studies that have examined the effect of compensation or benefits on return to work suggest a negative relationship,27, 28, 29 maybe because of fear of losing financial or medical benefits.21
In contrast, our investigation has examined changes in personal income from all sources and changes in income adequacy, which takes into account differences in household composition. Income matters: as well as meeting basic needs, it enables people to take part in valued activities and pay for the extra costs of disablement. Moreover, household income is a significant predictor of mortality among people with SCI, over and above age, sex, ethnicity and severity of injury.30 Loss of income and lack of access to universal health care also increases the risk of bankruptcy for medical debt following SCI.31
Overall, because of earnings-related compensation through ACC for most people and universal health-care coverage, people who sustain a SCI in New Zealand do not suffer a substantial loss of income and, importantly, disparities between ethnic groups are not compounded. The comparison of the ACC and non-ACC groups demonstrated that earnings-related compensation was the determining factor in preventing a drop in income. It also suggested that ACC cover did not deter return to work, and might even encourage return to work. Though the numbers were small, we could rule out anything above a 19% higher return to work in the non-ACC group compared with the ACC group at 30 months (ARR=0.57, 95%CI 0.27–1.19).
Our previous comparison of socioeconomic circumstances following injury or stroke demonstrated the same pattern: the injured group, who were mainly covered by ACC, maintained significantly higher incomes at 12 months and returned to work significantly earlier than the matched sample of people with stroke.8 The present comparison extends these findings to 30 months, following groups with the same condition, and over the same time period. We have previously proposed that the reasons compensation through ACC did not deter early return to work are: first its true no-fault nature with only minimal involvement of the legal system, and second its deliberate focus on rehabilitation to work.8
The strengths of this study are that it is population-based, has a prospective design and a relatively high response rate, and takes advantage of a natural experiment in New Zealand. A limitation is that the participant population and those who provided data for the full 30 months under-represented Māori and Pacific people and those with a more severe SCI (follow-up only). Nevertheless, an analysis restricted to those who provided data for 30 months demonstrated the same patterns. The under-representation of Māori and Pacific should be borne in mind in generalizing to the total population. When comparing to other populations, the somewhat lower proportion of people with the most severe SCI should also be borne in mind.32 Additionally, though the ACC and non-ACC groups were similar on AIS scores and health status measures 6 months post SCI, they diverged at 30 months, especially for cognition. Our primary interest was in socioeconomic outcomes between the two groups irrespective of functional impairment differences, but such differences are important for interpreting return to work. For the analyses comparing return to work, we adjusted for age, sex and AIS score. Additional adjustment for cognition did not materially affect the results. In the comparison of income between ACC and non-ACC groups, we were surprised that the difference in changes over time was not statistically significant (despite a highly significant difference in the incomes at 30 months); most likely due to small sample size and difference in income distribution between groups. Finally, because of small numbers, we were unable to investigate socioeconomic outcomes by ethnicity within the ACC and non-ACC groups.
Conclusion
In New Zealand, most people followed over 2 and a half years after sustaining a SCI retained their income and standard of living. Rates of return to work were high overall (49%). The reason for both these findings appears to be the no-fault compensation scheme for injury available to the majority of participants. This situation should mitigate against a downward spiral into poverty and further ill-health (a likely consequence of not receiving compensation). If such economic outcomes are also accompanied by re-integration into society and regaining of quality of life, then such a no-fault compensation scheme should be seen as a model for rehabilitation after SCI—traumatic and non-traumatic.
Data archiving
There were no data to deposit.
References
Derrett S, Beaver C, Sullivan MJ, Herbison GP, Acland R, Paul C . Traumatic and non-traumatic spinal cord impairment in New Zealand: incidence and characteristics of people admitted to spinal units. Injury Prev 2012; 18: 343–346.
Riphahn RT . Income and employment effects of health shocks. A test case for the German welfare state. J Popul Econ 1999; 12: 363–389.
Reville RT, Schoeni RF . Disability From Injuries at Work: The Effects on Earnings and Employment. RAND Corporation Publications Department. 2001.
Jenkins SP, Rigg JA . Disability and disadvantage: selection, onset and duration effects. J Soc Pol 2004; 33: 479–501.
Burchardt T . Employment retention and The Onset of Sickness or Disability: Evidence from Labour Force Sickness Longitudinal Datasets. London School of Economics, Centre for Analysis of Social Exclusion: London. 2003.
Royal Commission of Inquiry. Compensation for Personal Injury in New Zealand. New Zealand Government Printer: Wellington. 1967.
McDonald JW, Sadowsky C . Spinal-cord injury. Lancet 2002; 359: 417–425.
McAllister S, Derrett S, Audas R, Herbison P, Paul C . Do different types of financial support after illness or injury affect socio-economic outcomes? A natural experiment in New Zealand. Soc Sci Med 2013; 85: 93–102.
Statistics New Zealand. New Zealand Census of Population and Dwelling 2006 Available from: http://www.stats.census.govt.nz.
