Abstract
Study design:
Clinical intervention study.
Objective:
Arm hand skilled performance (AHSP) has a major role in the rehabilitation of persons with cervical spinal cord injury (C-SCI). A task-oriented client-centered upper extremity skilled performance-training (ToCUEST) module was developed. The present study aims to evaluate effects of ToCUEST on specific and general AHSP in C-SCI, during and after rehabilitation.
Setting:
Adelante Rehabilitation Centre (The Netherlands).
Methods:
C-SCI persons, either during or after rehabilitation, completed the ToCUEST training; a control group of patients during rehabilitation received standard rehabilitation. The training module was focused on patient's individual needs, combining principles of motor learning and training physiology. Three self-selected goals were trained 3 days per week, in three sessions of 30 min per day for 8 weeks. Measures were taken at 3 months after the start of the active rehabilitation (T0), before training (T1), after training (T2), at follow-up (3 months post-training; T3) and at discharge.
Results:
For both ToCUEST groups during (n=11) and after (n=12) rehabilitation, an improvement (P<0.001) on specific AHSP (using the Goal Attainment Scale and the Canadian Occupational Performance Measure (satisfaction and performance)) was found between T1–T2 and T1–T3. Also an improvement (P<0.02) in general AHSP (using the Van Lieshout Test, the QIF and the motor FIM) was found in the total ToCUEST group between T1–T2 and T1–T3. No significant difference in improvement of general AHSP was found between the ToCUEST rehab and control group.
Conclusion:
The ToCUEST module leads to improvement in AHSP, not only persons with C-SCI during rehabilitation, but also after finishing rehabilitation. These effects remain at follow-up.
Similar content being viewed by others
Introduction
In persons with a cervical spinal cord injury (C-SCI), improving arm and hand performance has a major role in rehabilitation and may lead to large improvement in self-management and quality of life.1 Although there are limited number of studies, a review on motor training programs for arm and hand functioning demonstrated the benefits of training programs and the importance of the specificity of the training. A client-centered treatment might offer a solution to the wide range of upper extremity activities and the importance of the specificity of the training.2 On the basis of (a) aforementioned findings, (b) the lack of theoretical framework on client-centered care and the need to provide guidelines how to apply client-centered care in daily practice and (c) the fact that tetraplegic patients encounter different needs throughout their lives, which may be dealt with in separate therapy modules after patients have been discharged, Spooren et al.3 developed a task-oriented client-centered upper extremity skilled performance training (ToCUEST) module for persons with tetraplegia. The ToCUEST module, described by Spooren et al.3 combines three elements, which have been advocated in rehabilitation, that is, individual goal setting, client-centeredness and task-oriented training, into a common framework.3, 4, 5 To date, their combined use and efficacy have, to the authors’ knowledge, not yet been reported in the SCI population. It is hypothesized that the ToCUEST module, focusing on specific needs, leads to an improvement on specific skills. Furthermore, it is assumed that ToCUEST, relative to therapy as usual, does not necessarily lead to more improvement in general arm hand skilled performance (AHSP). As to the latter, it is expected that similar results will be obtained.
The aim of the present study is to evaluate the effects of ToCUEST on AHSP in tetraplegic patients. First, the study aims to assess whether ToCUEST leads to an improvement of specific skills not only in persons during their rehabilitation, but also in persons who have finished their rehabilitation. Second, it aims to assess whether ToCUEST leads to general improvement in AHSP during and after rehabilitation. Third, the present study aims to compare improvement in general AHSP in both C-SCI persons receiving ToCUEST and in C-SCI persons receiving standard training.
