Abstract
Study design:
Cross-sectional survey.
Objectives:
To determine the employment outcomes of persons with spinal cord injury (SCI) and to investigate the impact of various demographic, injury-related and work-related variables on these outcomes.
Setting:
People living with SCI in Malaysia who are members of a disability support organization.
Methods:
A total of 84 members of the Malaysian Spinal Injury Association, who have had traumatic SCI for at least 2 years and were between 15 and 64 years of age at the time of study, were interviewed through phone using a questionnaire to identify the association between demographic, injury-related and work-related variables and employment outcomes.
Results:
The return to work rate in this study was 57.1% (employed at the time of study). The overall employment rate after SCI was 76.2% (worked at some point after injury). Those who were younger at time of injury (<20 years of age), able to drive a modified vehicle, independent in personal care and mobility were positively related to being employed. On the other hand, being hospitalized in the preceding 1 year and receiving financial incentives were negatively related to employment.
Conclusion:
Functional independence, especially ability to drive, was strongly associated with return to work and should be one of the priority goals of comprehensive rehabilitation of persons with SCI. The negative impact of recent hospitalization as well as financial compensation needs to be probed further.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is one of the major physically disabling medical conditions. The objectives of SCI rehabilitation include not only prevention of death and disability but also community reintegration and improving quality of life.1, 2 Studies have shown positive correlation between activity, both social and vocational, with quality of life measures3, 4 and even survival.5
Return to work rates in published literature varies greatly and this is mainly because of different methodologies, study sample characteristics, definitions of employment and employment rates. Yasuda et al.,6 in a review of studies on return to work published between 1995 and 2001, found rates ranged from 13.8% to 39.3%. Another review by Lidal et al.7 for studies published between 2000–2006 reported a rate between 21.0 and 67.0% for those working at the time of injury. Another recent review of studies published between 1992–2005 concluded that ∼40% of working age people greater than 12 months after injury were employed at the time of data collection.8
In reviewing factors associated with employment, access issues and financial disincentives were consistently identified as barriers to return to employment.9, 10, 11 One factor consistently associated with success was higher educational level.9, 10, 11 Pflaum et al.12 in a study on work life after traumatic SCI found a greater likelihood of employment for those with less severe disability, greater education and those in a stable marriage, whereas Anderson et al.13 found 14 factors linked with varying degrees of employment status, namely, education, type of employment, severity of the lesion, age, time since injury, sex, marital status, social support, vocational counseling, medical problems, employer's attitudes, race, psychologic state and environment.
The objectives of this study were to determine the employment outcomes of a sample of local population of persons with SCI and to study the impact of various demographic, injury-related and work-related variables on employment outcomes. To the authors’ knowledge, there has been no Malaysian study examining employment outcomes and associated determinants after a major disability such as SCI. In Malaysia, there are many governmental as well as non-governmental agencies involved in promoting the rights of the disabled including employment issues. Unfortunately, there is no effective coordination and the enforcement of many policies is lacking. The public transportation systems are not disabled friendly, and access to built environment is also an issue.
Methods
Participants and procedures
All participants were randomly selected from the Malaysian Spinal Injury Association (MASIA) membership list. MASIA is a non-governmental organization that primarily functions as a support group for persons living with SCI. The membership is voluntary and open to those who have sustained SCI due to trauma or any disease resulting in disability. MASIA was chosen for sampling of persons living with SCI in the community, as it had a large number of members (306 at the time of this study) of various ages, education and background from almost all the different states in Malaysia (rural and urban areas). On the other hand, the databases from the two major hospitals in Malaysia with SCI rehabilitation units, University Malaya Medical Center (UMMC) and Hospital Kuala Lumpur, were incomplete. It was also felt that using these two urban hospitals’ patient database would introduce bias in subject selection and may not be representative of persons living with SCI in Malaysia.
There were three inclusion criteria: (i) traumatic SCI, (ii) minimum 2 years after injury and (iii) age between 15–64 years. The age group was chosen based on Malaysian Department of Statistics definition of economically active population.14 This term of reference is also used in Malaysian Labour Force Survey and the population census. The respondents were selected using random sampling technique. MASIA's list of members was alphabetically ordered and 155 persons were selected. However, 44 (29.3%) could not be contacted, (out of this, only 5 did not have any contact numbers), 3 (2.0%) could not be interviewed because of language barrier and 1 (0.7%) refused to participate, giving a total of 48 non-responders (30.9%). Two were deceased and eight excluded because of age limit, leaving 97 persons who responded (64.7%). The selected participants were contacted through phone and were informed of the objectives, confidentiality and voluntary nature of participation in the study, and those who gave consent were interviewed. However, 12 persons had non-traumatic SCI and one has fully recovered with no disability and therefore excluded, leaving 84 participants. Approval to conduct this study was obtained from the Ethics Committee of UMMC, Malaysia.
