Abstract
Study design:
A cross-sectional survey.
Objectives:
To document bowel care practices of chronic spinal cord injury (SCI) patients in Pakistan.
Settings:
Outpatient Department, Armed Forces Institute of Rehabilitation Medicine, Rawalpindi, Pakistan.
Methods:
A total of 50 adult patients (18–65 years) with SCI of duration >12 months were sampled by convenience sampling. Medical record was reviewed, detailed neurological examination was performed and face-to-face semistructured interviews were conducted. Data were collected and analysed using SPSS v10. Frequencies and descriptive statistics were calculated for the various variables.
Results:
Most of the patients (29) were males. The mean age was 33±11 years. Majority of the patients (76%) had thoracic-level injury. In all, 43 patients gave a history of occasional or regular faecal incontinence. In addition, 17 patients reported the regular use of laxatives whereas 22 used bulk-forming agents on a regular basis. Majority of the patients (56%) had at least one bowel evacuation daily. In addition, 31 patients required 16–30 min to complete the bowel evacuation. Approximately half (54%) required assistance in bowel evacuation.
Conclusion:
A large number of patients with chronic SCI in Pakistan had faecal incontinence. A majority of patients used methods such as suppositories, laxatives and bulk-forming agents to control the frequency and duration of the bowel programme. Adherence to standard bowel care programme and practices are influenced by sociocultural factors and lack of education on the part of the patients.
Similar content being viewed by others
Introduction
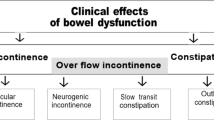
With the improved acute care of spinal cord injuries (SCI), the long-term complications are gaining increased importance as they have a significant influence on the quality of life of these patients. Neurogenic bowel dysfunction is a major physical and psychological problem in SCI patients,1 and it can severely disrupt a patient's quality of life.2 The two main manifestations of neurogenic bowel dysfunction are constipation and faecal incontinence,3 with the prevalence of constipation in these patients reported to be 40–58%,4 and faecal incontinence from 2 to 61%.1, 3Because of these problems, patients with chronic SCI tend to spend more time in the toilet while evacuating their bowels, use suppositories, laxatives and supplemental dietary fibre more frequently to improve bowel evacuation and require manual removal of faeces much more frequently when compared with their matched control population.4
Research on SCI in Pakistan is limited,5, 6, 7, 8 and there are no data available on chronic SCI or bowel-related problems of patients having chronic SCI .The earthquake on 8 October 2005 in Pakistan resulted in hundreds of SCI patients, most of whom were young paraplegic females with complete injury.5 In view of an increased burden of SCI in Pakistan in the past few years, our team is conducting research on different aspects of chronic SCI, and this study is the first preliminary report in the series.
Methods
Approval of hospital ethics committee was obtained before commencing the study. This cross-sectional survey was conducted at the Armed Forces Institute of Rehabilitation Medicine (AFIRM), Rawalpindi, a tertiary-care 100-bed indoor rehab setup, which is the largest in Pakistan at present.9 The spinal rehabilitation unit is the best equipped in the country with a setup of 20 beds for acute and 10 for follow-up cases.
A total of 50 consecutive patients of both genders, between 18 and 65 years of age, with traumatic SCI of >1-year duration and having American Spinal Injury Association (ASIA) impairment scale A–D were enrolled. Patients with lower motor neuron injuries (cauda equina syndrome), pre-existing bowel disorders (for example, irritable bowel syndrome and inflammatory bowel disease) and bowel problems not attributable to SCI were excluded. Convenience (nonprobability) sampling was used. All patients were recruited from the outpatient department and had reported for 6 monthly or yearly follow-up. Verbal informed consent was taken from the patients or caregivers after explaining the purpose of study and use of data for research and publication. Medical records of the patient were checked to record aetiology, type and duration of injury. Neurological examination was carried out to assess ASIA impairment scale.
Semistructured interviews were conducted by principal investigators of the study. Demographical data were obtained and bowel care practices were assessed based on the survey form designed specifically for this purpose. Forms were filled by the patient themselves or their attendants/caregivers. Questions were asked about continence, use of suppositories, laxatives and bulk-forming agents, method of evacuation, bowel programme, frequency of evacuation, assistance required and bladder management.
Data analysis
Data were analyzed using SPSS version 10. Descriptive statistics were used to calculate mean and s.d. for age and time taken to complete bowel programme. Frequency was calculated for gender, continence, use of suppositories, laxatives and bulk-forming agents, manual evacuations, time taken to complete the programme, assistance required and bladder management.
The χ2 or Fisher's exact test was used to compare categorical variables. A P-value of <0.05 was considered statistically significant.