Methods
Subjects
Patients with C-SCI (either a motor complete or motor incomplete lesion), who were either actively receiving rehabilitation (active-rehab group) or who had finished their active rehabilitation (post-rehab group), were invited to participate in this clinical intervention study. They were recruited from the SCI Unit of Adelante Rehabilitation Centre. Inclusion criteria were: diagnosed with C-SCI (including T1 lesion levels), age between 18 and 70 years and problems with AHSP (identified using the Canadian Occupational Performance Measure (COPM)). Exclusion criteria were: co-morbidity concerning neurological, orthopedic or rheumatologic diseases that might strongly interfere with ADL functioning and AHSP, and inability to take part in upper extremity measurements. A control group of patients during their rehabilitation were monitored prospectively during a prospective cohort study, ‘Physical Strain, Work Capacity and Mechanisms of Restoration of Mobility in the Rehabilitation of SCI’ (www.SCIONN.nl). Data of the latter persons were captured in a large database. The persons identified from this database were selected, matching every participating person by lesion completeness and motor lesion level according to the Neurological Classification of SCI, Upper Extremity Motor Score,6 age and gender, respectively (pair-matching). All subjects gave their informed consent. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Intervention
Patients receiving ToCUEST chose two goals out of the five personally most problematic activities identified using the COPM.7 Additionally, they chose one activity from the Van Lieshout test (VLT) items8, 9 to train on. These three self-selected goals were trained 3 days per week, in three sessions of 30 min per day for 8 weeks. The training program started with a task analysis and was based on principles of training physiology and motor learning. A detailed description of the ToCUEST module is given in an earlier paper by the authors.3 All participants were trained by a set team of specialized occupational therapists and physiotherapists. Persons in the active-rehab group received the specific training instead of a standard self-exercise program or ‘hand-function-group’ program. This way, the total rehabilitation load for the participants was not changed. For the post-rehab group, any maintenance physiotherapy focusing on the upper extremity was replaced by the ToCUEST program. Patients in the control group received therapy as usual, consisting of a comprehensive package of care according to lesion level and lesion completeness.
Measurements
Tests to measure both specific and generic AHSP (basic and complex activities) were used.
Specific activities
GAS: Goal Attainment Scale is used to objectively measure the effect of therapy on individual treatment goals and has shown to be feasible, reliable, valid and responsive to change.10, 11
COPM: is used to measure patient's perception of performance and satisfaction of the individual tasks on a scale ranging from 0–10. The reliability and validity of the COPM have been demonstrated in several populations and treatment settings.7
Generic AHSP
Van Lieshout test assesses the actual performance of arm hand skills at the level of basic activities. In the present study, the short form is used. In analysis A, the sum score of both hands was taken, resulting in a maximal attainable score of 100 and in analysis B, the score of the best hand was used with a maximal attainable score of 50. The criterion validity, reliability, the internal consistency and the responsiveness of the VLT Short Form were found to be good.8, 9
FIMmot: The motor score of the Functional Independence Measure was used, consisting of 13 items with an attainable maximal score of 91.12
QIF: In the current study, the short-form Quadriplegia Index of Function with a maximal total score of 24 was used.13
Both FIM and QIF have adequate psychometric properties.8, 9, 12, 13
Measurement moments were defined relative to specific moments of the rehabilitation. Measures of both specific and generic activities were taken at T1 (the start of specific training program (for the rehab group, this was at 5 months after the start of the active rehabilitation, in which the latter was defined as the moment that patients were able to sit for three consecutive hours)), at T2 (the end of the specific training program) and at T3 (3 months after finishing the training). To compare the data with the control group, general AHSP outcome measures were also taken at T0 (at 3 months after the start of the active rehabilitation) and at discharge.
All measurements were done by a trained team of therapists. Data were collected immediately after the measurements to ensure blinding of previous scores. The participants’ performance on the self-selected skills was also recorded on videotapes to allow for independent observers to blindly score the GAS.
Data analysis
A power analysis indicated that 10 persons per group were needed (given a mean improvement on the VLT of four points and a common s.d. of 13 (as observed between T0 and discharge in the ‘Koepel’-project data), an alpha of 0.01, a power of 90% and a loss to follow-up of 10%). Statistical analyses included Friedman two-way analysis of variance by rank test and Wilcoxon signed-rank test for multiple comparison within groups. Between-group comparison included the Mann–Whitney U-tests. Alpha was set at 0.05. Multiple comparisons included the Bonferroni correction.
