Abstract
Study design
A register based cohort study.
Objectives
To investigate labour market participation following spinal cord injury (SCI) and to describe the impact of personal and SCI characteristics.
Setting
Norway.
Methods
Persons registered with SCI in the Norwegian SCI registry 2011–2017, and matched reference individuals without SCI from the general population (named controls) were followed for up to six years after injury using national registry data on employment, education, income, and social security benefits. Main measures of labour market participation were: (1) Receiving any amount of pay for work, and (2) Receiving sickness and disability benefits.
Results
Among the 451 persons with SCI (aged 16–66 years and working before injury), the estimated percentages receiving pay for work and sickness and disability benefits in the sixth years after injury were 63% (95% CI 57–69) and 67% (95% CI 61–72).
Corresponding percentages for the controls (n = 1791) were 91% (95% CI 90–93) for receiving pay for work and 13% (95% CI 12–15) for receiving sickness and disability benefits. Among persons with SCI, less severe neurological outcome, higher level of education, younger age at injury, and a stronger pre-injury attachment to employment (higher employment income, having an employer, less receipt of benefits), were associated with higher labour market participation.
Conclusion
SCI substantially decreased labour market participation up to six years after injury compared to matched controls. Even if a relatively large proportion of persons with SCI remained in some degree of work activity, more than half did so in combination with receiving benefits.
Similar content being viewed by others
Introduction
Employment is a key rehabilitation outcome for people with spinal cord injury (SCI), and it tends to be positively associated with adjustment to SCI, life satisfaction, a sense of purpose, mental stimulation, social contact and well-being [1]. The level of employment among people with SCI is positively influenced by a number of factors, such as personal factors (younger age at time of injury, higher level of education, higher motivation), SCI-related characteristics (less severe neurological outcome) and employment-related factors (support from the employer, possibility to continue working in the same organisation) [2,3,4,5,6].
Most people with SCI can potentially be in employment if they get access to appropriate work accommodations [1]. However, the average employment rate among 9875 persons with SCI in 22 countries across the world was 38% (ranging from 10% to 61%), which was considerably lower than in the respective general working populations [7]. Contextual country-level factors, such as labour market systems and policies with respect to social security, vocational rehabilitation and employment, may explain some of the differences in employment levels across countries [8].
Norway has a well-developed welfare and health care system with universal rights to health and welfare provisions, a strong policy emphasis on high employment, and high expenditure on return to employment measures after sickness or injury. Compared with other European countries, a large portion of the Norwegian population is on sickness and disability benefits [9]; 17% in the 18–66 age group [10]. Still, in the last quartile of 2021, 72.3% of the population aged 15–74 was part of the workforce [11]. The proportion employed following SCI in Norway have been reported to range from 35% to 52% in different studies [4, 5, 7, 12], which shows that there is considerable employment gap between persons with SCI and the general population.
To gain further knowledge regarding labour market participation in the SCI population, there is a need for longitudinal studies with information on both employment and sickness and disability benefits, to achieve a more complete picture [13]. Norway is an ideal place to perform such studies due to its national SCI registry which can be linked to several population-based databases [14].
The overall objective was to investigate labour market participation up to six years following SCI. The specific aims were: (1) to describe labour market participation post-SCI for persons receiving pay for work (>0 Norwegian Kroner (NOK)/Euro (EUR)) the year before SCI; (2) to compare labour market participation following SCI with a matched group from the general population; (3) to describe the impact of personal and SCI characteristics on labour market participation after SCI.
Methods
Study design
Cohort study following persons with SCI from the Norwegian SCI registry (NorSCIR), and a matched reference group without SCI taken from the general Norwegian population (named “controls”), for one year before injury and up to six years after injury, using national registry data on employment, education, income, and social security benefits.
NorSCIR is a national medical quality registry for SCI care. All patients with traumatic or non-traumatic SCI admitted for first rehabilitation to one of the three Norwegian specialized SCI departments and who give their consent are included in the registry. Annual reviews show that this registry covers > 90% of the incidence population [15].
Ethical approval was obtained from the Regional Committee for Medical and Health Research Ethics in Central Norway (2018/294/REK-midt). Registration in the NorSCIR is voluntary with a written informed consent before registration occurs. Persons giving consent to participate in NorSCIR accept that their information can be used for research purposes, including linkage with a range of national registers.
