Abstract
Study design:
Cross-sectional survey; secondary analysis of existing data by linear regression analysis between spasticity and quality of life.
Objective:
To identify the relationship between spasticity and life satisfaction as measured by three multi-item factor scales and a rating of overall quality of life among participants with spinal cord injury (SCI).
Setting:
Large specialty hospital in the Southeastern United States.
Methods:
Participants included 1549 adults with traumatic spinal cord injuries, at least 18 years of age and a minimum of 1-year post-injury at survey. Outcome measures included: (1) home life satisfaction, (2) global satisfaction, (3) vocational satisfaction, (4) overall quality of life and (5) three subscales from the Patient Reported Impact of Spasticity Measure.
Results:
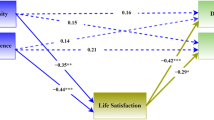
Three aspects of spasticity (daily activities, positive impact and spasticity at its worst) all were negatively correlated with home life satisfaction, global satisfaction and overall quality of life. Only the daily activities scale and the spasticity at its worst rating had a significant negative correlation with vocational satisfaction.
Conclusion:
Spasticity is negatively associated with quality of life after SCI. These negative outcomes need to be considered in an individual's rehabilitation and treatment methods.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (SCI) results in neurological function loss that can cause significant long-term complications including spasticity, pain, pressure sores and fatigue.1 It is estimated that there are 12 000 new cases of SCI a year in the United States alone.2 This study examines spasticity and its potential impact on life satisfaction after SCI.
The definition of spasticity varies widely in the literature; however, several sources cite it as one of the most difficult health complications after SCI.1, 3 Spasticity manifests itself over time after SCI.4 It can develop in both the upper and lower extremities, and over half of those with a cervical injury have spasticity in their upper extremities.5 Pain and inhibition of daily activities are characteristic of problematic spasticity. For example, some individuals experience extension spasticity so powerful that it can eject them from their wheelchair. However, one study found problematic spasticity decreased with time post-injury. There are mixed views on the harms and benefits of spasticity. Benefits include better ambulation and circulation, prevention of intramuscular fat accumulation, assistance in day-to-day activities, and nearly half of those with SCI claim spasticity to have a positive impact on their life.5, 6 However, the presence of spasticity may be a disturbance, if there is a high degree of pain, a high disturbance in day-to-day activities, less range of motion, more contractures or more complications and hospitalizations.1, 7, 8
Quality of life is an important consideration after SCI. One source cites spasticity as a factor in lower quality of life.9 It has been shown that the severity of the spasticity is correlated with many psychological factors.7 One study suggested there was a relationship between ‘reassuring thoughts’ and less spasticity.7 Conversely, excitable emotions, including anxiety, could trigger spasms.10 A key component of this finding is the fact that psychological factors have an important role in a person's perception of the severity of their spasticity.7 The investigation of the relationship between spasticity and life satisfaction is an important one, because individuals’ perceptions of their health and quality of life have been shown to be a risk factor for mortality.11
Purpose
The purpose of this study was to carry out secondary analysis of existing data to identify the relationship between self-reported spasticity and life satisfaction. We used two subscales of the Patient Reported Impact Of Spasticity Measure (PRISM),12 including negative impact on daily activities and the positive effects of spasticity. A rating scale was also used to indicate level of spasticity at its worst. The outcome measures included three factor analytically derived life satisfaction scales from the Life Situation Questionnaire-Revised13 and a rating of overall quality of life. We hypothesize that the daily activities scale and spasticity ratings will be negative predictors of life satisfaction, whereas the positive impact scale will be associated with greater life satisfaction and quality of life.
Participants and methods
Participants
Potential participants were identified, upon approval from the Institutional Review Board, from the records of a large specialty hospital in the southeastern USA. Inclusion criteria were: traumatic SCI, at least 18 years of age, and at least 1-year post-injury at time of survey. A total of 1549 of the 2480 eligible participants returned usable materials (62.5%).
The average age was 45.1 years at the time of the study and 32.5 years at injury. The average number of years of education in the sample was 13.6, 72.9% were male. The majority of the participants were white (72.9%) or black (21.8%). Nearly half (49.8%) sustained their injuries from a motor vehicle accident, followed by other (15.6%), falls or flying objects (13.4%), a sporting injury (10.1%), an act of violence (7.8%) and a medical or surgical complication (2.7%). Cervical injuries were reported by 53.1%. In terms of neurological completeness, 62.3% had sensation below the level of injury, and 46.3% had voluntary movement below the level of injury.
Procedure
Participants were sent preliminary letters describing the research method and to inform them materials would be forthcoming. About 5 weeks later, participants were sent an initial packet containing the survey and a letter detailing the study, which served as implied consent. If the survey was not returned completed, non-respondents were sent a second packet and were also contacted by phone. If the non-respondent had lost the materials but expressed a desire to participate in the study, the individual was sent a third packet. Individuals were given $50 remuneration for their participation.
