Abstract
Study design:
Systematic review.
Objectives:
Review the literature on the acute or prophylactic treatment of autonomic dysreflexia in the context of sexual activities.
Setting:
International
Methods:
Medline search using AD and spinal cord injury and all years of publication.
Results:
Thirty-seven papers on the specific treatment of AD showed that nifedipine, prazosin, captopril and clonidine are candidates in the context of sexual activities. Prazosin, however, has an initial hypotensive effect requiring to begin treatment 12 h before intercourse, which makes it less ideal for spontaneous sexual activities. Captopril has an initial hypotensive effect and was only studied in acute AD. Its usefulness in prophylaxis remains to be demonstrated. Clonidine has successfully been used clinically for decades, but never studied in randomized control trials. Nifedipine remains the most widely studied and significant treatment of AD whether in acute or prophylactic conditions. Recent concerns suggest increased cardiovascular risks with sublingual nifedipine in non-SCI populations, but negative long-term effects have not been reported in the SCI population.
Conclusion:
Sexual function is a priority for men with SCI. As sexual activities, in particular ejaculation, can be a source of AD, adequate treatments and prophylaxis must be considered in the context of sexual activities. Experts must meet and conclude on the thresholds, parameters and treatments that should be considered in the long-term management of AD in the context of sexual function in men with SCI.
Similar content being viewed by others
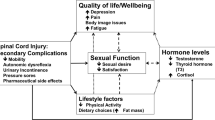
Introduction
A spinal cord injury disrupts several aspects of life. Among them, sexuality is considered a major concern and described as a priority.1 Although sexual function is usually lost following natural stimulation,2 successful treatments are now available, allowing the vast majority of men with SCI to achieve ejaculation.3, 4, 5
Sexual options for men with SCI
Ejaculation dysfunctions in men with SCI can be treated with a variety of options, starting with commercial vibrators, followed if unsuccessful by the use of the Ferticare device,6 which has been shown much more effective, followed if still negative by vibrostimulation combined with midodrine.7 When fertility is aimed for, rectal probe electroejaculation8, 9 and other assisted reproductive technologies can be offered, allowing intravaginal home injection,10 intrauterine or in vitro fertilization.11
Sexuality and fertility are therefore definite options for men with SCI, and considering the currently available treatments, more than 90% of men with SCI can achieve ejaculation.4, 5 The resulting response is accompanied with many sexual sensations12 including orgasm13, 14 despite the spinal cord lesion. Vibrostimulation is a common prescription in this context and a key option, as it can use it at home, with no medical assistance, alone or with a partner. Ejaculation is not only sought for fertility, but also to obtain sexual gratification and relieve spasticity.15, 16
Despite these beneficial effects, ejaculation may place some individuals with SCI at risk of developing autonomic dysreflexia (AD),17, 18 a condition which raises medical concerns. Although the question is not to deprive men with SCI from experiencing sexual gratification, AD risks warrant further investigation on the prevention strategies that can be proposed for sexual activities.
This paper reviews the literature on the treatment of AD to provide a better information on its prevention and management in the context of sexuality.
Materials and methods
A systematic review of the literature from Pubmed was conducted on studies that provided scientific evidence on the specific treatment of AD following SCI. The search used the keywords autonomic dysreflexia AND spinal cord injury, as well as autonomic hyperreflexia AND spinal cord injury. All years of publication were considered, which ranged from 1956 to 2011. The papers were assessed by two independent reviewers on the basis of their abstract, which had to mention that they specifically investigated a treatment of AD, that is, with a group comparison or with an indication of a therapeutic effect before and after treatment. The selected papers aimed all levels of evidence, including randomized placebo control, case reports and literature reviews, as long as they pertained to the specific treatment of AD. Because the literature review aimed treatments that can be implemented at home during sexual activities, studies on intravenous treatment were generally rejected, except for one study that used intravenous specifically in the context of ejaculation manoeuver in men with SCI. Also excluded were studies that only mentioned a procedural management of AD in their methods without giving specific results (hence not specifically studying AD treatment). A secondary search using the keywords vibrostimulation AND spinal cord injury, electroejaculation AND spinal cord injury, and ejaculation AND spinal cord injury was performed in this context and ranged from 1948 to 2011. The articles were read to assess whether they mentioned only a procedural management of AD or whether they specifically investigated a treatment of AD.
Results
The keywords on autonomic dysreflexia AND spinal cord injury gave rise to 558 articles and that on autonomic hyperreflexia AND spinal cord injury to 662 articles. The papers mentioning a specific treatment of AD lead to 50 articles. Considering only those on humans, only written in English or French and eliminating those with intravenous treatments left 37 articles pertaining to the specific treatment of AD, although not necessarily restricted to sexual activity. The secondary search relating to sexual activity using the keywords vibrostimulation AND spinal cord injury gave rise to 196 articles, that with electroejaculation AND spinal cord injury 110 articles and that with ejaculation AND spinal cord injury 267 articles. Of these studies 60% mentioned procedural managements of AD but without specific results. Three studies gave some results on a treatment effect on AD and were also found under the keywords on autonomic dysreflexia, therefore, included in the current review.
