Abstract
Objectives:
Hypertension (HTN) is an important risk factor for cardiovascular disease, a major cause of morbidity and mortality among people with spinal cord injury and disorders (SCI/D). Our study examined prevalence, associated factors, and pharmacological treatment of HTN in Veterans with SCI/D compared with a matched control group.
Methods:
A retrospective review was conducted of Veterans with traumatic SCI/D (TSCI/D; n=6672), non-traumatic SCI/D (NTSCI/D; n=3566) and a matched, non-injured cohort.
Results:
Over half of patients with TSCI/D (56.6%) had HTN, compared with 68.4% of matched controls (P<0.001). Paraplegic and tetraplegic Veterans with TSCI/D had significantly lower odds of having a HTN diagnosis compared with control (odds ratios (OR)=0.84 (0.77–0.91); OR=0.38 (0.35–0.42)). About 71.8% of patients with NTSCI/D had HTN compared with 72.3% of matched controls (P>0.05). Paraplegic and tetraplegic Veterans with NTSCI/D did not have significantly different odds of a HTN diagnosis compared with control (OR=0.92 (0.79–1.05); OR=0.85 (0.71–1.01)). Adjusted analysis indicates that Veterans with tetraplegia and HTN were less likely to receive antihypertensive therapy (TSCI/D, OR=0.62 (0.53–0.71); NTSCI/D, OR=0.81 (0.66–0.99)).
Conclusion:
HTN appears to be more prevalent in SCI/D Veterans than previously reported. TSCI/D Veterans have a significantly lower prevalence of HTN whereas NTSCI/D Veterans have a comparable prevalence of HTN to those without SCI/D. The level of injury (tetraplegia vs paraplegia) has a large impact on the prevalence of HTN in the traumatic cohort. Subsequent antihypertensive therapy is used less in both TSCI/D and NTSCI/D Veterans with tetraplegia and more in TSCI/D Veterans with paraplegia.
Similar content being viewed by others
Introduction
Hypertension (HTN) is a prevalent yet modifiable risk factor for cardiovascular disease (CVD).1, 2, 3 The VA/DoD Clinical Practice Guidelines Version 2.0b define HTN as a systolic blood pressure of over 145 mm Hg or a diastolic blood pressure over 90 mm Hg on two separate clinical evaluations. The most recent Joint National Committee’s report on high blood pressure described that ∼50% of all individuals, ages 60–69 years, and nearly 75% over the age of 70 years have a clinical diagnosis of HTN.1 Blood pressure measurements >130/85 mm Hg have been shown to increase the relative risk for CVD by greater than twofold when compared with individuals without HTN.1
CVD is a major cause of morbidity and mortality in patients with spinal cord injury and disorders (SCI/D).4, 5, 6 Septicemia, respiratory disorders and renal failure were once the primary cause of death in SCI/D patients.7 Treatments for these complications have continued to improve and SCI/D patients are now living an average of 20–40 years post-injury.8 As the life expectancy of individuals with SCI/D increases, the risk of developing CVD is a more significant concern. A recent study revealed that CVD was the cause of death for 40% of SCI/D Veterans.4 It is also suggested that patients with SCI/D experience CVD at an earlier age compared with the general population.8 CVD may be more difficult to detect in patients with SCI/D as they often do not experience specific symptoms, contributable to both loss of sensation and mobility.9
Blood pressure maintenance can be achieved by lifestyle modifications including diet, exercise and the control of comorbid conditions including diabetes.10 However, increasing exercise and maintaining an appropriate lean body-mass percentage are significant challenges for patients with SCI/D.11 In addition, injury to the spinal cord itself has a direct impact on the regulation of blood pressure. Physicians generally contend with conditions of low blood pressure including orthostatic hypotension, adaptive myocardial atrophy, bradyarrhythmia, reduced peripheral vascular resistance and venous pooling.12 However, it has been shown that the relative risk of HTN may increase with age in individuals with paraplegia and incomplete injuries.12, 13
The prevalence of HTN and associated variables in patients with SCI/D has been previously examined, but with contradictory findings. A study of Turkish SCI patients did not find a significant difference in the occurrence of HTN between individuals with and without SCI/D.14 This finding was likely owing to the small sample size and young age of the cohorts.14 Weaver et al.11 found that only 22% United States Veterans with SCI/D with a mean age of 58.2 years had HTN based on blood pressures available in clinical data warehouses. This was significantly lower than rates within the general population.11 Owing to the increasing prevalence of CVD in the SCI/D population and the known risks posed by high blood pressure, the role of HTN needs to be better defined.