Measures
Spasticity was measured using select subscales from the PRISM.12 The PRISM was developed in 2005 as a way to measure the impact of spasticity on persons with SCI through self-reported data.12 It is grouped into seven subscales, three of which were administered to the study participants: daily activities, positive impact and need for assistance/positioning.12 Only three subscales of the PRISM were included in the initial assessment in order to limit participant burden, and those three scales were selected to measure, at least conceptually, a combination of both favorable and unfavorable aspects of spasticity (eg, positive impact versus disruption of daily activities). Subscales not measured include: social avoidance/anxiety, psychological agitation, need for intervention and social embarrassment. All were highly correlated with the daily activities scale, and psychological agitation and social embarrassment were highly correlated with need for assistance.14 The questions state, ‘Over the past week, my abnormal muscle control or involuntary muscle movement…’ followed by a phrase pertaining to one of the subscales (for example, Made transfers hard for me or my attendant). Likert scaling is used with options ranging from ‘Never true for me’ to ‘Very often true for me.’ The measure has been shown to have good internal consistency and test/retest reliability, but has not been tested for validity because there is no other similar test of self-reported spasticity.12, 14 Participants were also asked to rate their spasticity at its worst in the past week on a scale from 0 (no spasticity) to 10 (spasticity as bad as you can imagine).
Life satisfaction and quality of life were measured using the Life Situation Questionnaire-Revised.13 Participants rated how satisfied they were with 20 different aspects of life on a scale from 1 (very dissatisfied) to 5 (very satisfied). There are three factor analytic satisfaction scales: home life satisfaction, vocational satisfaction, and global satisfaction.13 The scales had acceptable internal inconsistency and reliability.13 Participants were also asked to rate their quality of life overall on a scale from 1 (worst) to 10 (best). This was used as a more global measure of quality of life, in contrast to the satisfaction items, which measured specific content domains.
Other variables measured included; gender, ambulatory status (yes, no), years of education (at the time of survey), injury level (cervical, non-cervical), race (white, non-white), age at survey and years since injury.
Analyses
The analyses were conducted using SPSS statistical software (SPSS for Windows. 18.0 ed, SPSS Inc., Chicago, IL, USA). Descriptive statistics were generated for all 10 predictive variables (gender, ambulation, age, years since injury, years of education, type of injury, race, positive impact, daily activities and spasticity at its worst). It was determined that the subscale ‘need for assistance/positioning’ was to be eliminated because of its collinearity with the subscale ‘daily activities’ (0.83). Finally, four separate linear regression analyses were conducted, one for each of the three life satisfaction scales and the quality of life scale. Variables were entered simultaneously into each model. Variance inflation factors were used to assess collinearity between independent variables, but no significant collinearity was detected. Beta coefficients and standard errors are reported, and variables with P<0.05 were considered statistically significant.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Home life satisfaction
The regression model for home life satisfaction was significant (F=8.392, DF=10, P<0.001), but the predictors accounted for only 5% of the variation. The final model contained 1358 individuals. Significant predictors of home life satisfaction included chronologic age, years of education and race (Table 1). The reported satisfaction with home life increased with age, as well as the number of years of education. Whites reported higher satisfaction with home life than non-whites. Home life satisfaction had a significant negative association with both the positive impact and daily activities scales from the PRISM, as well as with the rating of spasticity at its worst.
Vocational satisfaction
The predictors accounted for 16.7% of the variance in vocational satisfaction that encompassed a total of 1274 participants in the final model (F=26.54, DF=10, P<0.001). Table 2 summarizes the regression analyses. Three control variables were significant predictors of vocational satisfaction including chronologic age, years of education and race. Vocational satisfaction increased with age, as well as the number of years of education. Whites reported greater satisfaction than non-whites. Severity of the spasticity and spasticity's interference in daily activities were associated with lower levels in vocational satisfaction as well. The positive impact scale was not related to vocational satisfaction.
Global satisfaction
The final model for global satisfaction contained 1329 individuals, and the predictors accounted for 9% of the variation (F=14.02, DF=10, P<0.001). Four control variables were statistically significant (Table 3), including years since injury and years of education, both of which were positively correlated with global satisfaction. Men, and those who were ambulatory reported higher global satisfaction. Each of the three spasticity variables was significant and negatively correlated with global satisfaction.
Overall quality of life
The predictors for overall quality of life accounted for just more than 7% of the variance (n=1, 386 in the final model; F=12.13, DF=10, P<0.001). Quality of life was negatively correlated with chronologic age but positively correlated with years since injury (Table 4). Non-whites reported higher overall quality of life than whites. Each of the three spasticity variables was statistically significant and negatively correlated with overall quality of life.