Autonomic dysreflexia
First described in 1890 by Bolby,19 AD is now considered a clinical emergency.20, 21 Its primary definition relies on hypertension and is characterized by an increase in systolic blood pressure of at least 20 mm Hg.17, 21, 22 AD is usually associated with at least one sign of autonomic arousal,17 but may sometimes occur unperceived.23 Upon severe conditions, hypertension can reach levels as high as 250 mm Hg18 SBP, making the individual at risk of organ dysfunction, cardiovascular events or even death if left untreated.
AD is therefore a potentially life-threatening condition. As sexual activities in particular ejaculation can trigger AD,17 while the individual is at home with no medical assistance, understanding its mechanisms and providing adequate prevention or treatment become a priority in the context of sexuality.
Pathophysiology of AD
The most common sources of AD are summarized in Table 1 and include ejaculation or its treatment. AD generally affects individuals with lesions above T6,17, 20, 21 where supraspinal inhibition can no longer act on the sympathetic outflow.
AD is initiated by intense or painful or sustained stimuli,17 traveling through the somatic and visceral afferents to the thoracic segments of the spinal cord.24 Postganglionic sympathetic terminals then release norepinephrine (NE)25, 26 that triggers a sudden generalized vasoconstriction, resulting in hypertension and visceral spasms. Visceral spasms further cause vasoconstriction, which further stimulates the sympathetic terminals and self-perpetuates the phenomenon.
Mathias et al.20 demonstrated that NE released from the sympathetic terminals were responsible for AD, as opposed to epinephrine released from the adrenal medulla (that is, greater plasma levels of NE compared with epinephrine). AD is therefore a primary sympathetic phenomenon stimulating predominantly alpha-adrenergic smooth muscles.
Hypertension25 triggered during AD episodes17 activates baroreceptors in the carotid sinus and aortic arch, which stimulate two reflexes, one involving the vagal nerve and causing bradycardia, and another involving inhibition of descending sympathetic pathways.24, 25, 26, 27 As this inhibition can no longer reach the spinal segments below the lesion, diverging symptoms are observed above and below the lesion (Table 2).
The hyperactive sympathetic syndrome has been explained by various mechanisms, the first involving the loss of supraspinal inhibition, resulting in the massive reflex discharge described above. Increased liberation of NE in response to normal stimuli and hyper-responsiveness to alpha stimulation28 have also been suggested, along with a decreased threshold for NE release. Recent evidence29, 30, 31 further suggests that sprouting of visceral or somatosensory afferents occurs following SCI and increases the synaptic potential, thereby lowering the threshold for sympathetic discharge and rendering previously non-painful stimuli sufficient to trigger AD.
The severity of the AD episodes appears to increase with the levels and extent of injury,17 higher and complete lesions being more vulnerable.26 Posttraumatic delays also appear to have a role, as AD usually develops within the first year post injury, although rarely before the first two months post injury.26
Clinical management of AD
The Consortium for Spinal Cord Medicine32 as well as Blackmer25 and Krassioukov et al.’s33 reviews recommend the use of non-pharmacological manoeuvres as a first treatment of AD. The standard protocol32 involves uplifting the individual, lowering the lower limbs, removing compressive clothing below the lesion level, verifying the flow of urinary catheter, voiding the bladder or rectal ampulla, and continuously monitoring blood pressure.
When SBP remains above 150 mm Hg despite these manoeuvres, pharmacological treatment is introduced.33 Treatments are usually considered when SBP reaches 150 mm Hg based on the criteria for primary hypertension. However, some procedures in rehabilitation, such as cystometry and cystoscopy, trigger rises in SBP, which sometimes exceed this threshold. Although treatment may then be implemented, tolerated thresholds of SBP are seldom described and usually left to clinical experience.
Ejaculation tests in men with SCI similarly involve higher SBP thresholds, which is not necessarily surprising given that non-SCI men show SBP rises from 140 mm Hg to 180 mm Hg at ejaculation.34 In our clinics, we therefore tend to use a threshold of 180 mm Hg SBP before considering pharmacological intervention5, 7, 12 unless the individual reports negative or uncomfortable side effects in which case the test is ceased and treatment implemented if side effects persist and blood pressure fails to diminish. Furthermore, when an individual is at risk of AD, prophylaxis treatment may also be considered.
Pharmacological treatment of AD
Studies specifically investigating the pharmacological treatments of AD include prophylaxis, acute as well as long-term treatments.
Treatment of AD during ejaculation procedures
Few studies have formally investigated the treatment of AD during ejaculation (Table 3), even though hundreds of papers described procedural managements of AD during ejaculation tests.3, 4, 8, 10, 11, 15 The outstanding majority of these studies used nifedipine (Adalat)3, 4, 8, 10, 11, 15, 35, 37 treatment. Others however attempted prazosin,37 sildenafil38 and prostaglandin E2,39 often with inconclusive results.
Nifedipine
Nifedipine is a calcium channel blocker acting on vascular smooth muscles and causing peripheral vasodilatation. Its sublingual absorption is effective within 5–10 min and its oral absorption within 45–60 min.