Study samples
Included in the SCI sample were all persons who experienced traumatic or non-traumatic SCI, were admitted to one of the three SCI units in Norway and registered in the NorSCIR from 01.01.2011 to 31.12.2017, were in working age (16 to 66 years) at time of injury, living in Norway in the month before injury, and “eligible” for work by receiving any pay for work (>0 NOK/EUR) in the year before SCI. We used 66 years of age as the upper limit because the legal retirement age is 67 years in Norway. The lower limit of 16 years was chosen as this is the last year of compulsory education.
Matched reference individuals from the general population (matching the SCI sample for year of birth, sex, county of residence, and level of education) were randomly drawn from population registries by Statistics Norway. Participants in this sample are in this study named “controls”. Five controls were drawn for each patient. Only controls living in Norway and employed, according to the same definition as for the SCI sample, were included in the analyses.
Data sources
NorSCIR [16] provided information on personal and injury characteristics: Age at injury, sex, date of acute hospital admission, neurological classification and cause of injury.
Statistics Norway (SSB) [17, 18] provided data on income from work, registration status (dates of death and emigration), highest attained educational level, ongoing education, year of birth, county of residence, and sex (controls).
The Norwegian Labour and welfare administration (NAV) [19, 20] provided information on dates of sickness absence benefit, work assessment allowance, disability pension, old age pension, and employment status.
The Norwegian social security system
All persons who are either residents or working as employees in Norway are insured under the National Insurance Scheme, managed by NAV [19]. Employed people can be granted sick leave compensation covering up to 100% of income for a period of maximum 52 weeks if they are unable to work due to an illness or injury. After 52 weeks, employees with a reduction in work ability of at least 50% due to illness or injury may apply for long-term benefits (work assessment allowance (AAP) or disability pension (DP)) to compensate for loss of income. While AAP is a temporary benefit (max 3 years) requiring active treatment and/or rehabilitation measures, DP is granted on a permanent basis to those whose earning capacity is permanently reduced. The total allowance from AAP and DP is approximately 66% of the income from the three best payed of the last five years before disability and up to maximum six times the National insurance basic amount (G) for each year (1G = 106 399 Norwegian kroners, approximately 11 033 euro (as of 21.3.2022)).
Linkage
The SCI and control sample were linked to the various registry data by an identification key created by Statistics Norway using the unique 11-digit personal identity number given to all Norwegian citizens.
Follow-up period
The start of the follow-up period was 12 months before the date of injury. The date of injury was set to the date of acute hospital admission registered in NorSCIR for the SCI sample, and controls were assigned the same date as their respective matched persons with SCI. Participants were censored at the date/month of emigration, death, 67 years’ birthday, last available data (31.12.2020) or month 72 after injury, whichever came first. The choice of ending follow-up at 72 months/6 years post-SCI was made since less than half of the cohort (only those injured 2011-2013) could be followed past this point. The total follow-up period was divided into a maximum of seven 1-year time intervals (−1 (year before injury), 0–1, 1–2, 2–3, 3–4, 4–5, 5–6 (years after injury)).
Measures of labour market participation post-spinal cord injury
Main measures of labour market participation were: (1) Receiving any amount of pay for work (>0 NOK/EUR), and (2) Receiving sickness and disability benefits, which included sickness absence benefit, work assessment allowance and/or disability pension, to compensate for loss of income. Additional outcomes included: (1) Mean employment income as a continuous variable and (2) Each of the sickness/disability benefits separately (Table 1).
Study variables
Study variables available for the SCI sample (from NorSCIR) included sex, age at injury (16–29, 30–39, 40–49, 50–59, 60–66 years), date of acute hospital admission for SCI (2011–2014, 2015–2017), cause of injury (traumatic, non-traumatic), and neurological status.Categorisation of neurological status was done using the International Standards for Neurological Classification of SCI [21], including neurological level of injury and American Spinal Injury Association Impairment Scale (AIS) grade, to create four SCI impairments groups (level and AIS): Tetraplegia (C1-C8) AIS A, B or C; Tetraplegia (C1-C8) AIS D, Paraplegia (T1-S5) AIS A, B or C; Paraplegia (T1-S5) AIS D, E. In cases of missing neurological status at discharge, this was replaced with the classification at admission. Those with AIS E at discharge had neurological level at T1 or lower prior to the last examination and were categorized into group Paraplegia AIS D, E.
