Abstract
Study design:
Retrospective descriptive observational study.
Objective:
The primary objective of this study was to quantify the incidence of iatrogenic spinal cord injury (SCI) at our SCI unit (SCIU). The secondary objective was to discover the surgical and medical procedures that cause iatrogenic SCI and to estimate the incidence with each procedure.
Subjects:
Patients admitted to or seen at outpatient services of the SCIU at a university hospital.
Methods:
Histories were compiled from 1 July 2005 to 30 June 2009. We included patients with SCI caused by any medical or surgical procedure. We collected age, sex, diagnosis leading to medical intervention, predominant clinical manifestations, medical–surgical procedure and level and grade of injury upon admission and discharge.
Results:
Out of 250 patients admitted to the SCIU, 32 (14.7%) patients presented iatrogenic SCI. Average age was 56.2 (s.d. 17.3), ranging from 0 to 82 years old. The most frequent clinical manifestation was pain. The most common diagnosis was channel stenosis. Lumbar level grade C of American Spine Injury Association (ASIA) was the most frequently observed.
Conclusion:
The rise in the population's life expectancy entails an increase in elderly patients with vascular risk factors, who underwent invasive interventions leading to spinal cord iatrogenia.
Similar content being viewed by others
Introduction
Iatrogenic disorder (from the Greek iatros: doctor; genus: origin) is defined as any adverse condition in a patient, occurring as a result of treatment by a physician, a surgeon or other health professionals. It has currently been expanded to define any undesirable event, experienced by a patient, directly resulting from a medical intervention. Iatrogenia is more frequent than what is believed and it is an obvious risk for patients.1 The concept of iatrogenia must not be confused with malpractice.
A spinal cord injury (SCI) may result from an iatrogenic intervention with ethical, legal and financial repercussions.2
In literature, there are series of isolated cases, although very few general reviews covering the various etiologies of iatrogenia in SCI, which focus especially in surgical treatment. The causes found are the following:
-
Surgical: laminectomy,3 discectomy,4 arthrodesis,5, 6 scoliosis,7 exeresis of calcified yellow ligaments,8 vascular surgery,9, 10 use of surgicel.11, 12
-
Interventionist techniques: vertebroplasty,13 arterial embolization,14 epidural anesthesia,15 intramuscular injections,16 acupuncture.17
-
Drugs: platelet antiaggregants,18 acenocumarol,19 tumor necrosis factor.20
-
Physical therapy: manipulation.21
Our working hypothesis focuses on the perception that lately, there has been an increase in the incidence of SCI due to iatrogenic causes.
The primary objective of our study was:
-
1
To quantify the incidence of iatrogenic SCI at our SCI unit (SCIU). Our secondary objectives were:
-
2
To learn which surgical and medical procedures lead to iatrogenic SCI.
-
3
To estimate the incidence of iatrogenic SCI derived from each diagnostic or therapeutic procedures.
Materials and methods
A retrospective descriptive study consisting in the review of the clinical histories of patients admitted to or seen in outpatient services of the SCIU at the Hospital La Fe in Valencia, whose SCI was iatrogenic.
Study period
We compiled data from patients admitted to the unit from 1 July 2005 to 30 June 2009.
Subjects
The inclusion criteria were: patients presenting spinal cord or cauda equina injury preceded by any diagnostic, surgical, pharmacological or physical therapy procedure carried out by healthcare professionals or prescribed by a physician.
The exclusion criteria were: (i) patients who underwent surgery due to tumors, as we consider that SCI is an inevitable side effect if borders are to be left disease free and (ii) patients treated with oral anticoagulants, presenting SCI after a severe traumatic event, given that it is not possible to ascertain whether the traumatism in itself could have caused the SCI.
During the study period, 250 patients were admitted to the SCIU, of which 32 met the criteria.
The SCIU at the Hospital La Fe is the reference unit for treating SCI in the Community of Valencia, which has a population of 4.1 million. The patients coming to the SCIU have been diagnosed or intervened at the hospital or at other hospitals in the region. In the Hospital La Fe 33 210 admissions occur each year, of which 2555 are due to traumatic emergency. A total of 17 380 elective surgeries and 6779 urgent surgeries are performed every year. The hospital has services of cardiac surgery, thoracic surgery and spine surgery unit.
Patients were divided into two groups: those who underwent invasive procedures (surgery and intervention), and those subject to non-invasive procedures (drugs and physical therapy).
We referred to the archive of clinical histories at our hospital and obtained the total number of patients intervened during the study period, with the following procedures: arthrodesis, laminectomy, vertebroplasty, bronchial artery embolization and oral anticoagulants.