According to Braddom and Rocco,24 and Blackmer,25 nifedipine is the most widely used treatment of acute AD. VerVoort et al.35 and Steinberger et al.36 assessed its effectiveness as a preventive treatment of AD during electroejaculation and found that it significantly reduced peak35, 36 and average SBP,37 as well as AD symptoms35, 36 (such as, headache, sweating, general discomfort).
Sønksen et al.6 provided a comparison between individuals receiving nifedipine before vibrostimulation and those failing to receive such prophylaxis treatment, and showed an absence of AD symptoms in those treated.
Blackmer25 describes no clinical incident upon nifedipine treatment of AD, but a warning was emitted concerning the risks of cardiac events with sublingual nifedipine in non-SCI25, 40 populations. The warning raised concerns and resulted in the removal of the drug in some hospital settings, thereby motivating the search for alternatives.
Prazosin
Prazosin is a selective antagonist of alpha1-adrenergic receptors, which reduces the overall peripheral resistance associated with sympathetic activity. Its vasodilatation lowers blood pressure without affecting heart rate (HR), except for a slight reflex tachycardia when standing.
Szasz et al.37 attempted prazosin in prophylaxis 6–8 h before vibrostimulation and additionally 2 h before the tests for those with a history of AD. Only a few participants reported mild headache, but no other results are given, in particular, on blood pressure variations.
Braddom and Rocco24 indicate that prazosin was the third most used medication in 1991 to treat AD, but mention that the product can cause hypotension or syncope upon the first dose, suggesting to start treatment the evening before.
Sildenafil and prostaglandins
Sildenafil is a type 5 phosphodiesterase inhibitor delaying the degradation of phosphodiesterase in smooth muscles and resulting in relaxation and vasodilatation. As a vasodilator, it may potentially decrease blood pressure. Sheel et al.38 studied the effectiveness of sildenafil as a prophylaxis treatment of AD during vibrostimulation in men with lesions located above T6, but found no significant results. Severe hypotension in contrast was observed on some tetraplegic individuals.
Frankel et al.39 found that intravenously prostaglandin E2, another vasodilator, reduced blood pressure during electroejaculation, but the report only concerned three cases.
Treatment of AD during other AD triggering procedures
Other procedures, in particular, in urology are known to trigger AD and require preventive or acute treatments (Table 4).
Cystometry, cystoscopy
Dykstra et al.41 studied the effect of sublingual nifedipine during cystoscopy and found that it significantly decreased mean SBP and diastolic blood pressure (DBP). Lindan et al.42 similarly found that it decreased blood pressure within 30–40 min. Thyberg et al.43 showed that prophylactic nifedipine significantly reduced maximum SBP and DBP, and blood pressure during cystometry.
Extracorporeal shock wave lithotripsy
Kabalin et al.44 reported successful control of blood pressure with sublingual nifedipine during AD triggered by extracorporeal lithotripsy. Burstein et al.45 similarly showed a decrease in blood pressure from 240/123 mm Hg to 120/70 mm Hg in an individual experiencing AD during extracorporeal lithotripsy.
Nifedipine therefore shows significant effect not only as an acute treatment, but also as a prophylactic treatment of AD. However, as nifedipine can decrease resting blood pressure,42 individuals who are vulnerable to hypotension must be monitored before considering its prophylactic use.
Treatment of AD in other conditions
When individuals with SCI show a resting hypertension above 150 mm Hg SBP, with no identified cause, pharmacological treatment is implemented. Most reports again mention not only nifedipine, but also prazosin, captopril, clonidine and alpha1-adrenergic antagonists (Table 5).
Nifedipine
Rooney et al.46 reported successful treatment of an early case of AD with sublingual nifedipine in a tetraplegic man suffering from ileus. Chaves et al.47 reported successful treatment of AD with sublingual nifedipine in a tetraplegic woman submitted to a cough manoeuvre. Vaidyanathan et al.48 successfully treated recurrent AD with sublingual nifedipine in a tetraplegic man with chronic aortic dissection. Skowronski et al.49 reported beneficial effect sublingual nifedipine in a tetraplegic parturient.
Prazosin
Krum et al.22 found that prazosin, as an alpha1-adrenergic antagonist, was superior to placebo as a continuous treatment of AD in individuals experiencing AD for a week.
Captopril
Following the warning concerning the increased risks of cardiac conditions with sublingual nifedipine, Esmail et al.50 assessed the effectiveness of captopril sublingual. Captopril is an angiotensin-converting enzyme inhibitor, which blocks the renin–angiotensin–aldosterone system and causes a reduction in peripheral arterial resistance, without changing cardiac output. Esmail et al.50 found that the drug significantly reduced SBP during AD in four out of five participants, one requiring rescue therapy with nifedipine.
Clonidine
Clonidine is an alpha2-adrenergic agonist that causes inhibition of the sympathetic outflow and decreases vascular resistance. According to Blackmer,25 clonidine is a common treatment of AD, and according to Braddom and Rocco24 8% of experts use clonidine as an acute treatment of AD. No systematic studies, however, can be found on the product, although four case reports show clinical improvements.
