Abstract
Study design:
Cross-sectional comparison, control group.
Objectives:
To investigate the relationship between carotid arterial stiffness and circulating markers for cardiovascular disease (CVD) in spinal cord-injured (SCI) subjects compared with able-bodied (AB) individuals.
Setting:
University Research Laboratory, University of Louisville.
Methods:
SCI (n=14) and AB (n=13) subjects between 20–52 years of age were recruited to participate in the study. B-mode Doppler ultrasound was used to obtain carotid artery diameter measurements. Arterial stiffness was assessed via the stiffness index and distensibility coefficient. Markers of CVD risk were obtained by fasting blood draw.
Results:
Carotid arterial stiffness index (P=0.061) and distensibility coefficient (P=0.370) were not different between the SCI and AB groups. The SCI group had higher high-sensitivity C-reactive protein (hsCRP) (P=0.046), triglycerides (P=0.017), leptin (P=0.040) and visfatin (P<0.001) compared with the control group. Visfatin (r=0.559, P=0.047), hsCRP (r=0.633, P=0.037), insulin (r=0.637, P=0.019) and HOMA (r=0.614, P=0.026) significantly correlated with carotid arterial stiffness index in the SCI group.
Conclusion:
This study demonstrated that SCI subjects are at a high cardiovascular risk as indicated by elevated hsCRP levels. Elevations in hsCRP and visfatin may contribute to accelerated atherogenic processes in the SCI population.
Similar content being viewed by others
Introduction
Diseases of the circulatory system have emerged as the most common underlying and contributing cause of death in patients with chronic spinal cord injury (SCI).1 Many cardiovascular risk factors including hyperlipidemia and diabetes have been shown to be comparatively high among individuals with SCI.2, 3 Patients with chronic SCI have also been observed to have elevated serum concentrations of chronic inflammatory markers, such as interleukin-6 (IL-6) and C-reactive protein (CRP), relative to able-bodied control subjects.2 CRP is an extremely sensitive, acute-phase reactant produced in response to most forms of injury, infection and inflammation, and has been shown to be a predictor of vascular disease and a higher risk of cardiovascular events.4
Vascular diseases are often evidenced by endothelial dysfunction and central arterial stiffness.5 Stiffness of the carotid artery is associated with atherosclerosis at various sites throughout the arterial tree and increased cardiovascular mortality risk.5 Vascular damage is associated with metabolic disturbances as increased stiffness of the common carotid artery is seen with an increasing number of components of the metabolic syndrome.6 Additionally, circulating mediators of inflammation, such as CRP and IL-6, have been suggested to contribute to the pro-atherogenic mechanism of vascular insult resulting in stiffening of the arterial system.7, 8
The purpose of this study was to determine if vascular function was reduced in SCI patients compared with their non-disabled counterparts and, secondly, to determine if there was any relationship between markers for atherosclerosis and carotid arterial stiffness in SCI patients compared with their non-disabled counterparts.
Materials and methods
Subjects
Fourteen men (n=10) and women (n=4) with a non-progressive spinal cord injury above the T12 level were recruited from the Neuroscience Collaborative Center at Frazier Rehabilitation Hospital (Louisville, KY, USA). All SCI subjects underwent a physical therapy evaluation and screening by a research physician before inclusion in the study for assessment of American Spinal Injury Association classification. All SCI subjects had been injured for a minimum of 2 years and were non-ventilator dependent with an American Spinal Injury Association classification of A–C. Subjects with a history of smoking, diabetes, cardiovascular disease (CVD) or hypercholesterolemia were excluded from the study. SCI subjects were free of urinary tract infections and pressure ulcers. SCI subjects were matched to a non-disabled, ambulatory control subject (n=13; men=9 and women=4) based on age, height, body weight, gender and race. Each group was composed primarily of Caucasians, with one African American subject. All subjects refrained from exercise for 24 h before testing. Several subjects were on medication for pain, bowel/bladder function, allergies and antibiotics that were not restricted during testing. Before the study, all subjects signed an informed consent approved by the Institutional Review Board of the University of Louisville.
