Abstract
Study design:
Several causes of Brown-Sequard syndrome have been described. Endovascular embolization can be used to treat symptomatic vertebral hemangiomas. We describe a previously undocumented case of Brown-Sequard syndrome followed by endovascular embolization with microcoils of a vertebral hemangioma. We also provide a clinical-radiological correlation of this finding and review the relevant literature.
Case report:
A 39-year-old male was referred to our hospital for endovascular treatment of a right T9 hemivertebral hemangioma with compromise of the spinal canal. Fifteen minutes after the procedure, the patient developed right lower limb weakness and numbness on the left leg. The emergency magnetic resonance imaging (MRI) of the spine showed no abnormalities. Five days later, a new spinal MRI revealed an infarction in the right half of the spinal cord at T6 and T7 level. This stroke was probably caused by a microcoil ended up in the right sulcocommisural artery. One week after surgery, the patient was able to raise the right leg against gravity, but sensory deficit showed no improvement.
Conclusions:
To the best of our knowledge this is the first case of a Brown-Sequard syndrome related to vertebral hemangioma embolization, a relatively safe technique with no important complications made known until this report. Clinicians should always weight the benefits with the potential devastating complications of this therapeutic option.
Similar content being viewed by others
Introduction
Brown-Sequard syndrome (BSS) is defined as an incomplete lesion of the spinal cord characterized by ipsilateral upper motor neuron paralysis and loss of proprioception, with contralateral loss of pain and temperature sensation. As an incomplete spinal cord syndrome, the clinical presentation of Brown-Sequard syndrome may range from mild to severe neurologic deficit. The most frequent causes of BSS are traumatic injury, tumor, demyelinating lesions, infections or infarction, although other uncommon causes of BSS have been described.1, 2 We describe a previously undocumented case of BSS related to endovascular embolization with microcoils of a symptomatic vertebral hemangioma.
Case report
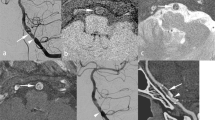
A 39-year-old male was referred to our hospital for endovascular treatment of a hemivertebral hemangioma at T9, involving the right T9 pedicle and compressing the spinal cord at the right T8–T9 level (Figures 1a and b), that produced an intractable back pain. His past medical history was unremarkable. Physical and neurologic exams before the procedure were rigorously normal. A retrograde catheterization of the right common femoral artery with a Judkins 4F catheter and a Progreat microcatheter was performed. Selective spinal angiography showed dilated vessels in the right T9 hemivertebra (Figure 2) suggesting a venous malformation that was embolized with microcoils in the right T8 and T9 intercostal arteries and injecting 100–300 μm embospheres. No neurologic deficits were observed during the procedure. Fifteen minutes later, the patient developed right lower limb monoplegia and numbness on the left leg. Neurologic examination, performed ∼12 h after the procedure, showed a reduced thermalgesic sensation in the left hemibody below T9 level. Vibration and position sensations were preserved. Deep tendon reflexes were very brisk in both legs, with right Achilles clonus and right Babinski's sign. There was no urinary retention or constipation. Spinal magnetic resonance imaging (MRI) showed no abnormalities at that time. One day later, the patient was able to raise the right lower limb from a supine position but the sensory deficits and reflexes remained unchanged. Five days later, a new spinal MRI was performed revealing a hyperintense T2-weighted triangular-shaped image in the right half of the spinal cord at T6–T7 level (Figures 1c and d). One week after the endovascular procedure, the patient was discharged. Neurologic examination at that moment showed mild weakness in the right leg (3/5), predominantly for foot dorsiflexion, and thermalgesic hypoesthesia in the left hemibody below T9. At 6-moths follow-up, without any specific therapy, he was able to walk, though unsteady, and sensation deficits and reflexes remained unchanged.
Spinal MRI (Siemens Symphony 1.5 Tesla) T2-weighted images before endovascular embolization, showing right locally aggressive hemivertebral hemangioma at T9 extending into the right T9 pedicle (a), compressing the spinal cord at the right T8–T9 level (b). Spinal MRI T2-weighted images after endovascular embolization demonstrating a triangular-shaped hyperintense image in the right side of the spinal cord at T6 and T7 level; axial view (c) and sagittal view (d).
Discussion
This case shows a precise clinical–radiological correlation of a right-sided ischemic spinal cord lesion at T9 following endovascular embolization of a vertebral hemangioma. The spinal cord infarction was likely caused by a microcoil flowing from the intercostal artery to the anterior spinal artery, which finally occluded the right sulcocommisural artery. Ischemic events in this artery have been implicated with BSS.3 Although highly unusual, endovascular embolization performed for other purposes, has been previously described as an iatrogenic cause of vertebral infarctions.4 However, to our knowledge, no cases of BSS after endovascular embolization with microcoils have been previously reported. In our patient, right hyperreflexia and Babinski's sign were noticed just ∼12 h after the procedure, which is infrequent, as hyperactive reflexes may not be present with acute spinal lesions and usually appear days or weeks after the injury. Symptomatic vertebral hemangiomas can be treated by surgical decompression, resection, vertebroplasty, transarterial embolization and radiation therapy.5 They can also be treated with intralesional injections of alcohol, although important complications such as BSS have been described.2 Endovascular treatment of vertebral hemangiomas can be used to alleviate intractable back pain and reduce the size of the hemangioma.5 To the best of our knowledge, this appeared to be a safe technique with no important complications described until this report. In conclusion, endovascular embolization for vertebral hemangiomas can give rise to BSS. Clinicians should individualize the patient selection, weighting the benefits against its potential devastating complications, and closely survey any new neurologic symptom after endovascular treatment of hemangiomas.
References
Hwang W, Ralph J, Marco E, Hemphill 3rd JC . Incomplete Brown-Sequard syndrome after methamphetamine injection into the neck. Neurology 2003; 60: 2015–2016.
Niemeyer T, McClellan J, Webb J, Jaspan T, Ramli N . Brown-Sequard syndrome after management of vertebral hemangioma with lesional alcohol. A case report. Spine 1999; 24: 1845–1847.
FitzGerald DB, Suran EL, Sargent J . Posterior circulation infarct after bronchial artery embolization and coiling. Neurology 2005; 65: 1312.
Finstein JL, Chin KR, Alvandi F, Lackman RD . Postembolization paralysis in a man with a thoracolumbar giant cell tumor. Clin Orthop Relat Res 2006; 453: 335–340.
Acosta FL, Dowd CF, Chin C, Tihan T, Ames CP, Weinstein PR . Current treatment strategies and outcomes in the management of symptomatic vertebral hemangiomas. Neurosurgery 2006; 58: 287–295.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fernandez-Torron, R., Palma, JA., Riverol, M. et al. Brown-sequard syndrome after endovascular embolization of vertebral hemangioma. Spinal Cord 50, 636–637 (2012). https://doi.org/10.1038/sc.2012.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.3
Keywords
This article is cited by
-
Spinal cord ischemia: aetiology, clinical syndromes and imaging features
Neuroradiology (2015)
-
Brown–Sequard described a rare, but important syndrome
Spinal Cord (2013)