Wright et al.51 successfully treated a paraplegic man suffering from a neuroblastoma and experiencing AD upon bowel distension with clonidine. Hall et al.52 showed that clonidine lowered peaks of pressure during dressing changes in a tetraplegic man suffering from buttock ulcer. Roche et al.53 described five cases of hypertension secondary to idiopathic high levels of catecholamines in paraplegic individuals, where four out of five responded positively to clonidine suppression. Skowronski et al.49 successfully treated AD with intramuscular clonidine to reduce pressure spikes in tetraplegic parturients.
Terazosin
Terazosin is an alpha1-adrenergic antagonist similar to prazosin but with a longer duration of action (24 h as opposed to 6–12 h). Similar to prazosin, it can cause orthostatic hypotension upon the first dose and it is recommended to start treatment the night before. According to Blackmer,25 terazosin is among the most widely used treatment for recurrent AD.
Vaidyanathan et al.54 showed that terazosin relieved the symptoms of recurrent AD in spinally injured individuals. Chancellor et al.55 showed that it significantly improved the severity and frequency of AD episodes long term, but did not change the intensity of headaches. Swierzewski et al.56 showed that daily terazosin during a month abolished or reduced AD episodes in four individuals with SCI.
Doxazosin
Doxazosin is another alpha1-adrenergic receptors antagonist successfully used44 to treat a tetraplegic man undergoing chronic aortic dissection. Despite this study, actually combining doxazosin with long-acting nifedipine,52 Krassioukov et al.,33 Blackmer,25 Braddom and Rocco24 all fail to include dozazosin as a recognized treatment of AD.
Phenoxybenzamine
Phenoxybenzamine is a long-acting non-selective antagonist of alpha-adrenergic receptors which, according to Braddom and Rocco24 in 1991, was the second most used drug for the treatment of minor AD. Krassioukov et al.,33 however, mention that there is conflicting evidence on its effectiveness. Lindan et al.42 compared it with nifedipine in prophylaxis during cystometry and found that both drugs reduced resting blood pressure, but failed to prevent AD during bladder distension. Both medications caused hypotension at rest, requiring discontinuation of treatment or reduction of dose in some participants. McGuire et al.57 reported positive effects of phenoxybenzamine, but animals studies showed tumor growths, suggesting a potential carcinogenic effect.24, 42 Phenoxybenzamine has therefore been eliminated as a treatment of AD.
Discussion
All in all, studies on the acute and prophylactic treatment of AD in individuals with SCI emphasize the effectiveness of nifedipine. Despite these results, the use of nifedipine has been questioned in a meta-analysis, yet performed on another population than SCI, but indicating that its sublingual use may increase the risk of myocardial infarction, stroke and severe hypotension.40 These warnings have motivated the search for alternatives. Yet, no adverse effects have been reported in the SCI population.32
Among alternatives, prazosin, clonidine and captopril have been found potential candidates. Prazosin,37 however, has a long delay of action (6–8 h), which requires a preliminary dose 12 h before its use (to counteract initial hypotension). This makes it less ideal for spontaneous sexual activities, especially as individuals with SCI complain that treatments for sexual dysfunctions often jeopardize the spontaneity of sexual acts. Prazosin, in this context, may be better suited for planned fertility tests rather than spontaneous sexuality. Prazosin also acts on smooth muscles and may increase the risk of retrograde ejaculation,37 again placing the drug as a less ideal candidate for sexual function.
Captopril is another product recommended as an alternative to nifedipine. Although successful for the treatment of acute AD,33, 50 its ability to prevent AD in prophylaxis during sexual activities remains unknown. Knowing that it has an initial hypotensive effect, its prophylactic use must be commended with care on tetraplegic individuals showing resting hypotension.
Clonidine has not been formally studied in randomized trials, but has been used in clinical practice for decades to prevent AD. Published case reports support its effectiveness for the acute and chronic treatment of AD in individuals with SCI.24, 25, 50, 52, 53 It may be a good candidate as a prophylactic treatment of AD in the context of sexual activities.
Sildenafil38 and prostaglandins,40 which can be used by men with SCI to control unstable or dysfunctional erections, have given inconclusive results. Although sildenafil failed to prevent AD,38 it was associated with severe hypotension at baseline in a small number of tetraplegic men but with significant results. Such findings reinforce the need and interest of clinical trials on the use of sildenafil at home for tetraplegic individuals.
Products such as terazosin, doxazosin and phenoxybenzamine have been ruled out as prophylactic treatments in the context of sexual activities based on their long delay of action, poor or lack of effect and hypotensive or carcinogenic potential. New treatments in contrast have not yet been tested empirically for the acute or preventive treatment of AD. Nitrol paste rapidly controls hypertension58 but its use may not be ideal with sexual activities where PDE5 inhibitors are also considered (risks of syncope).
Studies describing procedural management of AD mentioned nitroglycerine,57, 58, 59, 60, 61 a compound which we exclude because of the risks of severe hypotension when combined with PDE5 inhibitors. Others mention nicardipine,62 another calcium channel blocker but not available in North America. Earlier studies also mentioned phentolonium,63 dihydralazine,64 and general anaesthesia3, 15, 65, 66, 67, 68 during electroejaculation procedures,60, 61 but are not conceivable at home.