Statistics New Zealand. Household Economic Survey 2009-10 printable questionnaires 2009 (Accessed on 12 October 2011) Available from: http://www.stats.govt.nz/browse_for_stats/people_and_communities/Households/hes-flowcharts-2009-10.aspx.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M et al. Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med 2011; 34: 547–554.
The EuroQol Group. EuroQol - a new facility for the measurement of health-related quality of life. Health Policy 1990; 16: 199–208.
Brooks R . EuroQol: the current state of play. Health Policy 1996; 37: 53–72.
Krabbe PFM, Stouthard MEA, Essink-Bot M-L, Bonsel GJ . The effect of adding a cognitive dimension to the EuroQol multi-attribute health-status classification system. J Clin Epidemiol 1999; 52: 293–301.
Langley J, Derrett S, Davie G, Ameratunga S, Wyeth E . A cohort study of short-term functional outcomes following injury: the role of pre-injury socio-demographic and health characteristics, injury and injury-related healthcare. Health Qual Life Out 2011; 9: 68.
Survey of Working-Aged People in 2000 Available from http://www.msd.govt.nz/about-msd-and-our-work/publications-resources/monitoring/living-standards/living-standards-elsi.html.
Zou G . A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159: 702–706.
McCulloch CE, Neuhaus JM . Generalized Linear Mixed Models. Encyclopedia of Biostatistics. John Wiley & Sons, Ltd;. 2005.
StataCorp. Stata Statistical Software: Release 12. StataCorp LP: College Station, TX. 2011.
Levi R, Hultling C, Seiger Å . The Stockholm spinal cord injury study: 4. Psychosocial and financial issues of the Swedish annual level-of-living survey in SCI subjects and controls. Spinal Cord 1996; 34: 152–157.
Ottomanelli L, Lind L . Review of critical factors related to employment after spinal cord injury: implications for research and vocational services. J Spinal Cord Med 2009; 32: 503–531.
Lidal IB, Huynh TK, Biering-Sørensen F . Return to work following spinal cord injury: a review. Disabil Rehabil 2007; 29: 1341–1375.
Anderson D, Dumont S, Azzaria L, Le Bourdais M, Noreau L . Determinants of return to work among spinal cord injury patients: a literature review. J Vocat Rehab 2007; 27: 57–68.
Young AE, Murphy GC . Employment status after spinal cord injury (1992-2005): a review with implications for interpretation, evaluation, further research, and clinical practice. Int J Rehabil Res 2009; 32: 1–11.
Krause JS, Terza JV . Injury and demographic factors predictive of disparities in earnings after spinal cord injury. Arch Phys Med Rehabil 2006; 87: 1318–1326.
Krause JS, Terza JV, Dismuke C . Earnings among people with spinal cord injury. Arch Phys Med Rehabil 2008; 89: 1474–1481.
Ramakrishnan K, Loh SY, Omar Z . Earnings among people with spinal cord injury. Spinal Cord 2011; 49: 986–989.
Engel S, Murphy GS, Athanasou JA, Hickey L . Employment outcomes following spinal cord injury. Int J Rehabil Res 1998; 21: 223–229.
Bell SM . The effects of government disability benefits, accessibility laws and rehabilitation on employment choices by individuals. Florida International University: Miami. 2002.
Krause JS, Saunders LL, DeVivo MJ . Income and risk of mortality after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 339–345.
Relyea-Chew A, Hollingworth W, Chan L, Comstock BA, Overstreet KA, Jarvik JG . Personal bankruptcy after traumatic brain or spinal cord injury: the role of medical debt. Arch Phys Med Rehabil 2009; 90: 413–419.
Wyndaele M, Wyndaele J-J . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Acknowledgements
We are grateful to all those who participated in this study. We thank the management team at the Burwood Academy of Independant Living and the two spinal units—Christchurch and Auckland and Dr Rick Acland for helpful comments on an earlier draft of this paper. The study was funded by the Health Research Council of New Zealand. The views and conclusions expressed herein are the authors’ and may not reflect those of the funders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of intereset.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Paul, C., Derrett, S., McAllister, S. et al. Socioeconomic outcomes following spinal cord injury and the role of no-fault compensation: longitudinal study. Spinal Cord 51, 919–925 (2013). https://doi.org/10.1038/sc.2013.110
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.110
Keywords
This article is cited by
-
United and flexible: a collaborative approach to early vocational rehabilitation on a spinal unit. A realist study
Spinal Cord Series and Cases (2023)
-
Life satisfaction 18 months and 10 years following spinal cord injury: results from a New Zealand prospective cohort study
Quality of Life Research (2023)
-
Comparative neuroanatomy of the lumbosacral spinal cord of the rat, cat, pig, monkey, and human
Scientific Reports (2021)
-
The Association Between Fault Attribution and Work Participation After Road Traffic Injury: A Registry-Based Observational Study
Journal of Occupational Rehabilitation (2020)
-
The impact of musculoskeletal injuries sustained in road traffic crashes on work-related outcomes: a protocol for a systematic review
Systematic Reviews (2018)