Variables
For each patient, we collected age, sex, diagnosis leading to medical intervention, predominant clinical manifestations resulting in medical intervention, medical–surgical procedure causing iatrogenia, day stay, level and grade of the injury upon admission and discharge. If the patient had undergone an invasive procedure, we also collected data from evoked potential tests and whether the patient received megadoses of corticosteroids.
Statistical methods
In order to find the incidence, we divided the number of patients with SCI due to iatrogenia admitted by the total number of patients admitted to the SCIU. Then calculated the confidence interval (CI) 95%.
In order to find significant differences between the injury levels and between grades, we used the χ2-test.
To check whether there were statistically significant differences between the groups in the days and motor score variables upon admission and discharge, we used Student's t-test, as they were continuous variables.
The statistical significance level established was P<0.05.
To confirm all hypotheses, we used the program SPSS v.15 (SPSS Inc., Chicago, IL, USA).
Results
A total of 250 patients were admitted to the SCIU, of which 26 met the criteria, which gives an incidence of iatrogenic event in SCI of 10.4% (CI±3.8%). We found six patients more, who were seen in outpatient services; we decided to include them in the rest of analysis, total 32 patients. Eight patients (25%) underwent non-invasive procedures and 24 patients underwent (75%) invasive procedures. In all, 19 patients were female (59%) and 13 patients were male (41%). Average age was 56.2 (s.d. 17.3), ranging from 0 to 82 years old, with 75% of the patients aged over 44 years. The average age of the patients who underwent a non-invasive intervention was 61.3 (s.d. 19.4), the average age of the patients intervened was 54.5 (s.d. 16.5). No significant differences were observed between the groups (P=0.338). One was a child, who, due to administrative regulations, could not be admitted into our unit and the other five were grade D injuries that improved rapidly. The average stay at the SCIU for patients undergoing non-invasive treatment was 56.8 days (s.d. 41.6); for patients undergoing invasive treatment, the average was 79.1 days (s.d. 53.8). We noted that there were no significant differences between the groups with Student's t-test (P=0.334).
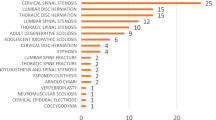
The diagnoses leading to medical intervention are shown in Table 1.
When we analyze the causes that lead to iatrogenic event, spine pain or irradiation are the most frequent with 14 cases (43.8%)
Table 2 shows the various interventions carried out on the patients and how many of them were conducted at the Hospital La Fe.
Table 3 shows diagnosis upon admission to the SCIU.
The levels involved and the American Spine Injury Association (ASIA) grade are shown in Table 4.
Upon admission, average ASIA score was 64.9 points (s.d. 22.2). Upon discharge from SCIU, average ASIA score was 73.6 points (s.d. 19), with an improvement of 8.1 points (s.d. 12.1). These results were significant (P=0.001).
The units from where the patients came are shown in Table 4.
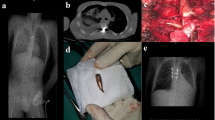
Four out of the 24 intervened patients underwent intraoperative monitoring with evoked potentials, and all cases were normal.
During the study period, our hospital carried out a total of 1034 vertebral arthrodeses, of which four suffered a resulting SCI, reflecting an incidence of 0.48% (CI (95%)±0.42%). A total of 1132 laminectomies were conducted at our hospital during the study period, of which three led to an SCI. The incidence calculated was 0.26% (CI (95%)±0.29%).
Our hospital carried out 35 bronchial artery embolizations, of which three suffered an SCI. This gives an incidence of 8.6% (CI (95%)±8.9%).
A total of 113 vertebroplasties were conducted at our hospital, causing one SCI, producing an incidence of 0.9% (CI (95%)±1.7%).
A total of 3900 patients were treated with oral anticoagulation during the study period in our area, of which two suffered SCI, rendering an incidence of 0.05% (CI±0.07%).
These results are shown in Table 2.
We were unable to calculate the incidence of other procedures, as they were not conducted at our hospital, and it is difficult to know the exact number of interventions carried out.
Discussion
This study includes 32 cases; to date, we have found no other paper compiling such a long series of iatrogenic SCI. The incidence of iatrogenic SCI in this study was 10.4%.