A sensitivity analysis was performed in order to assess the contribution a specific item that was trained (for example, a VLT-item chosen), might have on the generic outcome. The latter was done using a univariate analysis,14 that is, varying the trained item by 10% (+10% and −10%) at T2 and T3. In all analyses, the intention-to-treat principle was used.
Results
Subjects
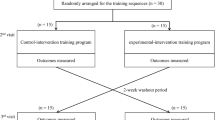
Figure 1 depicts a flowchart of the different stages of the trial.
Baseline characteristics of the patient groups for both analyses are shown in Table 1.
On the basis of the patients’ therapy booklets and on therapy databases, therapy compliance was calculated to be 90%. No adverse effects of the training were reported.
Outcome measures
Only 3.6% of the primary outcome measurements were missing. Tables 2 and 3 present the mean, s.d. and median for the different groups and measurement moments.
Analysis A: ToCUEST
Specific activities
As shown in Table 2, after training, all groups demonstrated an improvement on the COPM performance, COPM satisfaction and GAS. Improvement generally remained at follow-up. This was corroborated statistically for all specific outcome measures over the three measurement moments (P<0.001) and over the two time intervals of interest (T1–T2 and T1–T3; P<0.015) in all groups.
Generic AHSP
An improvement on the VLT, the FIM and the QIF was observed between T1 and T2, and between T1and T3. This improvement was statistically significant for all generic outcome measures across the three measurement moments (P<0.04) and in both intervals (T1–T2 and T1–T3; P<0.02) in the total group, but not in all the different subgroups, as can be observed in Table 2.
The univariate sensitivity analysis showed no difference in results, that is, varying the trained item by ±10% had no effect on the significance level.
Analysis B: ToCUEST versus control group
Table 3 shows the improvement on the FIM, the QIF and the VLT between T0 (3 months after the start of the active rehabilitation) and discharge in both groups. In the control group, the improvement was statistically significant for the QIF and the FIMmot (P<0.03). The training group additionally revealed a statistically significant improvement on the VLT (P<0.04). The improvement in the training group seems somewhat more, that is, the mean delta values of the VLT (the average difference of the VLT between T0 and discharge) were 2.5 in the control group and 5.0 in the ToCUEST group. Also the mean delta values of the QIF were three and four for the control and the ToCUEST group, respectively. However, no statistically significant difference between the average delta values of the VLT, the QIF and the FIMmot between the control and the ToCUEST group was found.
Discussion
The present study aimed to evaluate the effects of ToCUEST on AHSP in tetraplegic patients. In general, it can be concluded that: (a) ToCUEST leads to an improvement in specific upper extremity skills not only in persons with C-SCI during rehabilitation, but also in persons who have finished their rehabilitation, (b) ToCUEST leads to general improvement of AHSP in persons with C-SCI, (3) training results (both specific and generic) remain at follow-up. However, no significant difference in the amount of improvement of general AHSP between the ToCUEST group and the control group was found.
It was remarkable that a significant improvement on specific activities was seen not only in persons during their rehabilitation, but also in persons who finished their active rehabilitation.
To date, most studies were unable to demonstrate considerable functional changes after discharge.15, 16 Yarkony et al.15 reported that functional improvement occurs most rapidly during inpatient rehabilitation and attributed this effect to the combination of neurological recovery, intensity of the training and a multidisciplinary approach In the present study, the effect of neurological recovery in the post-rehab group was thought to be limited. By demonstrating important changes after discharge, the present study suggests that patients who have finished their rehabilitation may have residual potential to learn other activities. Future research should assess the neurophysiologic processes behind the training strategies. Furthermore, it was observed that patients in the post-rehab group had changing needs. They reported different needs after rehabilitation than before discharge. The present study demonstrates that ToCUEST may accommodate the demand to train on the changing needs throughout patients’ lives.5, 17 Additionally, ToCUEST is offered as a training module, thus facilitating re-admission for a limited amount of time to train on specific needs.
