Abstract
Purpose:
For patients with incomplete cervical cord injuries, appropriate urinary management based on an assessment of voiding and storage function of the bladder is necessary for a better prognosis, especially during the recovery phase. In our review of medical records of such patients, we identified factors related to recovery of bladder function and parameters for predicting prognosis.
Methods:
In this study, we included 234 patients with incomplete cervical cord injuries admitted to Kanagawa Rehabilitation Hospital. Their medical records were retrospectively reviewed for various parameters related to final urinary management measures at discharge. Parameters included age, severity of paralysis, bladder function over time, urinary sensation and cystometry results.
Results:
Patients were managed using urethral catheterization, suprapubic cystostomy, clean intermittent catheterization (CIC) by oneself or care givers, CIC with occasional spontaneous voiding, or spontaneous voiding alone. Bladder function improved in majority of the patients during hospitalization. The severity of paralysis and urinary sensation are predictive parameters for improvement in voiding function. In patients who were admitted with catheterization but were discharged with spontaneous voiding, the period for recovery was 85.2 days on average (range 16–142 days).
Conclusions:
Selection of urinary management measures for patients with incomplete cervical cord injuries can be performed adequately by considering the severity of paralysis and urinary sensation.
Similar content being viewed by others
Introduction
In developed countries, the incidence of spinal cord injuries from various traumatic and non-traumatic causes is 11.5–53.4 cases per million people per year.1 In Japan, most spinal cord injuries result in partial and incomplete paralysis, although about 20% of spinal cord injuries result in complete paralysis.2 The severity of spinal cord injuries is often evaluated according to the American Spinal Injury Association (ASIA) impairment scale. Patients with incomplete spinal cord injuries are categorized as class B through E by the AISA scale and, almost always have impairments in bladder function. The severity of the impairment varies substantially from patient to patient and dramatically changes over time, especially during the recovery phase. Therefore, bladder management during the recovery phase is critical for patients and medical staff to enable maximal recovery of bladder function and a better prognosis.
For proper management of urination, it is mandatory identify the actual status of voiding and storage disorders. From a practical point of view, it is advantageous to depict the plausible clinical courses of voiding and storage function of the blabber. In particular, we expected that certain parameters would be useful for predicting prognosis (that is, recovery of bladder function). Therefore, in this study, we reviewed the medical records of 234 patients with incomplete cervical cord injuries who spent their post-injury recovery phase at Kanagawa Rehabilitation Hospital.
Materials and methods
This study included 234 patients with incomplete cervical cord injuries in the recovery phase who were admitted to Kanagawa Rehabilitation Hospital for rehabilitation between April 2003 and March 2009. About 70% of cases were admitted between 1 and 4 months after the onset of injury or symptoms. The rest were admitted between 5 and 10 months after onset.
The patients’ medical records were retrospectively investigated to analyze clinical parameters related to urinary management at discharge. The parameters included age, sex, severity of paralysis upon hospitalization, state of micturition and its change during hospitalization, state of urinary sensation and results of cystometry.
The severity of paralysis was classified on the basis of the ASIA impairment scale. The ASIA impairment scale comprises five classes from A to E. Briefly, class A comprises complete cases, where motor or sensory function is completely lost in the sacral segments S4–5. Class B comprises incomplete cases, where sensory function alone is preserved below the neurological level. Classes C and D comprise cases where motor function alone is preserved below the neurological level. In Class C, more than half of the muscles below the neurological level are weakened to less than grade 3. In class D, muscles are maintained at grade 3 or above. Patients with motor and sensory function are classified as class E.
In most cases, urinary sensation was assessed at the time of cystometry as the presence or absence of the desire to urinate. Occurrence of detrusor overactivity during the urine storage phase was determined by cystometry. This study was approved by the Institutional Review Board at Kanagawa Rehabilitation Hospital. Statistically significant differences were analyzed by univariate analysis: Mann–Whitney’s U-test was used for age, and χ2-test was used for the other related factors. Factors in which significant differences were noted were further analyzed by multivariate analysis using logistic regression to determine the independence of these factors. The statistical software used was IBM SPSS Statistics 18 (IBM Japan, Tokyo, Japan).
Results
The age of patients at hospitalization ranged from 13 to 87 years (median, 61; mean±s.d., 57.2±14.0). Most of patients were between 50 and 69 years old. One hundred ninety-five patients were men, and 39 were women.
The causes of spinal cord injuries are summarized in Table 1. The majority of cases (204 cases) were caused by traumatic accidents, and remaining cases (30 cases) were caused by spinal cord disease. Traumatic accidents included tumbling, traffic accidents, falling from high places and sports-related injuries. The spinal cord diseases included spondylosis, spinal cord infarction, myelitis, spinal cord tumor, ossification of posterior longitudinal ligament and spinal canal stenosis.
The severity of paralysis upon hospitalization was evaluated using the ASIA impairment scale. Twenty-three patients (9.8%) were classified as class B; 90 patients (38.5%) were classified as class C, and 128 patients (51.7%) were classified as class D.