Bacher et al's22 study showed 21 patients with iatrogenia, exclusively following surgical procedures with an incidence of 0.69%. Our incidence of iatrogenia is much higher. First, our series include non-invasive procedures, representing 25% of the total, and second, the average age in Bacher et al's22 study is only 34.4, whereas the subjects in this paper have an average age of 56.2, which suggests that an older age could mean an iatrogenic risk factor. If we consider only non-invasive procedures, the average age is even higher, reaching 61.3. An older age is associated with an increase in vascular risk factors, which have been proven to be associated with iatrogenic risk.5
Another explanation for our high incidence is that, we are a reference unit for a large area of population and we see all SCI generated, either at our hospital or in other hospitals in our catchment. This may also be explained by the fact that in this study, we included both cauda equina and conus medullaris injuries. In the study by Podnar,23 the incidence of iatrogenia in this type of injuries was 0.6 for every million inhabitants.
Our study shows that iatrogenia is more frequent in females (59%) than in males (41%), although the differences are not significant. SCIs due to traumatism are more frequent in males, in an approximate proportion of 80%;24 in injuries of medical etiology, there are no gender differences in terms of incidence.25 In this regard, we should highlight that the most frequent cause leading to an iatrogenic event was subjective clinical manifestations of pain, paresthesia or sciatica, with a total of 14 out of 32 cases.
The pathology leading to an iatrogenic event varies; nonetheless, the most frequent is spinal channel stenosis, a total of 13 cases out of 32. It is worth noting the high risk, a surgical intervention entails in this pathology, for not only is there a mechanical factor of entrapment of neurological structures, but also a deficient irrigation of the area has a vital role.26
A total of 91% of the SCI received were incomplete, with a predominance of grade C of ASIA, which was statistically significant. Evolution of the injuries was positive, with a gain of 8.1 points on the ASIA motor scale at the time of discharge. In this regard, iatrogenic SCIs follow the same positive pattern as incomplete injuries.27
Regarding the incidence of iatrogenic SCI in each procedure, we found that surgical intervention of the spine was the most frequent cause of SCI with 20 out of 24 cases, of which vertebral arthrodesis and laminectomy were the most frequent invasive procedures. This result is logical and predictable, given the anatomical proximity of the spinal cord to the surgical area. The incidence collected at our hospital by spinal surgical procedures was: arthrodesis, 0.4%; laminectomy, 0.2%; vertebroplasty, 0.9%. In the study by Cramer et al.3 in a series of 11 817 patients, there was an incidence of neurological injuries in spinal interventions of 0.18%. When there is cervical myelopathy associated with cervical osteoarthritis, the possibility of post-surgical iatrogenia is high. Martín et al.5 found an incidence of 11.3%. As for the thoracic level, Ayhan et al.4 noted worsening on the ASIA scale of 7.4% of the patients.
Another long series compiled by Delank et al.28 includes an incidence of iatrogenia in scoliosis surgery of 0.55%. In our study, the incidence of SCI following scoliosis was one case, but we could not find the incidence as the patient was referred from another hospital and we do not know the total number of scoliosis interventions that were carried out. A limitation of this paper is the lack of information on other surgical procedures described as the cause of iatrogenia, as we lack all the data necessary to find the iatrogenic incidence.
Of the 24 patients intervened, who suffered SCI, only four were monitored with evoked potentials. Although false negatives have been described during monitoring of motor evoked potentials,29 follow-up of the corticospinal tract with these motor potentials and of the posterior cord with sensory-evoked potentials is currently a very useful tool to prevent iatrogenic medullary injury in high-risk surgeries.30, 31 In this regard, it would be recommendable to encourage this practice in spinal interventions and aortic surgery.
Outstanding for their high incidence are bronchial artery embolizations, which, with three cases, provide an incidence of 8.6%. According to the references checked, the prevalence of medullary ischemia secondary to bronchial artery embolizations is 1.4–6.5%.32, 33 This incidence decreases with supraselective catheterization, a good knowledge of spinal artery anatomy and if migration of the embolization fluid material is avoided.14
Non-invasive procedures amount to eight cases, or 25% of the total, with oral anticoagulants as the most frequent cause of SCI. Although the actual incidence in our environment is low, 0.05%, population sample is high, as they are widely used drugs. We have found no studies objectifying the incidence of iatrogenic SCI due to oral anticoagulation use. A weakness of our study is that whether patients treated with anticoagulants were well monitored is not known. We want to mention an SCI resulting from applying human chorionic gonadotropin-β in an infertility treatment, because it is very rare. Serour et al.34 described a series of 3500 patients with an incidence of 0.2% of thromboembolic events and 0.07% strokes due to its procoagulant effect, but no medullary infarction. We only found one case presented by Lin et al.,35 describing a lateral medullary syndrome following ovulation induction with recombinant HCG in a 36-year-old woman with no known prior risk factors.