All in all, the current review emphasizes the effectiveness of nifedipine and leaves relatively few options for the treatment of AD in the context of sexual activities. With the currently provided approaches to anejaculation in men with SCI, in particular vibrostimulation and midodrine easily used at home, the question of AD risks and management become essential. Both vibrostimulation and midodrine maximize ejaculation, but both carry the risk of AD. Studies on midodrine,7 however, do not show higher increases in SBP at ejaculation compared with vibrostimulation alone, but increases in baseline SBP (that lowers the threshold for ejaculation).7 AD risk with midodrine is therefore similar to that with vibrostimulation and seems related to the occurrence of ejaculation itself. Upon AD risks, the Consortium for Spinal Cord Medicine32 suggests that the ideal drug should have a rapid onset, short duration of action, few side effects, and be safely used at home. In this context, nifedipine remains an ideal candidate. Given the recent concerns on cardiovascular events, perhaps oral nifedipine would be preferred over sublingual to reduce its rapid and steep action precipitating cardiovascular risks.
When to use acute pharmacological or prophylaxis treatment for AD
Aside from these concerns on the ideal medication for AD in individuals with SCI, questions have been raised during this review on the threshold and parameters that should be considered for AD management. The Consortium for Spinal Cord Medicine suggests that a threshold of 150 mm Hg SBP be considered to implement pharmacological treatment, based on the treatment of primary hypertension in non-SCI populations.32 However, rehabilitation practice, particularly urology, often exceeds this threshold to complete cystometric or cystoscopic procedures. Although clinical judgement then decides on when and whether to treat AD, no published data appears to be available on the range and parameters that are considered in such cases.
Ejaculation tests performed on men with SCI can also exceed the threshold of 150 mm Hg SBP, in particular because normal ejaculation in able-bodied men already involves 140 to 180 mm Hg peaks.33 Although severe hypertension in men with SCI has exceeded these values,18 the maximum threshold that should be allowed during ejaculation tests is not discussed. The Paraplegic Veterans of America guidelines mention a threshold of 150 mm Hg SBP to implement treatment. This threshold suggests that many, if not most ejaculation tests with tetraplegic men, should provide AD treatment. This further raises the question of home use of vibrostimulation and the concerns associated with nifedipine risks. A discussion among professionals should probably be encouraged for a consensus to be reached on these thresholds and issues, especially upon home ejaculation.
Aside from these SBP values, DBP and HR are seldom mentioned as parameters of AD or as a sign of successful treatment. The primary definition of AD relies on hypertension, but specific criteria are seldom given for DBP (>90 mm Hg)17 and none for HR, even though both are considered in the diagnosis of both primary hypertension (SBP consistently >140 mm Hg, DBP consistently >90 mm Hg).69 In our practice, DBP can rise beyond 100 mm Hg at ejaculation, which raises the question of silent hypertension. The importance of HR can similarly be raised. As bradycardia often occurs during AD, values below 40 beats per min are considered critical by our teams, but fortunately have never been observed during our ejaculation tests.
While attempting prophylactic treatment of AD based on the above criteria, a new problem is raised when the individual’s resting blood pressure is particularly low, for example, in tetraplegic men. Men with such lesions often exhibit initial SBP within 80–90 mm Hg, which questions the minimal threshold that can be accepted before a prophylaxis treatment can be planned. The literature is silent on this issue. The same applies for the other cardiovascular parameters, DBP or HR. Knowing that men with SCI experience sexual activities at home, and knowing that options such as vibrostimulation and oral midodrine are available to help them achieving ejaculation,3, 4, 5, 6, 7 these issues become essential in the management of sexual function in individuals with SCI.
While debating on the thresholds and parameters to be considered, individuals with SCI may be systematically encouraged to purchase a sphygmomanometer, especially those with higher lesions and vulnerable to AD. McBride et al.70 showed that SBP could triple at ejaculation in tetraplegic individuals and while these cases are isolated in the literature and in our clinical experience, SBP rises between 200 and 230 mm Hg are encountered. Silent AD can further be observed at these values, making the warning more critical for individuals at risk. Although seldom discussed during intercourse—perhaps because natural ejaculation is rarely observed in men with SCI—information on AD should be provided to every individual at risk. Perhaps an assessment of ejaculation should be systematically offered before leaving rehabilitation to avoid undue risk at home. Educating the individuals about the various signs of hyper or hypotension, other than readings from the sphygmomanometer may also be considered (especially if they fail to use it during spontaneous sexual activities). In this context, we developed a questionnaire13 to help men with SCI recognizing the signs of autonomic responses during ejaculation. It could be useful to identify signs of AD, particularly in the context of silent or asymptomatic AD.23
Conclusion
Concerns about AD during sexual activity and about the long-term management of sexual function in individuals with SCI raise several issues: determining the SBP threshold at which pharmacological treatment of AD should be implemented or systematic prophylaxis considered exploring whether DBP and/or HR parameters should also be considered in the decision, which DBP/HR thresholds should then be considered before implementing treatment, whether patients should be systematically assessed for ejaculation before leaving rehabilitation, whether they should be encouraged to purchase a sphygmomanometer, what signs if any should be emphasized to draw the patients’ attention on hyper or hypotension and how to educate patients on silent AD.