Procedures
Subjects arrived at the laboratory for testing in the morning following a 12-h fast. An automated blood pressure cuff (HEM-907 XL, Omron, Vernon Hills, IL, USA) was placed on their left arm and a cuff to be used for the flow-mediated dilation (FMD) test was placed on their right arm. Once the subject was prepped they rested quietly in a quiet, dark room with a temperature of 22 °C for 10 min to allow blood pressure to stabilize. After stabilization baseline blood pressure measurements were taken, followed by the FMD test, carotid arterial testing and a blood draw.
Brachial artery FMD was performed as described previously.9 Post-ischemic cumulative shear rate was expressed as the area under the curve for the mean wall shear rate over time from the cuff release until peak diameter,10 integrated with the use of GraphPad Prism version 4.03 for windows (GraphPad Software, San Diego, CA, USA). The following equations were used to determine the relative FMD, mean wall shear rate and FMD normalized, where d is the diameter:



Carotid arterial ultrasound images were obtained in the left carotid arteries, which were imaged approximately 2–3 cm proximal to the carotid bulb using B-mode ultrasound with a 12.5-MHz linear-phase array ultrasound transducer for 60 s. A digital video was used to capture all data from the ultrasound and was later analyzed using the custom LabView program for the determination of diameter changes. Blood pressure was measured in the left brachial artery immediately before and immediately after ultrasound measurements. An average of these blood pressures was used for all calculations. Twenty consecutive seconds of systolic and diastolic diameters were analyzed from each video for determination of the stiffness index (β) and distensibility coefficient (DC). The stiffness index (β) and distensibility coefficient were calculated as measures of carotid arterial stiffness and distensibility, respectively, by the following equations:

where Ps is the average systolic pressure, Pd is the average diastolic pressure, Δd is the difference between the average systolic and diastolic diameters, D is the average end systolic diameter, and Δp is the average pulse pressure.
Following ultrasound imaging, approximately 12 ml of blood was collected from an antecubital vein in glass-evacuated blood collection tubes (Becton Dickinson, Plymouth, UK). Blood samples were allowed to clot and were centrifuged (Fisher Scientific, Model 228) at 3300 r.p.m. for 15 min. The separated serum was then transferred to 0.5-ml vials and stored at −80 °C until analyzed.
Total cholesterol (TC), triglyceride (TG) and glucose concentrations were measured using enzymatic tests (VITROS Chemistry Systems, Johnson & Johnson Gateway, Piscataway, NJ, USA). High-density lipoprotein-cholesterol (HDL-C) was determined after selective precipitation of the very-low-density lipoprotein-cholesterol (VLDL-C) and low-density lipoprotein-cholesterol (LDL-C). LDL-C concentrations were calculated by the Friedewald equation as follows: LDL-C=TC−HDL-C−(TG/5). Serum insulin concentrations were measured via electrochemiluminescence immunoassay (Modular Analytics E-170 Analyzer, Roche Diagnostics, Indianapolis, IN, USA). Serum high-sensitivity C-reactive protein (hsCRP) was measured via a particle-enhanced turbidimetric assay (COBRAS INTEGRA, Roche Diagnostics, Indianapolis, IN, USA). CRP concentrations greater than 1.0 mg dl−1 indicate the presence of acute infection or inflammation rather than chronic low-grade inflammation associated with atherosclerosis.11 Two SCI subjects had hsCRP values >1.0 mg dl−1. These two hsCRP values were excluded from the correlational data analysis in the present study. Adiponectin and visfatin were measured using a Bio-Plex Pro Human Diabetes 12-+2-plex panel (Bio-Rad Lab, Hercules, CA, USA) and determined using a Luminex 100 IS system (Luminex Corp, Austin, TX, USA). Data were analyzed using standard curves fitted by four-parameter regression according to the manufacturer's instructions. Serum asymmetric dimethylarginine (ADMA) was measured using an enzyme-linked immunosorbant assay (DLD Diagnostika GmbH, Hamburg, Germany). The homeostasis model of insulin resistance (HOMA-IR) was calculated with the following equation:

where FI is the fasting insulin concentration and FG is the fasting glucose concentration in the units indicated by the subscript.