Baseline variables for both the SCI and control samples were assessed during one year before injury (from SSB and NAV) and included highest educational level (primary, secondary, higher education), ongoing education, employment income (NOK 0–299.999, 300.000–499.999, 500.000–999.999, and ≥1.000.000), employment status (having a registered employer for at least 1 month in the year before injury or not) and receipt of sickness or disability benefits (receiving benefits in at least one month in the year before injury or not).
Statistical analysis
Characteristics of the patient and control samples were presented with descriptive statistics.
We explored the association between time during follow-up and labour market participation using general estimation equations’ (GEE) logistic regression analyses. Analyses included time as year in relation to injury (each year as a category, from year before to sixth years after) and repeated measures of the two dichotomous labour market participation outcomes (pay for work and sickness/disability benefits, assessed each year of follow-up for each participant). We performed separate analyses for the SCI and control samples, with adjustment for age, sex, and educational level. Estimates from the analyses were used to calculate and graphically present the level (percentage) of labour market participation at each 1-year interval during follow-up.
For the SCI sample, we used a similar approach to assess labour market participation over time for subgroups of age, sex, level of education, SCI impairment, and cause of injury. A separate GEE analysis was performed for each grouping variable by including it in the GEE model and adding an interaction term with the time variable. All analyses were adjusted for age, sex, and level of education.
For persons with SCI, we further explored the impact of various personal and SCI characteristics on labour market participation after injury using three different models (GEE logistic regression, with six repeated outcome assessments; from injury to six years after). Model A included adjustment for time, age group, sex, and level of education, Model B included additional adjustment for injury variables (SCI impairment group, cause of injury, year of injury), and Model C further added adjustment for pre-injury employment (employment income, employment status and medical benefits before injury).
We compared labour market participation between persons with SCI and controls within matched groups using fixed-effect logistic regression models. This analysis compares persons with SCI only with their designated controls, automatically adjusting for year of birth, sex, county of residence, and level of education (matching variables), and also accounting for the unequal number of controls per patient in the total samples. Estimates from the analyses were used to calculate the absolute and relative difference (prevalence difference in %-points and odds ratio with 95%CI) between the SCI and control sample for labour market participation at one year before injury, 1–3 years after injury and 4–6 years after injury.
Supplementary analyses included alternative outcome measures for labour market participation (assessed each year of follow-up for each participant); (1) Mean employment income as a continuous variable (SCI and control samples) and (2) each of the sickness/disability benefits separately; sickness absence benefit, AAP and DP (SCI sample only). The association between time (year in relation to injury) and each outcome was analysed using GEE linear or logistic regression, with an adjustment for age, sex and education.
Stata® version 16.0 (StataCorp, College Station, Texas, USA) was used for all statistical analyses.
Results
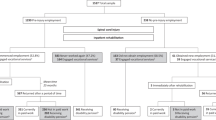
Of the 751 persons registered in the NorSCIR from 01.01.2011 to 31.12.2017, 300 persons were excluded (aged ≥ 67 (N = 179), pay for work = 0 (N = 113, of which 75 were on full-time medical benefits), not living in Norway (N = 8)). Thus, 451 participants with SCI were included in the SCI sample.
After excluding controls aged ≥ 67, not living in Norway, and with pay for work = 0 (same criteria as for the SCI sample), 1791 persons matched to 443 persons with SCI remained in the control sample. In the SCI sample, 8 persons had no controls, 12 persons had one control, 33 persons had two controls, 68 persons had three controls, 141 persons had four controls and 189 persons had five controls.
The SCI and control samples were quite similar regarding age, sex, and education (Table 2). Controls had a slightly higher annual employment income and received less sickness and disability benefits during the year before SCI compared with the persons with SCI.
The median follow-up time for the SCI sample was 57 months.