When treatment is implemented, nifedipine appears to be the best candidate despite recent concerns about its long-term cardiovascular risks in non-SCI populations. The Consortium for Spinal Cord Medicine,32 however, reveals no negative side effects on patients with SCI. Perhaps oral rather than sublingual nifedipine would be more secure.
Experts should meet and conclude on the thresholds and parameters to be considered in AD to provide a safe prevention during sexual activities, especially knowing that sexuality is a priority for individuals with SCI.
References
Anderson KD, Borisoff JF, Johnson RD, Stiens SA, Elliot SL . The impact of spinal cord injury on sexual function: Concerns of the general population. Spinal cord 2007; 45: 328–337.
Bors E, Comarr AE . Neurological disturbances of sexual function with special reference to 529 patients with spinal cord injury. Urol Surv 1960; 10: 191–222.
Biering-Sorensen F, Sonksen J . Sexual function in spinal cord lesioned men. Spinal Cord 2001; 39: 455–470.
Brackett NL, Lynne CM, Ibrahim E, Ohl DA, Sønksen J . Treatment of infertility in men with spinal cord injury. Nat Rev Urol 2010; 7: 162–172.
Courtois F, Charvier K, Vézina J-G, Carrier S, Morel Journel N, Jacquemin G et al Assessment of sexual potential and treatment of sexual dysfunctions in men and women with spinal cord injury. In: Tanya C, (ed.) Berkovsky, Handbook of Spinal Cord Injuries: Types, Treatments and Prognosis. Nova publishers: New York. 2009.
Sønksen J, Biering-Sørensen F, Kristensen JK . Ejaculation induced by penile vibratory stimulation in men with spinal cord injuries. The importance of the vibratory amplitude. Paraplegia 1994; 32: 651–660.
Courtois FJ, Charvier KF, Leriche A, Vézina J-G, Côté M, Bélanger M . Blood pressure changes during sexual stimulation, ejaculation and midodrine treatment in spinal cord injured men. BJU Int 2008; 101: 331–337.
Fode M, Krogh-Jespersen S, Brackett NL, Ohl DA, Lynne CM, Sonksen J . Male sexual dysfunction and infertility associated with neurological disorders. Asian J Androl 2012; 14: 61–68.
Seager SWJ, Halstead LS . Fertility options and success after spinal cord injury. Spinal Cord Injury 1993; 20: 543–548.
Sønksen J, Sommer P, Biering-Sørensen F, Ziebe S, Lindhard A, Loft A et al Pregnancy after assisted ejaculation procedures in men with spinal cord injury. Arch Phys Med Rehabil 1997; 78: 1059–1061.
Shieh JY, Chen SU, Wang YH, Chang HC, Ho HN, Yang YS . A protocol of electroejaculation and systematic assisted reproductive technology achieved high efficiency and efficacy for pregnancy for anejaculatory men with spinal cord injury. Arch Phys Med Rehabil 2003; 84: 535–540.
Courtois F, Charvier K, Leriche A, Vézina J-G, Côté I, Raymond D et al Perceived physiological and orgasmic sensations at ejaculation in spinal cord injured men. J Sex Med 2008; 5: 2419–2430.
Courtois F, Charvier K, Vézina J-G, Morel Journel N, Carrier S, Jacquemin G et al Assessing and conceptualizing orgasm after a spinal cord injury. BJUI 2011; 108: 1624–1633.
Alexander M, Rosen RC . Spinal cord injuries and orgasm: a review. J Sex Marital Ther 2008; 34: 308–324.
Biering-Sørensen F, Laeessøe L, Sønksen J, Bagi P, Nielsen JB, Kristensen JK . The effect of penile vibratory stimulation on male fertility potential, spasticity and neurogenic detrusor overactivity in spinal cord lesioned individuals. Acta Neurochir Suppl 2005; 93: 159–163.
Courtois F, Geoffrion R, Landry E, Bélanger M . H reflex and physiologic measures of ejaculation in men with spinal cord injury. Arch Phys Med Rehabil 2004; 85: 910–918.
Alexander MS, Biering-Sorensen F, Bodner D, Brackett NL, Cardenas D, Charlifue S et al International standards to document remaining autonomic function after spinal cord injury. Spinal Cord 2009; 47: 36–43.
Elliot S, Krassioukov A . Malignant autonomic dysreflexia in spinal cord injured men. Spinal Cord 2006; 44: 386–392.
Bowlby AA . On condition of reflexes in cases of injury to spinal cord; with special reference to indications for operative interference. Med Chir Tr 1890; 73: 317–325.
Mathias CJ, Frankel HL . Cardiovascular control in spinal man. Annu Rev Physiol 1988; 50: 577–592.
Teasell RW, Arnold JM, Krassioukov A, Delaney GA . Cardiovascular consequences of loss of supraspinal control of sympathetic nervous system after spinal cord injury. Arch Phys Med Rehabil 2000; 81: 506–516.
Krum H, Louis WJ, Brown DJ, Howes LG . A study of the alpha-1 adrenoceptor blocker prazosin in the prophylactic management of autonomic dysreflexia in high spinal cord injury patients. Clin Auton Res 1992; 2: 83–88.