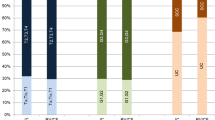
Figure 1 shows the methods for urinary management at the time of hospitalization and at discharge from the hospital. Upon hospitalization, 113 patients (48.3%) had urethral catheterization; 2 (0.9%) had suprapubic cystostomy with indwelling catheters; 13 (5.5%) required other persons for performing clean intermittent catheterization (CIC with nursing care); 2 (0.9%) performed CIC by themselves; 4 (1.7%) performed CIC with occasional spontaneous voiding, and 100 (42.7%) voided spontaneously. At the time of discharge from the hospital, 22 patients (9.4%) had urethral catheterization; 25 (10.7%) had suprapubic cystostomy, 6 (2.6%) performed CIC with nursing care, 37 (15.8%) performed CIC, 10 (4.3%) performed CIC with spontaneous voiding and 134 (57.2%) had spontaneous voiding. Thus, the proportion of patients with urethral catheterization decreased significantly, while that of patients with CIC and spontaneous voiding increased, indicating recovery from paralysis as well as improved bladder function during this period. There were no differences between the sexes.
Voiding methods at hospitalization and at discharge from the hospital. Approximately half of the patients had urethral catheterization upon hospitalization. At the time of hospital discharge, however, the percentage of patients with urethral catheterization was reduced, and more than half of the patients were able to void spontaneously.
The methods of voiding at the time of discharge were sub-categorized into groups based on the ASIA classification. The proportion of patients who voided spontaneously increased as the severity of paralysis was reduced. Specifically, the spontaneous-voiding rates of the patients in ASIA classes B, C and D were 13.0%, 37.8% and 80.2%, respectively, (P<0.001) (Figure 2). These findings demonstrate that milder paralysis favors improvement in micturition.
Next, we focused on 113 patients who had urethral catheterization upon hospitalization in order to identify parameters predictive of improved voiding function during the recovery phase. At the time of discharge, 35 patients were able to void spontaneously (spontaneous-voiding group), and the remaining 78 patients required catheterization (catheterization group). The catheterization group included not only patients with urethral catheterization, but also those with suprapubic cystostomy, CIC with nursing care, CIC and CIC with spontaneous voiding. The median ages of the spontaneous-voiding group and catheterization group were 60 years (mean±s.d.; 57.1±12.9) and 60 years (mean±s.d.; 57.4±12.9), respectively, with no significant difference between the groups (P=0.879). Urinary sensation at the time of cystometry was examined in all except 2 patients. Of the 35 patients in the spontaneous-voiding group, 31 (88.6%) expressed the desire to void, and 4 (11.4%) had an ambiguous urinary sensation, whereas no patient reported a lack of urinary sensation. Of the 76 patients in the catheterization group, 41 (53.9%) showed the desire to void; 11 (14.5%) had an ambiguous sensation of urination and 24 (31.6%) showed an absence of urinary sensation (P<0.001). Therefore, urinary sensation was considered an important parameter for predicting the prognosis of voiding function (Figure 3).
Presence or absence of urinary sensation in relation to voiding methods at the time of hospital discharge. None of the patients who were able to void spontaneously lacked urinary sensation; none of the patients who lacked urinary sensation at the time of hospitalization achieved spontaneous voiding at hospital discharge.
Data from cystometry performed on the available 108 patients were analyzed. Of the 34 patients in the spontaneous-voiding group, 17 (50.0%) showed normal results, and 17 (50.0%) showed detrusor overactivity. Of the 74 patients in the catheterization group, normal results were noted in 25 (33.8%) and detrusor overactivity was noted in 49 (66.2%). The percentage of patients with detrusor overactivity was slightly greater in the catheterization group, although the difference was not statistically significant (P=0.108) (Figure 4).
A multivariate analysis also revealed significant differences both in the severity of paralysis according to the ASIA classification (P=0.018) and the presence or absence of urinary sensation (P=0.005) (Table 2).
In the spontaneous-voiding group, the 33 patients who were hospitalized within 5 months after the onset of injury had a mean interval between the onset of injury and spontaneous voiding of 85.2 days (range: 16–142 days). Two patients in the spontaneous-voiding group who were hospitalized >5 months after injury were found to urinate spontaneously upon removal of the indwelling urethral catheters. Therefore, they were excluded from the assessments, because it was possible that the indwelling urethral catheters might have been kept in place unnecessarily. None of the patients was able to void spontaneously >5 months after the onset of injury.
Discussion
Management of urine excretion is important for the daily lives of patients with spinal cord injuries. As Lapides et al. proposed CIC in 1972, urinary tract management for such patients has dramatically improved.3 Before implementation of CIC, urinary tract infection was a major cause of death in patients with spinal cord injury. In the 1980s and 1990s, however, these disorders represented as low as 10% of all deaths from urinary tract infections.4 On the other hand, Soden et al.5 have reported survey results indicating that urinary tract infection remains an important factor determining the life span of patients with spinal cord injuries. Thus, it is important to offer adequate voiding management to such patients.