The median follow-up time for the patient sample was 57 months (lower quartile 38, and upper quartile 72), and 58 months for the controls (lower quartile 42, and upper quartile 72) (data not presented). The number (and %) of participants receiving pay for work and/or sickness and disability benefits each year of follow-up is provided for both samples in supplemental Table 1.
The estimated percentage receiving pay for work in the SCI sample gradually decreased from 100% before injury to 63% (95% CI 57–69) six years after injury, while decline in the control sample was from 100% to 91% (95% CI 90–93) (Fig. 1A). The estimated percentage receiving sickness and disability benefits in the SCI sample was 18% before injury (95% CI 14-21), peaked to 87% during the first year after injury and then decreased to 67% (95% CI 61–72) six years after injury (Fig. 1B). In the control sample it rose from 8% before “injury” to 13% (95% CI 12–15) six years later.
Results of the general estimation equations’ (GEE) logistic regression models with “Receiving any amount of pay for work” (A, left side) and “Receiving sickness and disability benefits” (B, right side) as dependent variables. All models included adjustment for age, sex and educational level. Estimates from the analyses were used to calculate and graphically present the estimated percent receiving pay for work, and receiving sickness and disability benefits, with 95% confidence intervals. The vertical line at injury indicates the time of spinal cord injury. The results are shown for the SCI sample and control sample at each 1-year interval during follow-up.
The development of labour market participation over time for the SCI sample across subgroups (age, sex, educational level, and injury characteristics) is shown in Figs. 2B–F and 3B–F.
Results of the general estimation equations’ (GEE) logistic regression models with “Receiving any amount of pay for work” as dependent variable. All models included adjustment for age, sex and educational level. Estimates from the analyses were used to calculate and graphically present the estimated percent receiving pay for work with 95% confidence intervals. The vertical line at injury indicates the time of spinal cord injury. AIS American Spinal Injury Association Impairment Scale. Primary, secondary and higher refer to the level of education. Traumatic refers traumatic spinal cord injury. Non-traumatic refers to non-traumatic spinal cord injury.
Results of the general estimation equations’ (GEE) logistic regression models with “Receiving sickness and disability benefits” as dependent variable. All models included adjustment for age, sex and educational level. Estimates from the analyses were used to calculate and graphically present the estimated percent receiving pay for work with 95% confidence intervals. The vertical line at injury indicates the time of spinal cord injury. AIS American Spinal Injury Association Impairment Scale. Primary, secondary and higher refer to the level of education. Traumatic refers traumatic spinal cord injury. Non-traumatic refers to non-traumatic spinal cord injury.
For the SCI sample, there was a gradual shift from short-term to long-term benefits during follow-up, with over half of persons with SCI on disability pension (DP) at end of follow-up (Supplementary Fig. 1).
Among those receiving pay for work 4–6 years after SCI, 55–57 % also received sickness and disability benefits (Supplementary Table 1).
Comparison between the persons with SCI and their controls (within matched groups) showed that persons with SCI had 28%-point lower annual percentage of receiving pay for work 4–6 years after SCI, and a corresponding 36%-point higher annual percentage of receiving sickness and disability benefits (Table 3).
Persons with SCI with higher age at injury (age 60+), primary level of education and more severe neurological outcome (tetraplegia AIS A-C) had lower odds of labour market participation (Table 4). Compared with persons with less impairment (Paraplegia AIS D-E), persons with more severe impairment (Tetraplegia AIS A-C) had 70 % lower odds for receiving pay for work (OR 0.30, 95% CI 0.17–0.54, Model C), and about 20 times higher odds of receiving sickness and disability benefits (OR 19.6 95% CI 9.04–42.53 Model C).
Differences in pre-injury employment (employment income, employment status and receipt of benefits) had a major influence on outcomes of labour participation after injury (Table 4).
The predicted probabilities for labour participation are shown in supplementary Table 2.
Results of the supplementary analysis are shown in Supplementary Fig. 1, Supplementary Fig. 2 and Supplementary Table 3.
Discussion
Level of labour market participation post-spinal cord injury
4-6 Years after injury, the percentage receiving pay for work among persons with SCI was 28%-points lower and the percentage receiving sickness and disability benefits 36%-point higher, compared with their matched controls from the general population. Thus, as expected, this study confirms the common notion and earlier studies showing that a SCI injury reduced labour market participation [2].