Pharmacological intervention for HTN is effective in decreasing CVD morbidity and mortality.1, 13 At the time of our search, the prevalence or class of antihypertensive therapy used in the SCI/D patient population had not been reported.
The aims of our study were to examine prevalence, associated factors, and pharmacological treatment of HTN in a large cohort of Veterans with SCI/D and compare these with a matched control group.
Materials and methods
Study design and setting
A retrospective review of clinical and pharmacy data from the Department of Veterans Affairs (VA) was conducted on Veterans with SCI/D seen at VA healthcare facilities from fiscal years (FY) 2002–2008 (October 1, 2002 to September 30, 2008).
Study population
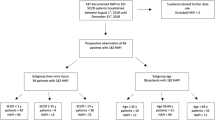
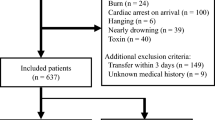
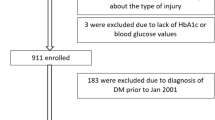
Veterans with SCI/D were identified from the VA Allocation Resource Center, which maintains a list of Veterans by diagnostic category. We excluded those with Multiple Sclerosis or Amyotrophic Lateral Sclerosis diagnoses using the VA medical inpatient and outpatient data sets and the VA Spinal Cord Dysfunction (SCD) registry. After exclusion this cohort is comprised of approximately 20 000 SCI/D Veterans who utilized services during the study timeframe. Our study looked specifically at medication prescription in FY 2008. The prescriptions were either newly prescribed medication or a previous prescription that was continued in 2008. Veterans who died before FY 2008 and their match were excluded from analysis (Figure 1).
Veterans with SCI/D were matched to non-SCI/D Veterans by age group (<30 years followed by 5-year blocks upto 80 and above), gender, first three digits of zip code and race (white, black and other). Veterans with SCI/D were divided into etiological categories of traumatic SCI/D (TSCI/D) or non-traumatic SCI/D (NTSCI/D) injuries or diseases. Recent studies have shown that the relative percentage of NTSCI/D is increasing and differs significantly from traumatic cases by being generally older, female, having increased comorbidities and an increased proportion of paraplegic injuries.15 Therefore traumatic and non-traumatic Veterans were analyzed separately to ease interpretation and application of results for these unique groups. Common causes of TSCI/D include motor vehicle accidents and falls, while NTSCI/D are often caused by spinal stenosis and neoplastic lesions.15
Data sources and measures
Demographics and diagnoses were extracted from the VA inpatient and outpatient MedSAS data sets. The National Spinal Cord Dysfunction registry was used to identify SCI/D characteristics: date, level (paraplegia/tetraplegia), completeness (complete/incomplete), and etiology (traumatic/non-traumatic) of injury. All of the aforementioned definitions were recorded by clinicians according to the International Standards for Neurological Classification of Spinal Cord Injury at the time of evaluation. The first three numbers of zip codes were used to merge census data from 2002. The Charlson Comorbidity Index is a validated method of classifying the effects of comorbidity in longitudinal studies. It was calculated using the classic 19 specified criteria excluding hemiplegia/paraplegia.16 Charlson scores were dichotomized into groups having 0, 1, 2 or 3 or more comorbidities. Any history of smoking was identified using International Classification of Diseases, Ninth Revision codes ‘305.1’, ‘649.0’ and V15.82.