The fact that results remain at follow-up may be attributed to different factors. First, patients who are trained on their individual needs are more motivated.18, 19 This leads to closer adherence to the training, to more effort of patients to use the skills in daily life and to maintain these activities after finishing the training, inducing an improved rehabilitation outcome.19, 20 Second, in ToCUEST, specific goals were formulated, which were analyzed and trained, combining principles of motor learning with principles of training physiology.3 The importance of a task-oriented intensive training was emphasized in ToCUEST, as well as the shift from a multi- to an inter- or trans-disciplinary approach. The latter resulted in a common rehab approach, merging the expertise of both physical and occupational therapists. Third, although the training duration of 8 weeks was in some cases considered (too) long, it may be crucial to maintain the level of the positive results at follow-up which is in accordance with general training principles and principles of motor learning (over-learning principle). Future research focusing on varying the duration of the training may provide more insight in this matter.
An improvement in general AHSP was found in all C-SCI patients and based on the results of the sensitivity analysis, it was ruled out that the improvement was attributed solely to the improvement of the trained items. For example, if eating was trained, the generalized improvement was not attributable to the increase on the feeding item of the FIM alone. In short, a generalized improvement of AHSP on tasks that were not trained, may have taken place due to the ToCUEST training. However, more in depth research is needed to further corroborate our data on this issue.
No statistically significant difference in improvement of general AHSP between the ToCUEST and the control group was found. However, from clinical point of view, it would suffice that ToCUEST results in at least an equal level of general AHSP relative to the therapy as usual. On the basis of the findings in the study, it is expected that the ToCUEST training may lead to a reduction of inpatient stay (time between T0 and discharge was 28 weeks in the ToCUEST group and 41 weeks in the control group). A shortening of the inpatient stay may lead to improved patient's satisfaction and increased quality of life. A cost-effectiveness analysis is planned to shed light on the latter issues.
The present study has some methodological limitations.
Despite the fact that the recruitment period was 2.5 years, the number of participants was small. The limiting factors regarding participation are shown in Figure 1. Many patients with a lesion level at C8 had no major problems regarding AHSP, indicating that ToCUEST is mostly suitable in persons with lesion level of C7 or higher. Owing to the limited number of participants, performing a randomized controlled trial was not realistic. Furthermore, no specific outcome measurements (like the COPM and the GAS) were taken in the control group. The Medical Ethics Committee decided that it was not ethical to first ask patients’ training needs and then tell them not to train on these needs. As to blinding, assessors were not blinded for intervention, except for the GAS-score. However, they were blinded regarding previous results. Finally, to measure improvement on the VLT, measuring both the hands gives more information than measuring the best hand only, because in most cases the worst affected hand is trained. However, for analysis B, only the best hand was measured, often resulting in a ceiling effect on the VLT outcome of best hand.
The present study has demonstrated, despite some limitations, that the ToCUEST training module, which combines three important elements, that is, individual goal setting, client-centeredness and task-oriented training into a common framework, is feasible and beneficial in improving specific AHSP in C-SCI. Future research should aim for the ToCUEST module to be evaluated in a randomized controlled trial, involving more patients and to assess for cost-effectiveness.
References
Snoek GJ, MJ IJ, Hermens HJ, Maxwell D, Biering-Sorensen F . Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004; 42: 526–532.
Spooren AI, Janssen-Potten YJ, Kerckhofs E, Seelen HA . Outcome of motor training programmes on arm and hand functioning in patients with cervical spinal cord injury according to different levels of the ICF: a systematic review. J Rehabil Med 2009; 41: 497–505.
Spooren AIF, Janssen-Potten YJM, Kerckhofs E, Bongers HMH, Seelen HAM . ToCUEST: a task-oriented client-centered training module to improve upper extremity skilled performance in cervical spinal cord-injured persons. Spinal Cord 2011; 49: 1042–1048.
Wade DT . Goal setting in rehabilitation: an overview of what, why and how. Clin Rehabil 2009; 23: 291–295.
Cott CA . Client-centred rehabilitation: client perspectives. Disabil Rehabil 2004; 26: 1411–1422.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 (Suppl 1) (Spring) S50–S56.