Our finding that 63% received pay for work six years post-injury is higher than the level reported from most other studies from Norway (35% to 52%, [4, 5, 7, 12]) and internationally (10% to 61% [7]). However, these studies have used different definitions of work activity, preventing a direct comparison, a problem that has been reported in literature reviews [2, 13, 22]. A recently published systematic review showed that 54 % of the studies used a salary-dependent definition such as “working for pay” or “earning minimum wage” [13]. The definition used in our study, being registered in the tax system as receiving any pay, was inclusive and led to a higher level than e.g., a definition of including those earning more than the minimum wage would have given. Despite the relatively high proportion receiving pay for work in this study, the considerably lower mean income levels compared with the matched controls indicate that many people who were employed after SCI still may not have achieved a satisfactory level of employment.
When it comes to the level receiving sickness and disability benefits, which was 67% after 6 years post-injury in our study, there are similar challenges regarding direct comparison. For previous studies with linkages to national registries, the levels reported have been 41 % 5 years after severe trauma in Norway [23], and 24% 5 years after mild traumatic brain injury in Denmark [24]. In our study, the high post-injury level of benefit receipt was probably partly influenced by the pre-injury level of sickness and disability benefits in the SCI sample (17%), which was elevated compared to controls (9%). This difference in pre-injury benefit status is in line with findings from a nationwide Danish register-based SCI study that showed approximately two times higher health care costs for persons with SCI two years before injury, compared to controls [25]. We found their explanation, that this might be related to ongoing disease in advance of non-traumatic SCI, and a traumatic SCI group that could be more accident-prone, both resulting in higher costs, plausible and relevant for our findings.
Increasing labour market participation
Even if the current study showed a relatively high level of labour market participation for persons with SCI, efforts should be made to increase it further, especially because a considerable group is not included in the labour market after SCI (mainly the more severely injured and low educated persons). At the same time, the importance of work in people’s lives is well known [1, 26].
The factors found in this study to influence labour market participation following SCI, neurological outcome, level of education, age at injury, time since injury, and pre-injury attachment to employment, strongly confirming findings from previous studies [2,3,4,5,6]. Of these, gaining additional education is a factor that can be modified after the injury [3]. Higher educated persons are more often in non-physically demanding employment compared to those with lower education [27]. Consequently, persons with higher education post-SCI tend to have more career opportunities open to them [27]. Thus, promoting vocational re-training towards jobs requiring higher education is likely to be a valid approach to increase the level of labour market participation [27,28,29].
But also measures taken at the workplace should be considered. One example is assistive technologies which have been suggested to be helpful for those with limited cognitive resources to do physically oriented jobs [27]. Also increased employer incentives, such as obligations regarding offering a suitable job and providing workplace adaptations could be useful [9]. Previous research has indicated that the role of the employers is underutilised in Norway [5].
Study strengths and limitations
Strength of this study is the nationwide register-based and controlled design, with clinical patient data from a national medical SCI quality registry linked with complete individual national registry data on employment, education, income, and social security benefits. This linkage provides high accuracy and quality owing to the use of the unique identity number assigned to all Norwegians. Use of registry data minimizes the risk of information bias, compared with patient-reported outcome measures [30]. Moreover, we had access to data of the general population and could therefore provide a detailed comparison between people with SCI and the general population.
There are some noteworthy limitations. In general, one should be careful with making causal interpretations of the findings. Registry data provide limited information on personal characteristics (including health status) to be used as adjustment variables in the regression analyses. In addition, registry data is not well suited to study quality of employment that would be of importance for labour market participation after SCI, such as the promotions and job satisfaction.
Only persons with SCI that received pay for work in the year before injury were included in this study, which means that the results are not generalizable to all persons with SCI. Furthermore, the number of control persons per patient varied from zero to five, introducing some imbalance in the composition of the control sample. The comparisons between the SCI sample and control sample must therefore be interpreted with caution. However, we have taken this imbalance into account by performing analyses within matched groups.
The outcome pay for work is based on annual registrations, with the consequence that those with SCI are registered with income the year of their injury.