Primary outcome measures included diagnosis of HTN documented within the 7-year study period, receipt of antihypertensive medication in FY 2008 and type of medications received. Diagnoses of HTN were identified using the International Classification of Diseases, Ninth Revision code ‘401.XX.’ Pharmacy data were obtained from the Decision Support System Pharmacy National Data Extract. Classification of prescription medication was based the VHA National Formulary and included: ACEI (benazepril, captopril, enalapril, enalaprilat, fosinopril and lisinopril), β-blockers (atenolol, bisoprolol, carvedilol, labetalol, metoprolol, propanolol and sotalol), thiazide diuretics (chlorothalidone, hydrochlorothiazide, indapamide and metolazone), calcium channel blockers (amlodipine, diltiazem, felodipine, nifedipine and verapamil), α-blockers (doxazosin, prazosin and terazosin), loop diuretics (bumetanide, ethacrynate and furosemide) and angiotensin II receptor antagonists (losartan and valsartan).
Statistical analyses
All analyses were conducted in Statistical Analysis Software (SAS) version 9.2 (SAS Institute, Cary, NC, USA). Descriptive statistics including χ2-test for dichotomous variables and t-tests for continuous variables were performed to analyze demographic information, characteristics of the SCI/D cohort and prescription of antihypertensive medications. Multiple logistic regression analyses were used to model factors associated with a HTN diagnosis from FY 2002–2008 and prescription of antihypertensive medication during FY 2008. These data are presented as both unadjusted and adjusted odds ratios (OR). The unadjusted OR includes analysis of only the particular variable, whereas the adjusted OR includes the described covariates.
Results
Demographics
The majority of Veterans were male (98%) and white. The average age of those with TSCI/D and NTSCI/D was 58.7 and 63.1 years, respectively. Additional demographic data are presented in Table 1. A significant amount of data regarding duration of injury and completeness of injury was missing and therefore not further examined. There were no differences between groups when examining gender, age and race (Table 1).
Prevalence of HTN and associated factors
A diagnosis of HTN was present in 56.6% of those with TSCI/D compared with 68.4% of their matched comparison group (P<0.001). No significant difference in unadjusted HTN prevalence was found between the non-traumatic cohorts (71.8% of those with NTSCI/D vs 72.3% of their match). Unadjusted factors associated with HTN in SCI/D Veterans are presented in Table 2 categorized by both etiology and level of SCI/D.
After controlling for demographics and comorbidities using logistic regression, Veterans with paraplegic and tetraplegic level TSCI/D had significantly lower odds of having a HTN diagnosis compared with controls (OR=0.84 (0.77–0.91); OR=0.38 (0.35–0.42); Table 3). Additional variables associated with HTN prevalence were being male, older, married, African-American/Black, having a higher Charlson Comorbidity score, a history of smoking, and from a low-income zip code.
Neither paraplegic nor tetraplegic Veterans with NTSCI/D had significantly different odds of a HTN diagnosis compared with their match after adjusting for covariates (OR=0.92 (0.79–1.05); OR=0.85 (0.71–1.01); Table 3). Associated variables included being older, married, African-American/black, having a higher Charlson Comorbidity score, and a history of smoking. (Table 3). In a separate sub-analysis, logistic regression was used to assess the association between HTN among TSCI/D and NTSCI/D Veterans independent of their matched cohorts. Injury etiology was a significant predictor of HTN, whereby Veterans with NTSCI/D had higher odds of having HTN compared with those with TSCI/D (OR=1.43 (1.23–1.66)), after controlling for available SCI characteristics, BMI, autonomic dysreflexia, demographics and comorbidities.
HTN was present in 42 of the 97 (43.3%) female Veterans with TSCI/D and 42 of the 72 (50%) female Veterans with NTSCI/D (P=0.08). Of those with HTN, age did not differ for female Veterans with NTSCI/D compared with females with TSCI/D (55.5±13.5 vs 51±11.0, P=0.06). Regression analysis of this subgroup was not possible owing to small sample size.