It would be interesting to conduct prospective studies to find which are the iatrogenic SCI risk factors and prevent them.
Conclusions
In conclusion, in our study, iatrogenic SCI due to invasive or non-invasive interventions has a high incidence (10.4%) in our environment. These iatrogenic SCIs are basically incomplete and at the lumbar level. The increased life expectancy of the population entails a rise in the number of elderly patients with vascular risk, who undergo invasive interventions.
The highest risk surgical procedures are those involving spinal surgery and bronchial artery embolizations, the latter showing the highest risk in the series at 8.6%. It is essential to take this risk into account when establishing surgical indications, that the patient is duly informed and that during the intervention, the patient's motor and sensory potentials are monitored. The non-invasive intervention with more patients affected was the intake of anticoagulants, so we must insist the patient and the physician to be careful in using laboratory tests and drug interactions.
References
Starfield B . Is US health really the best in the world? JAMA 2002; 284: 483–484.
New PW, Jackson T . The costs and adverse events associated with hospitalization of patients with spinal cord injury in Victoria, Australia. Spine (Phila Pa 1976) 2010; 35: 796–802.
Cramer DE, Maher PC, Pettigrew DB, Kuntz IV C . Major neurologic deficit immediately after adult spinal surgery: incidence and etiology over 10 years at a single training institution. J Spinal Disord Tech 2009; 22: 565–570.
Ayhan S, Nelson C, Gok B, Petteys RJ, Wolinsky JP, Witham TF et al. Transthoracic surgical treatment for centrally located thoracic disc herniations presenting with myelopathy: a 5-year institutional experience. J Spinal Disord Tech 2010; 23: 79–88.
Martin R, Carda JR, Montiaga F, Pinto JI, Sanz F, Paternina B et al. [Cervical myelopathy: retrospective analysis of surgical results in 53 cases treated by anterior cervical discectomy and interbody fusion]. Neurocirugia (Astur) 2005; 16: 235–255.
Robaina-Padron FJ . [Controversies about instrumented surgery and pain relief in degenerative lumbar spine pain. Results of scientific evidence]. Neurocirugia (Astur) 2007; 18: 406–413.
Diab M, Smith AR, Kuklo TR . Neural complications in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2007; 32: 2759–2763.
Hirabayashi H, Ebara S, Takahashi J, Narasaki K, Takahara K, Murakami G et al. Surgery for thoracic myelopathy caused by ossification of the ligamentum flavum. Surg Neurol 2008; 69: 114–116; discussion 116.
Etz CD, Luehr M, Kari FA, Bodian CA, Smego D, Plestis KA et al. Paraplegia after extensive thoracic and thoracoabdominal aortic aneurysm repair: does critical spinal cord ischemia occur postoperatively? J Thorac Cardiovasc Surg 2008; 135: 324–330.
Biglioli P, Roberto M, Cannata A, Parolari A, Spirito R . Paraplegia after iatrogenic extrinsic spinal cord compression after descending thoracic aorta repair: case report and literature review. J Thorac Cardiovasc Surg 2002; 124: 407–410.
Iwabuchi S, Koike K, Okabe T, Tago S, Murakami T . Iatrogenic paraplegia caused by surgicel used for hemostasis during a thoracotomy: report of a case. Surg Today 1997; 27: 969–970.
Dogan S, Kocaeli H, Doygun M . Oxidised regenerated cellulose as a cause of paraplegia after thoracotomy: case report and review of the literature. Spinal Cord 2005; 43: 445–447.
Sietsma MS, Heerspink FO, Ploeg WT, Jutte PC, Veldhuizen AG . [Kyphoplasty as treatment for osteoporotic vertebral compression fractures: relatively safe, but still no evidence of functional improvement; a review of the literature]. Ned Tijdschr Geneeskd 2008; 152: 944–950.
de Gregorio MA, Medrano J, Laborda A, Higuera T . Hemoptysis workup before embolization: single-center experience with a 15-year period follow-up. Tech Vasc Interv Radiol 2007; 10: 270–273.
Kao MC, Tsai SK, Tsou MY, Lee HK, Guo WY, Hu JS . Paraplegia after delayed detection of inadvertent spinal cord injury during thoracic epidural catheterization in an anesthetized elderly patient. Anesth Analg 2004; 99: 580–583, table of contents.
Mjahed K, Alaoui SY, Salam S, Lhoucine B . Acute paraplegia and pulmonary edema after benzathine penicillin injection. Am J Emerg Med 2008; 26: 250.e1–250.e5.