Ekland M, Krassioukov A, McBride KE, Elliott SL . Incidence of autonomic dysreflexia and silent autonomic dysreflexia in men with SCI undergoing sperm retrieval: implications for clinical practice. J Spinal Cord Med 2007; 30: 43–50.
Braddom RL, Rocco JF . Autonomic dysreflexia: a survey of current treatment. Am J Phys Med Rehabil 1981; 70: 234–241.
Blackmer J . Rehabilitation medecine: 1. Autonomic dysreflexia. CMA J 2003; 169: 931–935.
Campagnolo DI, Merli GJ . Autonomic and cardiovascular complications of spinal cord injury. In Kirshblum S, Campagnolo DI, DeLisa JA, (eds). Spinal Cord Medicine. Lippincott Williams & Wilkins: Philadelphia. 2002 pp 123–134.
Furlan JC, Fehlings MG, Shannon P, Norenberg MD, Krassioukov AV . Descending vasomotor pathways in humans: correlation between anxonal preservation and cardiovascular dysfunction after spinal cord injury. J Neurotrauma 2003; 20: 1351–1363.
Arnold JM, Feng QP, Delaney GA, Teasell RW . Autonomic dysreflexia in tetraplegic patients: evidence for alpha-adrenoceptor hyper-responsiveness. Clin Auton Res 1995; 5: 267–270.
Krassioukov AV, Bunge Ruckett WR, Bygrave MA . The changes in human spinal cord sympathetic preganglionic neurons after spinal cord injury. Spinal Cord 1999; 37: 6–13.
Krassioukov AV, Johns DG, Schramm LP . Sensitivity of sympathetically correlated spinal interneurons, renal sympathetic nerve activity, and arterial pressure to somatic and visceral stimulate after chronic spinal injury. J Neurotrauma 2002; 19: 1521–1529.
Krassioukov AV, Weaver LC . Morphological changes in sympathetic preganglionic neurons after spinal cord injury in rats. Neuroscience 1996; 70: 211–225.
Consortium for Spinal Cord Medicine. Acute Management of Autonomic Dysreflexia: Individuals with Spinal Cord Injury Presenting to Heath Care Facilities 2nd ed Paralyzed Veterans of Americas: Washington, DC. 2001.
Krassioukov A, Warburton DE, Teasell R, Eng JJ . Spinal Cord Injury Rehabilitation Evidence Research Team. A systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil 2009; 90: 682–695.
Masters WH, Johnson VE . Human Sexual Response. Little Brown: Boston. 1966.
VerVoort SM, Donovan WH, Dykstra DD, Syers P . Increased current delivery and sperm collection using nifedipine during electroejaculation in men with high spinal cord injuries. Arch Phys Med Rehabil 1988; 69: 595–597.
Steinberger RE, Ohl DA, Bennett CJ, McCabe M, Wang SC . Nifedipine pretreatment for autonomic dysreflexia during electroejaculation. Urology 1990; 36: 228–231.
Szasz G, Carpenter CH . Clinical observations in vibratory stimulation of the penis of men with spinal cord injury. Arch Sex Behav 1989; 18: 461–474.
Sheel AW, Krassioukov AV, Inglis JT, Elliot SL . Autonomic dysreflexia during sperm retrieval in spinal cord injury: influence of lesion level and sidenafil citrate. J Appl Physiol 2005; 99: 53–58.
Frankel HL, Mathias CJ . Severe hypertension in patients with high spinal cord lesions undergoing electroejaculation-management with prostaglandin E2. Paraplegia 1980; 18: 293–299.
Grossman E, Messerli FH, Grodzicki T, Kowey P . Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA 1996; 276: 1328–1331.
Dykstra DD, Sidi AA, Anderson LC . The effect of nifedipine on cystoscopy-induced autonomic hypperreflexia in patients with high spinal cord injuries. J Urol 1987; 138: 1155–1157.
Lindan R, Leffler EJ, Kedia KR . A comparison of the efficacy of an alpha-1-adrenergic blocker in the slow calcium channel blocker in the control of autonomic dysreflexia. Paraplegia 1985; 23: 34–38.
Thyberg M, Ertzggard P, Gylling M, Granerus G . Effect of nifedipine on cystometry-induced elevation of blood pressure in patients with a reflex urinary bladder after a high level spinal cord injury. Paraplegia 1994; 32: 308–313.
Kabalin JN, Lennon S, Gill HS, Wolfe V, Perkash I . Incidence and management of autonomic dysreflexia and other intraoperative problems encountered in spinal cord injury patients undergoing extracorporeal shock wave lithotripsy without anesthesia on a second generation lithotriptor. J Urol 1993; 149: 1064–1067.
Burnstein A, Richlin D, Sotolongo JR . Nifedipine pretreatment for prevention of autonomic hyperreflexia during anesthesia-free extracorporeal shock wave lithotripsy. J Urol 1992; 147: 676–677.
Rooney KD, McKinstry C . Early autonomic dysreflexia in acute paraplegia following anterior spinal artery thrombosis. Anaesth Intensive Care 2007; 35: 769–770.