Antihypertensive medication
Over 75% of patients in each cohort with HTN received an antihypertensive medication in FY 2008 (Figure 2). No difference in receipt of antihypertensive medication was seen between SCI/D cohorts and their matched controls after stratification based on HTN diagnosis. Veterans with TSCI/D and HTN compared with their matched controls with HTN were less likely to be prescribed ACEI, Thiazide diuretics, calcium channel blockers and angiotensin II receptor antagonists, but were more likely to be prescribed loop diuretics (P<0.05). Those with NTSCI/D and HTN were less likely to be prescribed thiazide diuretics, calcium channel blockers and angiotensin II receptor antagonists, while more likely to receive β-blockers, α-blockers and loop-diuretics compared with their matched controls with HTN (P<0.05). TSCI/D patients also had lower odds of being prescribed more than one antihypertensive medication when compared with their matched comparison group (P<0.05).
Adjusted regression analysis of Veterans with HTN revealed that having a TSCI/D resulting in paraplegia increased the odds of being prescribed an antihypertensive medication (OR=1.24 (1.10–1.41)); while those with traumatic tetraplegic-level injuries were less likely to receive medication (OR=0.62 (0.54–0.72); Table 4).
Adjusted regression models revealed that NTSCI/D patients with tetraplegia, who had HTN, had significantly lower odds of receiving antihypertensive therapy when compared with control (OR=0.81, (0.76–0.99)). There was no statistical difference in the paraplegic NTSCI/D patients (OR=0.90 (0.76–1.06)). Analysis of this cohort also revealed that being male, older, married and having a higher Charlson Comorbidity significantly increased the odds of receiving an antihypertensive medication (all P<0.05).
Discussion
Data from our cohorts indicate that the prevalence of HTN may be higher in SCI/D patients than reported in previous studies.13 For example, a 2001 study reported only 22% of SCI/D Veterans to be hypertensive compared with our findings of 56.6% of those with TSCI/D and 71.8% of those with NTSCI/D.11 The average age of the cohort in the Weaver et al.11 study was 0.5 years younger than our TSCI/D and 4.9 years younger than our NTSCI/D cohort in this study. Our study also differs as it is focused on diagnosis and treatment of HTN whereas the Weaver study assessed blood pressure measurements. A study of 168 Veterans in California revealed 45% prevalence of HTN, of which 67% had paraplegia.17 Prevalence was also higher than reported in the recent Stockholm SCI study, which found 40% of their SCI/D cohort with post-traumatic paraplegia to have HTN.7 The higher prevalence may be partially attributed to the age of the cohorts, an increased duration of our retrospective review and the lack of NTSCI/D patients in the Stockholm study.
Our findings suggest that TSCI/D Veterans have a lower prevalence of HTN compared with a matched control, consistent with previously reported data.7, 11 Sympathetic dysfunction below the level of injury likely has a key role in this observation. This is supported with the finding that the odds of having HTN were much less in tetraplegic injuries (OR=0.36 (0.33–0.40)) versus paraplegic injuries (OR=0.84 (0.77–0.92)) when compared with matched controls.12 Coexisting conditions such as autonomic dysreflexia and orthostatic hypotension may also contribute to diagnostic confusion particularly in Veterans with tetraplegic TSCI/D.