Results
In all, 50 patients with chronic SCI fulfilling the enrollment criteria were interviewed and completed the survey form. These were 29 (58%) males and 21 (42%) female patients. The mean age for all participants was 33±11 years (18–65 years). The duration of injury varied from 13 to 204 months (mean 36 months). Approximately half (26) of the patients had sustained SCI because of the earthquake of 8 October 2005. Remaining 48% had motor vehicle accidents, falls, gunshot and acts of violence as the aetiology. Only 20% of the patients had cervical spine injury. Most were paraplegics (T1–T6=6%, T7–T12=70% and LS=4%). A majority of the patients (43, 86%) had complete injury (ASIA-A), whereas five patients (10%) were categorized as ASIA-C and two as ASIA-D.
Most of the patients (43, 86%) reported faecal incontinence (Figure 1). These included 18 female and 25 male patients. Use of suppositories and laxatives was more common in males. Regular use of bulk-forming agents was the most frequent method used by the patients to regulate bowel movements. There was no statistically significant association between gender and the use of suppositories, laxatives and bulk-forming agents (P=0.11, 0.07 and 0.8, respectively).
In all, 28 patients reported daily bowel movement and 6 had a bowel movement twice a week.
Majority of the patients (84%) usually had bowel movement in the morning whereas the remaining patients (8, 16%) usually had a bowel movement in the evening. Higher the level of injury more was the time consumed in bowel care (Table 1).
In addition, 27 patients (14 males and 13 females) required some form of assistance in the bowel programme (such as transfer to the toilet seat, insertion of suppository, manual evacuation and cleaning after bowel programme) whereas the rest could do it unassisted.
A history of need for manual evacuation of stool regularly was given by 12 (24%) patients. These included 10 male (34%) and 2 female (9.5%) patients. Males were significantly more likely to have required manual evacuation of stools when compared with females (P=0.041; odds ratio 1.38; 95% confidence interval 1.025–1.861).
Most of the patients (62%) were managing bladder by intermittent catheterization. Approximately 20% were performing Credé's manoeuvre, whereas 18% had an indwelling catheter in place.
Discussion
To the best of our knowledge and literature survey, this is the first attempt to address any aspect of chronic SCI in Pakistan and document bowel care practices in this group.
After SCI, most patients experience problems related to the gastrointestinal system. Faecal incontinence holds great importance for patients with SCI because the fear of unexpected bowel movements greatly impairs their social functioning and everyday life.1 A majority (86%) of the patients in this study had regular or occasional faecal incontinence.
One of the possible explanations can be as follows. Most of the patients included in the study (52%) were earthquake victims of October 2005 who, after receiving acute medical/surgical management and indoor rehabilitative care, were discharged to their native homes in the North of Pakistan. At that time the health-care system in that part of Pakistan and Azad Kashmir was totally destroyed in the aftermath of the disaster.7And even now, there are issues with quality health-care delivery and medical setups. Most of these patients were living in tent villages without suitable toilet facilities for many months. It would be extremely difficult for someone living in such abject conditions to follow standard bowel care schedule, thus resulting in an increased frequency of faecal incontinence and constipation. These circumstances that the patients faced may have contributed significantly to the finding of occasional or regular faecal incontinence and constipation.
There are some others issues as well related to Pakistan in the context of bowel management in SCI that merit mention.
-
Most of the Pakistani population live in the rural areas without access to proper toilet facilities, and go out in the fields to attend the call of nature. In the remaining cases, the majority of the toilets in Pakistani household are unfriendly for the disabled and unsuitable for use by SCI patients. Most of the patients sustaining SCI in Pakistan (including participants of this study) are from poor socioeconomic background. Many a times the earning member of the family sustains the injury, resulting in a major financial burden. Most of the savings are spent on the patient's management and there is hardly any resources left for toilet modifications.
-
Indian commode fixed in ground is the most common all around Pakistan. It is totally unsuitable for SCI patients who have no or little useful motor power in lower limbs.
-
Social support care in the form of a large number of dedicated caregivers (mostly family members) is available to most of the patients of SCI at home. Moreover, it is also considered an honour to serve the severely disabled paraplegics in many households. Therefore, these SCI patients are offered bowel care right there on the bed without the need to transfer to toilet. This overcaring attitude negatively influences the standard bowel care practices in these patients.
-
Long-term bowel management in SCI patients has been facilitated by the use of colostomy in the developing world. Both colostomy and ileostomy surgery significantly reduce the amount of time required for bowel management.10, 11 Patients who undergo this surgery tend to be satisfied with their surgery, and a significant portion report a desire to be counselled about this option earlier.10 This is an option hardly offered or used by the SCI patients in Pakistan. One of the possible explanation for underutilization of this option on the part of patients can be that many patients of SCI, including almost all paraplegics of October 2005 earthquake, live in farflung areas with no easy and regular supply of medical products such as colostomy bags/colostomy wafers and so on. These patients are very reluctant to undergo a procedure for which follow-up medical supplies are not easily available.
Sometimes, bowel dysmotility increases to such a degree that manual removal of faeces becomes necessary. Thus, 24% of these patients reported regular requirement of manual evacuation of affected faeces when compared with 19 and 46% reported by De Looze et al.11 and Lynch et al.,12 respectively. The requirement for manual removal of faeces and assistance in toileting puts greater load on caregivers. Therefore, both caregivers and patients should be counselled accordingly so that the burden does not lead to loss of motivation to follow standard bowel care and resultant deterioration of bowel care programmes.