Charves CJ, Lee G . Reversible posterior leukoencephalopathy in a patient with autonomic dysreflexia: a case report. Spinal Cord 2008; 46: 760–761.
Vaidyanathan S, Hughes PL, Oo T, Soni BM . Recurrent autonomic dysreflexia due to chronic aortic dissection in an adult male with cervical spinal cord injury. Sci World J 2008; 8: 604–610.
Skowronski E, Hartman K . Obstetric management following traumatic tetraplegia: case series and literature review. Aust N Z J Obstet Gynaecol 2008; 48: 485–491.
Esmail Z, Shalansky KF, Suderji R, Anton H, Chambers K, Fish W . Evaluation of captopril for the management of hypertension in autonomic dysreflexia: a pilot study. Arch PhysMed Rehabil 2002; 83: 604–608.
Wright KC, Agre JC, Wilson BC, Theologis A . Autonomc dysreflexia in a paraplegic man with catecholamine-secreting neuroblastoma. Arch Phys Med Rehabil 1986; 67: 566–567.
Hall PA, Young JV . Autonomic hyperreflexia in spinal cord injured patients: trigger mecanism-dressing changes of pressures sores. J Trauma 1983; 23: 1074–1075.
Roche WJ, Nwofia C, Gittler M, Patel R, Yarkony G . Catecholamine-induced hypertension in lumbosacral paraplegia: five case reports. Arch Phys Med Rehabil 2000; 81: 222–225.
Vaidyanathan S, Soni BM, Sett P, Watt JW, Oo T, Bingley J . Pathophysiology of autonomic dysreflexia: long-term treatment with terazosin in adult and paediatric spinal cord injury patients manifesting recurrent dysreflexic episodes. Spinal Cord 1998; 36: 761–770.
Chancellor MB, Erhard MJ, Hirsch IH, Stass WE . Prospective evaluation of terazosin for the treatment of autonomic dysreflexia. J Urol 1994; 151: 111–113.
Swierzewski SJ, Gormley EA, Belville WD, Sweetser PM, Wan J, McGuire EJ . The effect of terazosin on bladder function in the spinal cord injured patient. J Urol 1994; 151: 951–954.
McGuire J, Wagner FM, Weiss RM . Treatment of autonomic dysreflexia with phenoxybenzamine. J Urol 1976; 115: 53–55.
Backo AL, Clause SL, Triller DM, Gibbs KA . Clonidine-induced hypertension in a patient with a spinal lesion. Ann Pharmacother 2002; 36: 1396–1398.
Brackett NL . semen retriveal by penile vibratory stimulation in men with spinal cord injury. Hum Reprod Update 1999; 5: 216–222.
Halstead LS, Seager AWJ . The effects of rectal probe electrostimulation on spinal cord injury spasticity. Paraplegia 1991; 29: 43–47.
Halstead LS, Seager SWJ, Houston JM, Whitesell K, Dennis M, Nance PW . Relief of spasticity in SCI men and women using rectal probe electrostimulaiton. Paraplegia 1993; 31: 715–721.
Groothuis JT, Rongen GA, Deinum J, Pickkers P, Danser AH, Geurts AC et al Sympathetic nonadrenergic transmission contributes to autonomic dysreflexia in spinal cord-injured individuals. Hypertension 2010; 55: 636–643.
Piera A . Sexual and genital prognosis in adult paraplegics. Paraplegia 1972; 10: 456–477.
Siösteen A, Forssman L, Steen Y, Sullivan L, Wichström I . Quality of semen after repeated ejaculation treatment in spinal cord injury men. Paraplegia 1990; 28: 96–104.
Nehra A, Werner MA, Bastuba M, Title C, Oates RD . Vibratory stimulation and rectal probe electroejaculation as therapy for patients with spinal cord injury: semen parameters and pregnancy rates. J Urol 1996; 155: 554–559.
Rutkowski SB, Geraghty TJ, Hagen DL, Bowers DM, Craven M, Middleton JW . A comprehensive approach to the management of male infertility following spinal cord injury. Spinal Cord 1999; 37: 508–514.
Shieh JY, Chen SU, Wang YH, Chang HC, Ho HN, Yang YS . A protocol of electroejaculation and systematic assisted reproductive technology achieved high efficiency and efficacy for pregnancy for anejaculatory men with spinal cord injury. Arch Phys Med Rehabil 2003; 84: 535–540.
Sonksen J, Sommer P, Biering-Sorensen F, Ziebe S, Lindhard A, Loft A et al Pregnancy after assisted ejaculation procedures in men with spinal cord injury. Arch Phys Med Rehabil 1997; 78: 1059–1061.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL et al Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–1252.
Mc Bride F, Quah SP, Scott ME, Dinsmore WW . Tripling of blood pressure by sexual stimulation in a man with spinal cord injury. J R Soc Med 2003; 96: 349–350.
Acknowledgements
We thank Dr Nancy Michelle Robitaille for her comments on the Ethics proposal from this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Courtois, F., Rodrigue, X., Côté, I. et al. Sexual function and autonomic dysreflexia in men with spinal cord injuries: how should we treat?. Spinal Cord 50, 869–877 (2012). https://doi.org/10.1038/sc.2012.83
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.83