Most known risk factors for HTN including increasing age, comorbidities and African-American race were consistently associated with higher prevalence of HTN. Interestingly, marriage appears to be risk factor for HTN in each subgroup of our population. This contrasts previous literature associating marriage with decreased prevalence of HTN.18 This may be secondarily owing to marital strain of a chronic disease. However, our data suggest increased likelihood of HTN independent of SCI/D. Smoking history was found to be a risk factor for HTN only in Veterans with tetraplegic injuries, regardless of etiology. This finding may reflect the vasoconstrictive role of nicotine in patients with autonomic dysregulation, as well as an increase in spasticity associated with nicotine use in patients with SCI/D.19
This study was unique in comparing HTN in TSCI/D and NTSCI/D. We found that Veterans with NTSCI/D had higher odds of having HTN compared with those with TSCI/D (OR=1.47 (1.27–1.70)), after controlling for available SCI characteristics, age, demographics and comorbidities. And unlike TSCI/D injuries, there was no significant change in the odds of having HTN in both paraplegic and tetraplegic injuries when compared with their matched controls. The increased likelihood of HTN in Veterans with NTSCI/D may be owing to later onset of SCI/D and differences in impairment, which were not analyzed in this study because of a large number of missing data. No past studies analyzing HTN in only NTSCI/D could be found for comparison. Future prospective studies are needed to confirm that NTSCI/D patients are as likely to develop HTN as the general population.
Veterans with TSCI/D resulting in tetraplegia had lower odds of receiving medication treatment after being diagnosed with HTN. Additionally, TSCI/D patients with HTN were less likely to be prescribed >1 antihypertensive medication when compared with match control. These findings are likely owing to concern over the propensity for these patients to develop hypotension. Contrastingly, TSCI/D resulting in paraplegia increased the odds of receiving antihypertensive medication after a diagnosis of HTN. This discovery may be owing to the increase in frequency of care following a TSCI/D. Additional variables may be contributing these discrepancies and should be examined in future studies.
ACEIs were the most likely prescribed medication for the TSCI/D cohort and both control cohorts. This is consistent with a recent study within the VA in which ACEI were found to be the most prevalently prescribed antihypertensive medication.13 We found that, compared with matched controls, patients with TSCI/D as well as NTSCI/D were less likely to receive thiazide diuretics, which are recommended as first-line antihypertensive agent in the general population. This may reflect a reluctance to use these agents in patients with SCI/D because of potential effect on urine volumes and bladder management programs using intermittent bladder catheterization, a common management strategy for SCI/D.
Strengths of this study include a large sample size and the use of a matched control group for both TSCI/D and NTSCI/D. Limitations include confinement to coded diagnoses from the VA database rather than recorded blood pressure measurements. This may allow for missed or inaccurate diagnoses of HTN and associated comorbidities. However, previous analyses have shown that coding for the VA medical data sets is reliable.20 Our results may also have limited generalizability given that our cohort was solely of Veterans, most of whom were white males. This study is additionally limited by grouping level of injury into paraplegia or tetraplegia. It is likely that Veterans with higher levels of paraplegic injuries above the level of T6 may have autonomic instability more comparable with Veterans with tetraplegia, and we cannot be sure as to what proportion of our cohort may fit this description.
It remains a challenge to fully ascertain the role of HTN in the development on CVD in SCI/D Veterans. Future prospective studies may be helpful in further examining blood pressure measurements, medication adherence and comorbid outcomes of CVD owing to HTN in this patient population.
In conclusion, HTN appears to be more prevalent in SCI/D Veterans than previously reported. Our data also suggest that Veterans with TSCI/D have a lower prevalence of HTN compared with matched control whereas Veterans with NTSCI/D have a similar prevalence of HTN. The level of injury (tetraplegia vs paraplegia) appears to more significantly impact the prevalence of HTN for the traumatic cohort compared with the non-traumatic. Subsequent antihypertensive therapy appears to be used significantly less in both TSCI/D and NTSCI/D Veterans with tetraplegia and more in TSCI/D Veterans with paraplegia.
Data archiving
There were no data to deposit.
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–1252.
Yusuf HR, Giles WH, Croft JB, Anda RF, Casper ML . Impact of multiple risk factor profiles on determining cardiovascular disease risk. Prev Med 1998; 27: 1–9.
Strandberg TE, Salomaa VV, Vanhanen HT, Pitkala K . Blood pressure and mortality during an up to 32-year follow-up. J Hypertens 2001; 19: 35–39.