Statistical analyses
Statistical Package for Social Sciences (SPSS version 17.0) was used for all statistical analyses. The limits of statistical significance were P<0.05. Independent-samples t-tests were used to determine differences between the SCI and able-bodied (AB) groups. Mann–Whitney rank-sum U tests were used in place of the independent-samples t-tests when the Levene's test for equality of variances was significant. All correlational analyses were executed with the Pearson product-moment correlational analysis.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Characteristics of the individual SCI subjects can be found in Table 1. The average duration of injury of the SCI individuals was 11±9 years. There were no significant differences between groups on any baseline measures, indicating that the groups were well matched (Table 2). Blood pressure was not significantly different between groups (Table 2) and there were no differences between groups on any of the vascular measurements (Table 3). Between-group differences in vascular measurements were non-significant, with β-stiffness index approaching statistical significance (P=0.061).
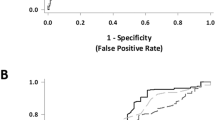
Blood samples were analyzed for indicators of cardiovascular risk factors (Table 4). Triglycerides (P=0.017), hsCRP (P=0.046), visfatin (P<0.001) and leptin (P=0.040) were significantly elevated in the SCI group compared with the AB group. hsCRP (r=0.633, P=0.037) (Figure 1), visfatin (r=0.559, P=0.047) (Figure 2), fasting insulin (r=0.637, P=0.019) and HOMA (r=0.614, P=0.026) were significantly correlated to β-stiffness index in the SCI group (Table 5). β-Stiffness index was also significantly correlated to age in both groups (SCI: r=0.614, P=0.025 and AB: r=0.556, P=0.048) and to duration of injury in the SCI group (r=0.697, P=0.008).
Discussion
The main findings of this study were that hsCRP and visfatin were significantly elevated in the SCI group compared with the AB group. Furthermore, both hsCRP and visfatin were significantly correlated with the carotid arterial stiffness index in the SCI group. Our hsCRP data indicate that the SCI group in this study is at high risk for CVD as established by the American Heart Association.12 Numerous studies have demonstrated associations of elevated hsCRP levels with cardiovascular risk factors such as BMI, insulin resistance, hypertension, endothelial dysfunction and dislipidemia, as well as a linear relationship between circulating CRP levels and CVD risk.8
Large artery stiffening involves structural changes, including fragmentation and degradation of elastin, increases in collagen and thickening of the vessel wall, all of which are believed to be important mechanisms in mediating arterial stiffness with aging.6 These mechanisms certainly influence arterial stiffness in SCI and AB subjects alike; however, the elevated hsCRP levels in SCI individuals indicate that the portion of arterial stiffening that is driven by inflammation may be occurring at an increased rate or at an earlier age in the SCI individual. Thus, the correlation between hsCRP and carotid arterial stiffness in the SCI group and lack of such correlation in the AB group suggests that hsCRP may have a greater impact on the central vasculature in the SCI group than the AB group. The influence of CRP on arterial stiffness has been suggestive of disease progression, as CRP has been correlated with carotid arterial stiffness in patients with type 2 diabetes mellitus.13 CRP has also been correlated with early asymptomatic arteriosclerosis demonstrated by increased intima–media thickness.13 CRP has several atherogenic properties, as it has been shown to induce the expression of endothelial adhesion proteins vascular cell adhesion molecule, intercellular adhesion molecule and E-selectin.8
Our findings from this study support previous research in which circulating CRP concentrations were elevated in an SCI group compared with an AB control group.2, 3, 14 Wang et al.2 suggested that their SCI group was at increased risk for atherogenesis due to chronic endothelial activation as evidenced by elevated endothelin-1 and vascular cell adhesion molecule levels, and further demonstrated an association between CRP levels and carotid intima–media thickness in SCI.3 Additionally, Gibson et al.15 observed elevated waist circumference, TGs, HOMA and decreased HDL-C in SCI subjects with CRP values indicative of increased CVD risk compared with SCI subjects with normal CRP levels. Thus, the elevation in hsCRP in the SCI population may contribute to increased atherogenesis and an elevated cardiovascular risk.