Conclusion
Labour market participation clearly decreased after injury among persons with SCI. Even though a relatively large proportion of those who participated in the labour market before SCI still did so after injury, more than half of these also depended on sickness and disability benefits. Even stronger emphasis of vocational re-training towards jobs requiring higher education, more flexible workplace adaptations and more employer incentives should be considered to increase labour market participation for persons with SCI.
Data availability
The data used in this study are from the NorSCIR, SSB and NAV. There are restrictions on the use of data from national registries. These data were used under licence for the current study and are not publicly available.
References
Bickenbach J International perspectives on spinal cord injury. Geneve: WHO/ International Spinal Cord Society; 2013. Available from: https://apps.who.int/iris/handle/10665/94190.
Ottomanelli L, Lind L. Review of critical factors related to employment after spinal cord injury: implications for research and vocational services. J Spinal Cord Med. 2009;32:503–31.
Trenaman L, Miller WC, Queree M, Escorpizo R, Team SR. Modifiable and non-modifiable factors associated with employment outcomes following spinal cord injury: A systematic review. J Spinal Cord Med. 2015;38:422–31.
Leiulfsrud AS, Solheim EF, Reinhardt JD, Post MWM, Horsewell J, Biering-Sorensen F, et al. Gender, class, employment status and social mobility following spinal cord injury in Denmark, the Netherlands, Norway and Switzerland. Spinal Cord. 2020;58:224–31.
Solheim E, Leiulfsrud A. Employment after spinal cord injury in Norway: A cross-sectional survey. Scand J Disabil Res. 2018;20:197–210.
Krause JS, Terza JV, Erten M, Focht KL, Dismuke CE. Prediction of postinjury employment and percentage of time worked after spinal cord injury. Arch Phys Med Rehabil. 2012;93:373–5.
Post MW, Reinhardt JD, Avellanet M, Escorpizo R, Engkasan JP, Schwegler U, et al. Employment among people with spinal cord injury in 22 countries across the world: results from the International Spinal Cord Injury Community Survey. Arch Phys Med Rehabil. 2020;101:2157–66.
Roels EH, Reneman MF, New PW, Kiekens C, Van Roey L, Townson A, et al. International comparison of vocational rehabilitation for persons with spinal cord injury: systems, practices, and barriers. Top Spinal Cord Inj Rehabil. 2020;26:21–35.
Hemmings P, Prinz C. Sickness and disability systems: comparing outcomes and policies in Norway with those in Sweden, the Netherlands and Switzerland. 2020.
Norwegian Ministry of Labour and Social Affairs. Work and benefits, measures to increase employment.: Norwegian Ministry of Labour and Social Affairs; 2019 [Available from: https://www.regjeringen.no/contentassets/b9ac9f756f21467f8a3230e9a8cdafa4/en-gb/pdfs/nou201920190007000engpdfs.pdf.
Statistics Norway. Labour force survey 2021 [Updated 27.01.22; cited 2022 10.02.2022]. Available from: https://www.ssb.no/en/arbeid-og-lonn/sysselsetting/statistikk/arbeidskraftundersokelsen.
Lidal IB, Hjeltnes N, Roislien J, Stanghelle JK, Biering-Sorensen F. Employment of persons with spinal cord lesions injured more than 20 years ago. Disabil Rehabil. 2009;31:2174–84.
Bloom J, Dorsett P, McLennan V. Investigating employment following spinal cord injury: outcomes, methods, and population demographics. Disabil Rehabil. 2019;41:2359–68.
The Research Council of Norway. Evaluation of Biology, Medicine and Health Research in Norway (2011). 2011. Report No.: ISBN 978-82-12-03001-5 (print), ISBN 978-82-12-03002-2 (pdf).
Halvorsen A, Pettersen AL. Annual reports Norwegian Spinal Cord Injury Registry. 2022 [cited 2022 01.03.2022]. Available from: https://stolav.no/fag-og-forskning/medisinske-kvalitetsregistre/norsk-ryggmargsskaderegister-norscir#rapporter.
NorSCIR. Norwegian Spinal Cord Injury Registry 2022 [01.03.2022]. Available from: www.norscir.no.
Statistics Norway. About Statistics Norway: SSB; 2022 [Available from: https://www.ssb.no/en/omssb/ssbs-virksomhet.