Donnelly C, Eng JJ, Hall J, Alford L, Giachino R, Norton K et al. Client-centred assessment and the identification of meaningful treatment goals for individuals with a spinal cord injury. Spinal Cord 2004; 42: 302–307.
Spooren AI, Janssen-Potten YJ, Post MW, Kerckhofs E, Nene A, Seelen HA . Measuring change in arm hand skilled performance in persons with a cervical spinal cord injury: responsiveness of the Van Lieshout Test. Spinal Cord 2006; 44: 772–779.
Post MW, Van Lieshout G, Seelen HA, Snoek GJ, Ijzerman MJ, Pons C . Measurement properties of the short version of the Van Lieshout test for arm/hand function of persons with tetraplegia after spinal cord injury. Spinal Cord 2006; 44: 763–771.
Hurn J, Kneebone I, Cropley M . Goal setting as an outcome measure: a systematic review. Clin Rehabil 2006; 20: 756–772.
Bravo G, Dubois MF, Roy PM . Improving the quality of residential care using goal attainment scaling. J Am Med Dir Assoc 2005; 6: 173–180.
Hall KM, Cohen ME, Wright J, Call M, Werner P . Characteristics of the functional independence measure in traumatic spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1471–1476.
Marino RJ, Goin JE . Development of a short-form Quadriplegia Index of Function scale. Spinal Cord 1999; 37: 289–296.
Drummond MF, O'Brien B, Stoddart GL, Torance GW . Methods for the Economic Evaluation of Health care Programmes. Oxford University Press: New York, 1997.
Yarkony GM, Roth EJ, Heinemann AW, Lovell L, Wu YC . Functional skills after spinal cord injury rehabilitation: three-year longitudinal follow-up. Arch Phys Med Rehabil 1988; 69: 111–114.
Spooren AIF, Janssen-Potten YJM, Snoek GJ, Ijzerman MJ, Kerckhofs E, Seelen HAM . Rehabilitation outcome of upper extremity skilled performance in persons with cervical spinal cord injuries. J Rehabil Med 2008; 40: 637–644.
Kennedy P, Sherlock O, McClelland M, Short D, Royle J, Wilson CM . A multi-centre study of the community needs of people with spinal cord injuries: the first 18 months. Spinal Cord 2010; 48: 15–20.
Duff J, Evans MJ, Kennedy P . Goal planning: a retrospective audit of rehabilitation process and outcome. Clin Rehabil 2004; 18: 275–286.
Siegert RJ, McPherson KM, Taylor WJ . Toward a cognitive-affective model of goal-setting in rehabilitation: is self-regulation theory a key step? Disabil Rehabil 2004; 26: 1175–1183.
Wressle E, Eeg-Olofsson AM, Marcusson J, Henriksson C . Improved client participation in the rehabilitation process using a client-centered goal formulation structure. J Rehabil Med 2002; 34: 5–11.
Acknowledgements
We thank all medical and paramedical staff of the Spinal Cord Injury Unit of Adelante Rehabilitation Centre for their kind co-operation in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Spooren, A., Janssen-Potten, Y., Kerckhofs, E. et al. Evaluation of a task-oriented client-centered upper extremity skilled performance training module in persons with tetraplegia. Spinal Cord 49, 1049–1054 (2011). https://doi.org/10.1038/sc.2011.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.54
Keywords
This article is cited by
-
Innovative haptic-based system for upper limb rehabilitation in visually impaired individuals: a multilayer approach
Multimedia Tools and Applications (2023)
-
Early and intensive motor training to enhance neurological recovery in people with spinal cord injury: trial protocol
Spinal Cord (2023)
-
Efficacy of a technology-based client-centred training system in neurological rehabilitation: a randomised controlled trial
Journal of NeuroEngineering and Rehabilitation (2021)
-
The impact of task-oriented client-centered training on individuals with spinal cord injury in the community
Spinal Cord (2016)
-
Robot-assisted task-oriented upper extremity skill training in cervical spinal cord injury: a feasibility study
Spinal Cord (2015)