In the SCI group, visfatin was also significantly correlated with β-stiffness index. The mechanism by which visfatin affects the vasculature is unclear as it may be related to disruption in the insulin mediated pathways of endothelial function5, 16 or it may increase the inflammatory processes.17 The precise physiological roles of visfatin remain to be definitively elucidated; however, it has been shown to be elevated in type 2 diabetic patients16 and is believed to be associated with the total amount of visceral adipose tissue.18 The waist circumference and waist-to-hip ratio of the SCI group was not different from those of the AB group in the present study, however, visceral fat area has shown to be elevated in SCI in the absence of elevated BMI or waist circumference.19
Although our study is novel and does extend the literature regarding arterial stiffness and low-grade inflammation in an SCI population, our study is not without limitations. One limitation of this study was the small sample size and the heterogeneity of the sample. Owing to the low number of subjects, it was necessary to include males and females, as well as a wide range of age and duration of injury of subjects in order to have adequate power to establish trends within each group. A second limitation is that our analyses are based on a single measurement of fasting serum concentrations, which may not reflect the relationship over time. Additionally, correlational analysis does not infer causation and limits our ability to make conclusions on the physiological roles of the blood markers that were investigated within the SCI population. Nevertheless, our study does extend the data regarding inflammation and vascular function in an SCI population.
Despite our small sample size and heterogeneity, the hsCRP values in our SCI and AB groups were similar to those of previous works with SCI patients2, 14, 15 and with obese and insulin-resistant groups in a much larger study.20 Despite the exclusion of hsCRP values indicative of infection from data analysis in the present study, it remains possible that patients with chronic SCI could demonstrate elevated hsCRP due to bruising, bladder management techniques and minor infections. However, given that our SCI group demonstrated hsCRP levels similar to other at-risk groups20 and in conjunction demonstrated elevated TG, leptin and visfatin levels, we feel it is likely that the SCI group has an accelerated development of CVD and the metabolic syndrome.
In conclusion, we found that apparently healthy SCI individuals had an elevated hsCRP indicating enhanced inflammation, which puts them at high risk of CVD. Furthermore, we found that hsCRP was significantly correlated to carotid arterial stiffness in the SCI population, which may contribute to atherogenesis. Visfatin was significantly correlated with carotid arterial stiffness in the SCI group as well, indicating that it may be a surrogate marker of inflammation or vascular insult. The precise physiological role of visfatin should continue to be investigated, particularly in the SCI population.
References
Myers J, Lee M, Kiratli J . Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation and management. Am J Phys Med Rehabil 2007; 86: 142–152.
Wang TD, Wang YH, Huang TS, Su TC, Pan SL, Chen SY . Circulating levels of markers of inflammation and endothelial activation are increased in men with chronic spinal cord injury. J Formos Med Assoc 2007; 106: 919–928.
Wang YH, Chen SY, Wang TD, Hwang BS, Huang TS, Su TC . The relationships among serum glucose, albumin concentrations and carotid artherosclerosis in men with spinal cord injury. Atherosclerosis 2009; 206: 528–534.
Koenig W, Sund M, Frohlich M, Fischer H-G, Lowel H, Doring A et al. C-reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: results from the MONICA (monitoring trends and determinants in cardiovascular disease) Augsburg cohort study, 1984 to 1992. Circulation 1999; 99: 237–242.
Hadi HA, Carr CS, Al Suwaidi J . Endothelial dysfunction: cardiovascular risk factors, therapy, and outcome. Vasc Health Risk Manag 2005; 1: 183–198.
Li S, Chen W, Srinivasan SR, Berenson GS . Influence of metabolic syndrome on arterial stiffness and its age-related change in young adults: the Bogalusa Heart Study. Atherosclerosis 2005; 180: 349–354.