There are some important differences from the bowel care practices reported from a large multicentre cohort of SCI patients from Europe.9 More than half of this study population had a daily bowel movement when compared with 32% from the European cohort. Most of the patients in both groups had bowel movements in the morning or midday and completed their bowel programme in <60 min. The use of oral laxatives was more common in the European sample when compared with the Pakistani sample (55 vs 32%). The frequency of unplanned bowel evacuations was very high in our population (86%) when compared with the European patients (50.8%)
The findings from the study are important in the care of patients with chronic SCI because it is one of the initial efforts in this region to study such problems. We hope that this study opens new vistas in research of the problems of spinal cord injury patients. This effort should lead to a gain in the knowledge database regarding such patients, which will be beneficial to the patients and the health-care resources of Pakistan.
As some of the findings of this study do not conform to literature, these differences need to be validated through larger future studies in Pakistani patients with SCI.
Limitations of the study
This study was carried out on a small cohort of patients with chronic SCI presenting to a specialized rehabilitation centre. There was some oversampling of patients with high injuries (cervical and thoracic). This might have led to some bias in the findings. However, we believe that this was a representative sample of chronic SCI patients in the northern Pakistan, where a significant proportion of such patients got injured during the earthquake on 8 October 2005. Hence, the findings of this study can be applicable to the patients of chronic SCI from northern Pakistan.
Conclusions
A majority of the patients with chronic SCI have a history of occasional or regular faecal incontinence. The frequency of faecal incontinence is significantly greater in Pakistani patients than the data reported from the developed world. Most of the patients control their bowel programme with laxatives, bulk-forming agents and suppositories and require some assistance in their bowel programme. Larger, multicentre studies are needed to validate the findings of this study and, in turn, to formulate clinical guidelines for management of bowel care in patients with chronic SCI in Pakistani/developing world settings.
References
Glickman S, Kamm MA . Bowel dysfunction in spinal-cord-injury patients. Lancet 1996; 347: 1651–1653.
Benevento BT, Sipski ML . Neurogenic bladder, neurogenic bowel, and sexual dysfunction in people with spinal cord injury. Phys Ther 2002; 82: 601–612.
Ng C, Prott G, Rutkwski S, Li Y, Hansen R, Kellow J et al. Gastrointestinal symptoms in spinal cord injury: relationships with level of injury and psychologic factors. Dis Colon Rectum 2005; 48: 1562–1568.
Lynch AC, Anthony A, Dobbs BR, Frizelle FA . Anorectal physiology following spinal cord injury. Spinal Cord 2000; 38: 573–580.
Rathore MF, Rashid P, Butt AW, Malik AA, Gill ZA, Haig AJ . Epidemiology of spinal cord injuries in the 2005 Pakistan earthquake. Spinal Cord 2007; 45: 658–663.
Rathore MF, Hanif S, Farooq F, Butt AW, Ahmed N . Traumatic spinal cord injuries at a tertiary care rehabilitation institute in Pakistan. J Pak Med Assoc 2008; 58: 53–57.
Rathore FA, Farooq F, Muzammil S, New PW, Ahmad N, Haig AJ . Spinal cord injury management and rehabilitation: highlights and shortcomings from the 2005 earthquake in Pakistan. Arch Phys Med Rehabil 2008; 89: 579–585.
Raja IA, Vohra AH, Ahmed M . Neurotrauma in Pakistan. World J Surg 2001; 25: 1230–1237.
Haas U, Geng V, Evers GC, Knecht H . Bowel management in patients with spinal cord injury—a multicenter study of the German speaking society of paraplegia (DMGP). Spinal Cord 2005; 43: 724–730.
Hocevar B, Gray M . Intestinal diversion (colostomy or ileostomy) in patients with severe bowel dysfunction following spinal cord injury. J Wound Ostomy Continence Nurs 2008; 35: 159–166.
De Looze DA, Van Laere M, DeMuynck MC, Beke R, Elewaut AG . Constipation and other chronic problems in spinal cord injury patients. Spinal Cord 1998; 36: 63–66.
Lynch AC, Wong C, Anthony A, Dobbs BR, Frizelle FA . Bowel dysfunction after spinal cord injury: a description of bowel function in a spinal cord-injured population and comparison with age and gender matched controls. Spinal Cord 2000; 38: 717–723.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yasmeen, R., Rathore, F., Ashraf, K. et al. How do patients with chronic spinal injury in Pakistan manage their bowels? A cross-sectional survey of 50 patients. Spinal Cord 48, 872–875 (2010). https://doi.org/10.1038/sc.2010.46
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.46
Keywords
This article is cited by
-
Current and future international patterns of care of neurogenic bladder after spinal cord injury
World Journal of Urology (2018)
-
Constipation in degenerative cervico-thoracic spine myelopathy: a simple co-existence or a complex inter-relationship?
European Spine Journal (2017)