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D et al A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005; 43: 408–416.
Banerjea R, Sambamoorthi U, Weaver F, Maney M, Pogach LM, Findley T . Risk of stroke, heart attack, and diabetes complications among veterans with spinal cord injury. Arch Phys Med Rehabil 2008; 89: 1448–1453.
Bauman WA, Spungen AM . Coronary heart disease in individuals with spinal cord injury: assessment of risk factors. Spinal Cord 2008; 46: 466–476.
Wahman K, Nash MS, Westgren N, Lewis JE, Seiger A, Levi R . Cardiovascular disease risk factors in persons with paraplegia: the Stockholm spinal cord injury study. J Rehabil Med 2010; 42: 272–278.
Yekutiel M, Brooks ME, Ohry A, Yarom J, Carel R . The prevalence of hypertension, ischaemic heart disease and diabetes in traumatic spinal cord injured patients and amputees. Paraplegia 1989; 27: 58–62.
Groah SL, Weitzenkamp D, Sett P, Soni B, Savic G . The relationship between neurological level of injury and symptomatic cardiovascular disease risk in the aging spinal injured. Spinal Cord 2001; 39: 310–317.
Kahn R, Robertson RM, Smith R, Eddy D . The impact of prevention on reducing the burden of cardiovascular disease. Circulation 2008; 118: 576–585.
Weaver FM, Collins EG, Kurichi J, Miskevics S, Smith B, Rajan S et al Prevalence of obesity and high blood pressure in veterans with spinal cord injuries and disorders: a retrospective review. Am J Phys Med Rehabil 2007; 86: 22–29.
Grigorean VT, Sandu AM, Popescu M, Iacobini MA, Stoian R, Neascu C et al Cardiac dysfunctions following spinal cord injury. J Med Life 2009; 2: 133–145.
Furmaga EM, Cunningham FE, Cushman WC, Dong D, Jiang R, Basile J et al National utilization of antihypertensive medications from 2000 to 2006 in the Veterans Health Administration: focus on thiazide diuretics. J Clin Hypertens 2008; 10: 770–778.
Demirel S, Demirel G, Tukek T, Erk O, Yilmaz H . Risk factors for coronary heart disease in patients with spinal cord injury in Turkey. Spinal Cord 2001; 39: 134–138.
Guilcher SJ, Munce SE, Couris CM, Fung K, Craven BC, Verrier M et al Health care utilization in non-traumatic and traumatic spinal cord injury: a population-based study. Spinal Cord 2010; 48: 45–50.
Charlson ME, Pompei P, Ales KL, MacKenzie CR . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383.
Lee MY, Myers J, Abella J, Froelicher VF, Perkash I, Kiratli BJ . Homocysteine and hypertension in persons with spinal cord injury. Spinal Cord 2006; 44: 474–479.
Keenan NL, Rosendorf KA . Centers for Disease Control and Prevention (CDC). Prevalence of hypertension and controlled hypertension – United States, 2005-2008. MMWR Surveill Summ 2011; 60 (Suppl): 94–97.
Shefner JM, Berman SA, Young RR . The effect of nicotine on recurrent inhibition in the spinal cord. Neurology 1993; 43: 2647–2651.
Kashner TM . Agreement between administrative files and written medical records: a case of the Department of Veterans Affairs. Med Care 1998; 36: 1324–1336.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Disclaimer
This material is based upon work supported in part by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, the Department of Veterans Affairs Spinal Cord Injury Quality Enhancement Research Initiative (SCI QUERI) and by grant #2618 from the PVA Research Foundation. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Rights and permissions
About this article
Cite this article
Barry, W., St Andre, J., Evans, C. et al. Hypertension and antihypertensive treatment in veterans with spinal cord injury and disorders. Spinal Cord 51, 109–115 (2013). https://doi.org/10.1038/sc.2012.122
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.122