Statistics Norway. Access to data from Statistics Norway: SSB; 2022 [01.03.2022]. Available from: https://www.ssb.no/en/data-til-forskning.
Norwegian Labour and Welfare Administration. Norwegian Labour and Welfare Administration 2019 [updated last update 05.09.2022. Available from: https://www.nav.no/en/home/benefits-and-services/information-about-nav-s-services-and-benefits.
Norwegian Labour and Welfare Administration. Data og forskning på NAV 2020 [updated last update 23.03.2022. Available from: https://www.nav.no/no/nav-og-samfunn/kunnskap/data-og-forskning-pa-nav.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Lidal IB, Huynh TK, Biering-Sorensen F. Return to work following spinal cord injury: a review. Disabil Rehabil. 2007;29:1341–75.
Uleberg O, Pape K, Kristiansen T, Romundstad PR, Klepstad P. Population-based analysis of the impact of trauma on longer-term functional outcomes. Br J Surg. 2019;106:65–73.
Graff HJ, Siersma V, Moller A, Kragstrup J, Andersen LL, Egerod I, et al. Labour market attachment after mild traumatic brain injury: nationwide cohort study with 5-year register follow-up in Denmark. BMJ Open. 2019;9:e026104.
Soendergaard PL, Norup A, Kruse M, Biering-Sorensen F. Socioeconomic consequences of traumatic and non-traumatic spinal cord injuries: a Danish nationwide register-based study. Spinal Cord. 2022;60:647–54.
Leiulfsrud AS, Ruoranen K, Ostermann A, Reinhardt JD. The meaning of employment from the perspective of persons with spinal cord injuries in six European countries. Work 2016;55:133–44.
Schwegler U, Nutzi M, Marti A, Trezzini B. Swi SCIsg. Pre- and post-injury job type distributions of individuals with SCI in relation to structural changes in the labor market: A comparative analysis based on findings from the Swiss Spinal Cord Injury Cohort Study. J Spinal Cord Med. 2021;44:77–88.
Sturm C, Bokel A, Korallus C, Geng V, Kalke YB, Abel R, et al. Promoting factors and barriers to participation in working life for people with spinal cord injury. J Occup Med Toxicol. 2020;15:37.
Halvorsen A, Pape K, Post MWM, Biering-Sorensen F, Mikalsen S, Hansen AN, et al. Participation and quality of life in persons living with spinal cord injury in Norway. J Rehabil Med. 2021;53:jrm00217.
Hjollund NH, Larsen FB, Andersen JH. Register-based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Public Health. 2007;35:497–502.
Acknowledgements
The authors thank user representatives Monica Engelsjord, Anders Nupen Hansen, and Steinar Mikalsen for using their personal experiences to give input on the study design and for reporting the results. We further thank the three SCI specialized centers, located at Haukeland University Hospital, St Olav’s University Hospital, and Sunnaas Rehabilitation Hospital, for registration in NorSCIR, the steering committee of the Norwegian SCI registry (NorSCIR) for providing access to the data, and Ann Louise Pettersen for delivering the data.
Funding
The funding for the research project which this study was part of came from Dam Foundation (Grant number 2018/FO198620), the Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology (NTNU) (Grant number 18/420) and the joint research committee between St. Olavs hospital HF and the Faculty of Medicine and Health Sciences at NTNU (Grant number 2018/42795).
Author information
Authors and Affiliations
Contributions
AH was the main investigator of the study and the main contributor in the writing of the paper. AH, KP and AS were responsible for designing the study with support from MP and FBS. AH was responsible for the data collection. AH and KP analysed and interpreted the data. AH, KP and AS prepared and revised the drafts of the manuscript. ASL, MP and FBS provided feedback on the manuscript. All authors have given their final approval of the version to be submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interests. AH is the leader of NorSCIR but had no role in granting access to or delivery of the NorSCIR data.
Ethics approval
Ethical approval for this study was obtained from the Regional Committee for Medical and Health Research Ethics in Mid Norway (2018/294/REK-midt). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Halvorsen, A., Steinsbekk, A., Leiulfsrud, A.S. et al. Labour market participation after spinal cord injury. A register-based cohort study. Spinal Cord 61, 244–252 (2023). https://doi.org/10.1038/s41393-023-00876-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00876-4