Discussion
The purpose of this study was to identify the relationship between spasticity and life satisfaction. The literature presented mixed reviews as to whether the relationship would be positive or negative. With spasticity being one of the most problematic health complications after SCI, its impact on an individual's life satisfaction is an important area in terms of rehabilitation and treatment methods.1, 3 For this reason, this study was designed to examine demographic, injury-related and spasticity-related factors that would be relevant predictors of life satisfaction after SCI.
Even after controlling for demographic and injury variables, spasticity indicators were consistently negatively correlated with life satisfaction and quality of life. This included both the positive impact and daily activities scales, as well as spasticity at its worst. With the exception of vocational satisfaction, the predictors accounted for less than 10% of the variation in each outcome, so the strength of the relationships were modest at best. Finding the positive impact scale was actually negatively correlated with most subjective outcomes suggests that spasticity presents significant barriers to quality of life. Although we found perceptions of spasticity were related to psychological outcomes, it is also possible, perhaps likely, that psychological factors influence spasticity itself (not simply perceptions of spasticity). The relationship may indeed be bidirectional.
Although not the primary focus of the study, some additional findings are noteworthy. First, we found limited evidence for a relationship between injury level or ambulatory status with life satisfaction or quality of life, with those who were ambulatory having higher global quality of life. Previous research has suggested that severity of spasticity and severity of injury are correlated;6 so it is interesting that we found spasticity, but not injury severity, to be consistently correlated with life satisfaction. This suggests the need for investigating secondary conditions in relation to subjective outcomes, rather than more general indices of injury severity. Second, previous research has suggested that men and women rarely differ in life satisfaction, except for in areas of interpersonal relations.15 These findings generally support this statement as gender was only significant in relation with global satisfaction. Third, our results somewhat conflict with previous findings that have suggested differences in satisfaction outcomes typically are restricted to vocational/financial areas and favor whites.16 Although whites reported higher satisfaction in home life and vocational satisfaction, non-whites reported higher overall quality of life. However, it is difficult to draw any definitive conclusions from these findings, because no further investigation was carried out in examining differences between all other racial groups present in the sample. Fourth, increasing age has typically been correlated with higher satisfaction in the areas of home environment and employment, and time since injury has been related to higher life satisfaction overall.17
Rehabilitation programs that work to maximize life satisfaction and quality of life should consider the negative correlation between spasticity and life satisfaction. Perhaps the level of an individual's spasticity also needs to be considered when treating the psychological aspects of dealing with SCI. In particular, it is important to consider the effect of spasticity on day-to-day activities and how that may translate into lower satisfaction and quality of life. Medications are frequently used to treat spasticity. However, existing studies have shown pain and spasticity medications are associated with poor functional outcomes that include diminished ability to ambulate community distances (even after controlling for injury severity).18 Medications to treat spasticity, pain, depression and sleep loss have also been associated with a greater risk of mortality.19
Limitations
There were several limitations to the study. First, the measure of spasticity is subjective. The measurements depended on each individual's perception of their situations. With self-reported data such as these, reporting biases may occur. On the other hand, evaluation of satisfaction and quality of life is, by definition, subjective. Second, the data collected were cross-sectional and correlational. We cannot assume causation in the relationships. Although we cannot identify actual changes in the relationship of spasticity and global quality of life throughout the lifetime, we were able to identify the association of years lived post-injury with these variables. Third, there is the chance that there are other confounding variables, not included in the analysis, attributed to the study findings. We accounted for several demographic and injury factors, but it is not possible to account for all potential influences other than spasticity. Lastly, although statistically significant, the strength of the relationship between spasticity indicators and life satisfaction/quality of life indicators was not that strong. We were also not able to control for potential therapies/treatments being used for spasticity. Therefore, additional predictors may need to be accounted for in future studies.
Future research
The results of this study would benefit future research. A longitudinal study could help predict causation in the relationship between spasticity and life satisfaction. Also, only one type of measure was used in measuring both spasticity and life satisfaction. Future research could bring in other measures of the two variables. For example, a physician's evaluation of a participant's spasticity, as well as a participant's perception of their spasticity could bring valuable information to the study. Also, only three of the seven subscales from the PRISM were assessed, and two were used in the analysis due to collinearity. Spasticity is a complicated topic, with many areas needing exploration. It would be also beneficial to look at the relationships between the other PRISM subscales and life satisfaction. Further exploration in bringing the findings on this relationship to a clinical application would greatly benefit those with SCI who have negative outcomes related to spasticity. Specifically, information on the impact of specific treatments for spasticity on quality of life could be used in the tailoring of treatment plans for persons with spasticity.
References
Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG . Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1998; 36: 45–50.
National Spinal Cord Injury Statistical Center. Spinal Cord Injury Facts and Figures at a Glance. In. National Spinal Cord Injury Statistical Center: Burmingham, Alabama, 2010.