A survey of 269 American members of The Society for Urodynamics and Female Urology indicated that CIC in combination with anticholinergic drugs is a favorable method for management of detrusor overactivity in patients with spinal cord injuries.6 In the case of cervical cord injury, however, some patients cannot perform CIC by themselves, depending on their degree of tetraplegia. Independent CIC is performed at the level of C6B1.7 In addition, the severity of physical disorder substantially varies among patients with incomplete cervical cord injuries; as such, it is impossible to offer a particular measure method of urinary management without knowledge of their physical conditions and environmental situations. Therefore, it is necessary to assess individual patients for bladder function, voiding and storage ability accurately during the recovery phase. In the clinical settings, it is useful to know which parameters reliably predict prognosis for the recovery of bladder function. Such information is valuable for identifying the appropriate management plan for urination over the course of the disease.
In the present study, 49.2% of patients had indwelling catheters upon hospitalization, but only 20.1% did at the time of discharge. Iwatsubo8 evaluated recovery of voiding function in 16 patients with traumatic cervical cord injuries by voiding cystosphincterometry with uroflowmetry. Within 6 weeks (42 days), 14 patients had recovered from the shock phase, and in 13 weeks (91 days), 10 patients had become able to void, showing synchronization of urinary bladder contraction and relaxation of the external urethral sphincter. In this study, we observed several cases that recovered voluntary urination after up to 142 days of morbidity. On the other hand, there were cases of recovery of voluntary urination after longer than 5 months of morbidity. Therefore, 5 months after injury onset is an appropriate time point for assessing bladder management.
We also found that the severity of paralysis and urinary sensation were predictive parameters for improvement of voiding function. On the other hand, improvement could not be predicted based on age or cystometry data. However, we cannot exclude the possibility that cystometry is useful for evaluating bladder function and for predicting recovery. In fact, there are several urodynamic studies (UDS) on patients with spinal cord injuries reporting its usefulness for evaluation of bladder conditions. Chua et al.9 reported UDS of patients with incomplete cervical cord injuries: detrusor sphincter dyssynergia (DSD) was noted in 43.8% of patients; detrusor hyper-reflexia without accompanying DSD was noted in 31.3%, and areflexia or hyporeflexia was noted in 12.5%, whereas 12.5% normal UDS, indicating a high incidence of UD abnormalities. Gomelsky et al.10 performed UDS to evaluate the voiding status of 18 patients with spinal cord injuries due to ischemic disease and reported that UDS results were not associated with the causes or level of sensory disorders. However, they reported that incomplete cord injuries, specifically those classified as ASIA class D, may be associated with fewer UD abnormalities and a greater probability of volitional voiding. Therefore, UDS may be useful test for the long-term management of the urinary tract rather than for selecting the method of bladder voiding. Follow-up cystometry may also provide important information.
In the present study, we found that the severity of paralysis and urinary sensation are reliable and easily obtained data for predicting the prognosis of bladder function during the recovery phase of spinal cord injuries, particularly within 5 months after onset. Nonetheless, it remains important for urologists to perform regular follow-up care in order to evaluate the state of the urinary tract and to modify urine excretion measures as necessary.
References
Patki P, Woodhouse J, Hamid R, Shah J, Craggs M . Lower urinary tract dysfunction in ambulatory patients with incomplete spinal cord injury. J Urol 2006; 175: 1784–1787.
Shingu H, Ohama M, Ikata T, Katoh S, Akatsu T . A nationwide epidemiological survey of spinal cord injuries in Japan from January 1990 to December 1992. Paraplegia 1995; 33: 183–188.
Lapides J, Diokno AC, Silber SJ, Lowe BS . Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol 1972; 107: 458–461.
Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA et al Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992; 30: 617–630.
Soden RJ, Walsh J, Middleton JW, Craven ML, Rutkowski SB, Yeo JD . Causes of death after spinal cord injury. Spinal Cord 2000; 38: 604–610.
Razdan S, Leboeuf L, Meinbach DS, Weinstein D, Gousse AE . Current practice patterns in the urologic surveillance and management of patients with spinal cord injury. Urology 2003; 61: 893–896.
Asayama K, Kihara K, Shidoh T, Shigaki M, Ikeda T . The functional limitations of tetraplegic hands for intermittent clean self-catheterisation. Paraplegia 1995; 33: 30–33.
Iwatsubo E . Bladder recovery in patients with traumatic cervical cord injury evaluated by voiding synchronous cystosphincterometry with uroflowmetry. J Urol 1981; 126: 503–508.
Chua HC, Tow A, Tan ES . The neurogenic bladder in spinal cord injury—pattern and management. Ann Acad Med Singapore 1996; 25: 553–557.
Gomelsky A, Lemack GE, Weld KJ, Dmochowski RR . Urodynamic patterns following ischemic spinal cord events. J Urol 2003; 170: 122–125.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gohbara, A., Tanaka, K., Kawaji, K. et al. Urinary tract management in patients with incomplete cervical cord injury during the recovery phase. Spinal Cord 51, 310–313 (2013). https://doi.org/10.1038/sc.2012.138
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.138