Araki T, Emoto M, Yokoyama H, Maeno T, Hatsuda S, Mori K et al. The association of plasma adiponectin level with carotid arterial stiffness. Metabolism 2006; 55: 587–592.
Berg AH, Scherer PE . Adipose tissue, inflammation, and cardiovascular disease. Circ Res 2005; 96: 939–949.
Olive JL, Ballard KD, Miller JJ, Milliner BA . Metabolic rate and vascular function are reduced in women with a family history of type 2 diabetes mellitus. Metabolism 2008; 57: 831–837.
Nishiyama SK, Wray DW, Berkstresser K, Ramaswamy M, Richardson RS . Limb-specific differences in flow-mediated dilation: the role of shear rate. J Appl Physiol 2007; 103: 843–851.
Myers GL, Rifai N, Tracy RP, Roberts WL, Alexander RW, Biasucci LM et al. CDC/AHA workshop on markers of inflammation and cardiovascular disease: application to clinical and public health practice: report from the laboratory science discussion group. Circulation 2004; 110: e545–e549.
Pearson TA, Mansah GA, Alexander RW, Anderson JL, Cannon III RO, Criqui M et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003; 107: 499–511.
Diamant M, Lamb HJ, van de Ree MA, Endert EL, Groeneveld Y, Bots ML et al. The association between abdominal visceral fat and carotid stiffness is mediated by circulating inflammatory markers in uncomplicated type 2 diabetes. J Clin End Met 2005; 90: 1495–1501.
Finnie AK, Buchholz AC, Martin Ginis KA . Current coronary heart disease risk assessment tools may underestimate risk in community-dwelling persons with chronic spinal cord injury. Spinal Cord 2008; 46: 608–615.
Gibson AE, Buchholz AC, Martin Ginis KA . C-reactive protein in adults with chronic spinal cord injury: increased chronic inflammation in tetraplegia vs. paraplegia. Spinal Cord 2008; 46: 616–621.
Chen M-P, Chung F-M, Chang D-M, Tsai JC-R, Huang H-F, Shin S-J et al. Elevated plasma level of visfatin/Pre-B cell colony-enhancing factor in patients with type 2 diabetes mellitus. J Clin End Met 2006; 91: 295–299.
Oki K, Yamane K, Kamei N, Nojima H, Kohno N . Circulating visfatin level is correlated with inflammation, but not with insulin resistance. Clin Endocrinol 2007; 67: 796–800.
Sandeep S, Velmurugan K, Deepa R, Mohan V . Serum visfatin in relation to visceral fat, obesity, and type 2 diabetes mellitus in Asian Indians. Metabolism 2007; 56: 565–570.
Maruyama Y, Mizuguchi M, Yaginuma T, Kusaka M, Yoshida H, Yokoyama K et al. Serum leptin, abdominal obesity and the metabolic syndrome in individuals with chronic spinal cord injury. Spinal Cord 2008; 46: 494–499.
Ridker PM, Buring JE, Cook NR, Rifai N . C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Circulation 2003; 107: 391–397.
Acknowledgements
We thank all the study participants for participating in the study. We also thank Dr Susan Harkema and the Frazier Rehabilitation Staff for their assistance in subject recruitment and ASIA classification of the SCI subjects. Drs Robert Topp and Vinay Mauder should be thanked for their assistance with phlebotomy. We also thank Drs James Miller and Shirish Barve for their assistance in blood analyses.
Sponsorship: Research office of the University of Louisville.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
La Favor, J., Hollis, B., Mokshagundam, S. et al. Serum hsCRP and visfatin are elevated and correlate to carotid arterial stiffness in spinal cord-injured subjects. Spinal Cord 49, 961–966 (2011). https://doi.org/10.1038/sc.2011.56
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.56
Keywords
This article is cited by
-
Endocrinological and inflammatory markers in individuals with spinal cord injury: A systematic review and meta-analysis
Reviews in Endocrine and Metabolic Disorders (2022)