Hsieh JT, Wolfe DL, Miller WC, Curt A . Spasticity outcome measures in spinal cord injury: psychometric properties and clinical utility. Spinal Cord 2008; 46: 86–95.
Elbasiouny SM, Moroz D, Bakr MM, Mushahwar VK . Management of spasticity after spinal cord injury: current techniques and future directions. Neurorehabil Neural Repair 2010; 24: 23–33.
Skold C, Levi R, Seiger A . Spasticity after traumatic spinal cord injury: nature, severity, and location. Arch Phys Med Rehabil 1999; 80: 1548–1557.
Gorgey AS, Dudley GA . Spasticity may defend skeletal muscle size and composition after incomplete spinal cord injury. Spinal Cord 2008; 46: 96–102.
Voerman GE, Erren-Wolters CV, Fleuren JF, Hermens HJ, Geurts AC . Perceived spasticity in chronic spinal cord injured patients: associations with psychological factors. Disabil Rehabil 2010; 32: 775–780.
Fleuren JF, Voerman GE, Snoek GJ, Nene AV, Rietman JS, Hermens HJ . Perception of lower limb spasticity in patients with spinal cord injury. Spinal Cord 2009; 47: 396–400.
Adams MM, Hicks AL . Spasticity after spinal cord injury. Spinal Cord 2005; 43: 577–586.
Mahoney JS, Engebretson JC, Cook KF, Hart KA, Robinson-Whelen S, Sherwood AM . Spasticity experience domains in persons with spinal cord injury. Arch Phys Med Rehabil 2007; 88: 287–294.
Krause JS, Zhai Y, Saunders LL, Carter RE . Risk of mortality after spinal cord injury: an 8-year prospective study. Arch Phys Med Rehabil 2009; 90: 1708–1715.
Cook K, Williams A, Teal C, Robinson-Wheelen S, Mahoney J, Engebretson JC et al. The Patient-Reported Impact of Spasticity Measure (PRISM): a new measure assessing the impact of spasticity on persons with spinal cord injury. J Neurol Phys Ther 2005; 29: 204–205.
Krause JS, Reed KS . Life satisfaction and self-reported problems after spinal cord injury: measurement of underlying dimensions. Rehabil Psychol 2009; 54: 343–350.
Cook KF, Teal CR, Engebretson JC, Hart KA, Mahoney JS, Robinson-Whelen S et al. Development and validation of Patient Reported Impact of Spasticity Measure (PRISM). J Rehabil Res Dev 2007; 44: 363–372.
Kemp B, Krause J, Adkins R . Depression among African Americans, Latinos, and Caucasians with spinal cord injury: a exploratory study. Rehabil Psychol 1999; 44: 235–247.
Krause JS, Saladin LK, Adkins RH . Disparities in subjective well-being, participation, and health after spinal cord injury: a 6-year longitudinal study. NeuroRehabil 2009; 24: 47–56.
Krause JS . Aging, life satisfaction, and self-reported problems among participants with spinal cord injury. Top Spinal Cord Injury Rehab 2010; 15: 34–40.
Kohout R, Saunders L, Krause JS . The relationship between prescription medication use and ability to ambulate distances after spinal cord injury. Arch Phys Med Rehabil (in press).
Krause JS, Carter RE, Pickelsimer E . Behavioral risk factors of mortality after spinal cord injury. Arch Phys Med Rehabil 2009; 90: 95–101.
Acknowledgements
The contents of the publication were developed under a grant from the Department of Education, NIDRR Grant Numbers H133B090005 and H133G050165. However, those contents do not necessarily represent the policy of the Department of Education, and you should not assume endorsement by the Federal Government. This publication was also supported by NIH Grant Number 1R01 NS 48117. Its contents are solely our responsibility and do not necessarily represent the official views of the NIH. Special thanks to Karla Reed for her contributions in making this research article possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Westerkam, D., Saunders, L. & Krause, J. Association of spasticity and life satisfaction after spinal cord injury. Spinal Cord 49, 990–994 (2011). https://doi.org/10.1038/sc.2011.49
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.49
Keywords
This article is cited by
-
Phenol neurolysis in people with spinal cord injury: a descriptive study
Spinal Cord Series and Cases (2022)
-
The role of selective dorsal rhizotomy in the management of post-traumatic spasticity: systematic review
Neurosurgical Review (2021)
-
Treatment patterns of in-patient spasticity medication use after traumatic spinal cord injury: a prospective cohort study
Spinal Cord (2018)
-
The experience of spasticity after spinal cord injury: perceived characteristics and impact on daily life
Spinal Cord (2018)
-
Neuropathic pain and spasticity: intricate consequences of spinal cord injury
Spinal Cord (2017)