Peuker E, Gronemeyer D . Rare but serious complications of acupuncture: traumatic lesions. Acupunct Med 2001; 19: 103–108.
Karabatsou K, Sinha A, Das K, Rainov NG . Nontraumatic spinal epidural hematoma associated with clopidogrel. Zentralbl Neurochir 2006; 67: 210–212.
Senelick RC, Norwood CW, Cohen GH . “Painless” spinal epidural hematoma during anticoagulant therapy. Neurology 1976; 26: 213–225.
van der Laken CJ, Lems WF, van Soesbergen RM, van der Sande JJ, Dijkmans BA . Paraplegia in a patient receiving anti-tumor necrosis factor therapy for rheumatoid arthritis: comment on the article by Mohan et al. Arthritis Rheum 2003; 48: 269–270.
Parke WW, Whalen JL . Phrenic paresis—a possible additional spinal cord dysfunction induced by neck manipulation in cervical spondylotic myelopathy (CSM): a report of two cases with anatomical and clinical considerations. Clin Anat 2001; 14: 173–178.
Bacher T, Schiltenwolf M, Niethard FU, Paeslack V . The risk of paraplegia through medical treatment. Spinal Cord 1999; 37: 172–182.
Podnar S . Epidemiology of cauda equina and conus medullaris lesions. Muscle Nerve 2007; 35: 529–531.
Jackson AB, Dijkers M, Devivo MJ, Poczatek RB . A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil 2004; 85: 1740–1748.
McKinley WO, Seel RT, Hardman JT . Nontraumatic spinal cord injury: incidence, epidemiology, and functional outcome. Arch Phys Med Rehabil 1999; 80: 619–623.
Djurasovic M, Glassman SD, Carreon LY, Dimar II JR . Contemporary management of symptomatic lumbar spinal stenosis. Orthop Clin North Am 2010; 41: 183–191.
Waters RL, Adkins RH, Yakura JS, Sie I . Motor and sensory recovery following incomplete paraplegia. Arch Phys Med Rehabil 1994; 75: 67–72.
Delank KS, Delank HW, Konig DP, Popken F, Furderer S, Eysel P . Iatrogenic paraplegia in spinal surgery. Arch Orthop Trauma Surg 2005; 125: 33–41.
Modi HN, Suh SW, Yang JH, Yoon JY . False-negative transcranial motor-evoked potentials during scoliosis surgery causing paralysis: a case report with literature review. Spine (Phila Pa 1976) 2009; 34: E896–E900.
Collado-Corona MA, de Leo-Vargas R, Sandoval-Sanchez V, Diaz-Hernandez A, Gutierrez-Sougarret BJ, Shkurovich-Bialik P . Neurophysiological monitoring in spinal cord surgery. Cir Cir 2009; 77: 385–390.
Tamaki T, Tsuji H, Inoue S, Kobayashi H . The prevention of iatrogenic spinal cord injury utilizing the evoked spinal cord potential. Int Orthop 1981; 4: 313–317.
Ramakantan R, Bandekar VG, Gandhi MS, Aulakh BG, Deshmukh HL . Massive hemoptysis due to pulmonary tuberculosis: control with bronchial artery embolization. Radiology 1996; 200: 691–694.
Mal H, Rullon I, Mellot F, Brugiere O, Sleiman C, Menu Y et al. Immediate and long-term results of bronchial artery embolization for life-threatening hemoptysis. Chest 1999; 115: 996–1001.
Serour GI, Aboulghar M, Mansour R, Sattar MA, Amin Y, Aboulghar H . Complications of medically assisted conception in 3,500 cycles. Fertil Steril 1998; 70: 638–642.
Lin HC, Chen MJ, Chou CH, Young YH . Lateral medullary syndrome in a woman after ovulation induction. Auris Nasus Larynx 2007; 34: 383–385.
Acknowledgements
We thank Drs María Delgado and Inmaculada Miguel for their disinterested collaboration, Dr Beatriz Salañer for helping us to find the records and Dr Enrique Viosca for reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Alcanyis-Alberola, M., Giner-Pascual, M., Salinas-Huertas, S. et al. Iatrogenic spinal cord injury: an observational study. Spinal Cord 49, 1188–1192 (2011). https://doi.org/10.1038/sc.2011.72
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.72
Keywords
This article is cited by
-
Neurological injury as a complication of spinal surgery: incidence, risk factors, and prognosis
Spinal Cord (2020)
-
Risk factors in iatrogenic spinal cord injury
Spinal Cord (2017)
-
International Spinal Cord Injury Data Sets for non-traumatic spinal cord injury
Spinal Cord (2014)