Measure
A questionnaire was designed, with the main outcome variable being employment status at the time of the study. A dichotomous variable was used in the analyses (participating in work and non-participating in work). In accordance with the resolution concerning statistics of the economically active population adopted by the 13th International Conference of Labour Statisticians (Geneva 1982),15 both paid employment and self-employment were considered as participation. The employed is defined as all persons within a specific age group who during a specified period were in one of the above categories.
Paid employments are those jobs where the incumbents hold explicit (written or oral) or implicit contracts and are typically remunerated by wages and salaries. Self-employments are those jobs where the remuneration is directly dependent upon the profits derived from the goods and services produced. Students, homemakers and those in training (not within a job contract) were not counted as in active employment.
As this study was based on self-reported data, the International Standards for Neurological Classification of SCI by the American Spinal Injury Association could not be followed to determine the neurological level or completeness of the injury. Participants were interviewed as to whether they have weakness in the legs only (paraplegia) or involving the upper extremities as well (tetraplegia). As for the functional independence level, they were asked on three aspects, namely, whether they are independent in caring for all their personal needs including bowel and bladder, independent in locomotion including self-wheelchair transfer and whether they are able to drive a modified, hand-controlled car or ride a modified, hand-controlled three-wheeled motorcycle.
Analyses
Descriptive statistical analyses were performed using SPSS version 18.0 (SPSS BI Malaysia Sdn Bhd, Kuala Lumpur, Malaysia). Differences in the variables between the two groups (with and without employment at time of study) were tested using χ2-statistics obtaining P-values, and where appropriate, risk estimates were obtained giving odds ratios with 95% confidence interval. The significance level was chosen as P<0.05.
Results
Descriptive
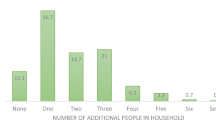
Most participants were male (83.3%) and slightly more than half were of Chinese ethnicity (52.4%). Motor vehicle crash was the primary etiology (73.8%). Majority had paraplegia (77.4%). The mean age at time of injury was 24.7 years (s.d.=8.8), and ranged between 6 and 48 years. Most injuries occurred between the ages of 15 and 35. The mean age at the time of study was 39.8 years (s.d.=10.5), the youngest participant was 22 years of age and the oldest, 62 years. The mean duration of injury in this study was 15.0 years (s.d.=8.6), with the range of 2.0–44.0 years. A total of 22 persons (26.2%) had been injured more than 20 years.
Return to work rate
The return to work rate in this study was 57.1% (employed at the time of study). The overall employment rate after SCI was 76.2% (worked at some point after injury).
Impact of the various demographic, injury-related and work-related variables on employment outcome
All the demographic variables were not significantly related with employment outcome in this study as shown in Table 1. There were more men returning to work compared with women but if homemaker status is considered an occupation, this difference becomes reversed. There were three female participants who considered themselves as homemaker after SCI, whereas none were in that status before injury. The education level in this study was stratified according to the Malaysian levels of education, whereby primary education is for the first 6 years, followed by another 5 years of secondary education, both of which are heavily subsidized by the government. After secondary or tertiary level education includes college, vocational skill training, university, graduate and postgraduate levels. There was no difference in education levels between those who were in employment and those who were not.
The injury-related variable that achieved statistical significance in this study was age at the time of injury, favoring the younger age group (as shown in Table 2). Among those who were injured after the age of 40 years, none returned to work, and among those who have been living the longest with SCI, more than 30 years, 80.0% returned to work. There were more persons with paraplegia who were working (60.0%) compared with persons with tetraplegia (47.4%) but this did not achieve significance. One of the strongest variables in favoring positive employment outcome after SCI in this study was the ability to drive a modified vehicle (Table 2). Majority (79.5%) of those who were able to drive were in occupation compared with only 32.5% of those who were not able to. Independence in personal care and mobility were also significant in favoring positive employment outcome.
This study also found that those who were hospitalized in the last 1 year were less likely to work. This only compared hospitalization related to spinal injury, such as urinary tract infection and pressure ulcer. However, examining the impact of comorbid medical conditions, like diabetes mellitus and hypertension, did not find any significant difference on employment outcome. A total of 18 (21.4%) persons out of 84 had associated medical problems, mainly diabetes mellitus and hypertension, and almost all were in the older age group. The status at the time of injury, whether employed or not, also did not influence employment outcome. Those receiving financial incentive, however, were less likely to return to work.
Discussion
This study has found a relatively high (57.7%) return to work rate among spinal cord-injured persons compared with the published rates in the literature of between 13.8 and 67.0%.4, 5, 7, 9, 10, 11, 12, 13 The reason for the relatively high rate could possibly be sheer economic necessity. On the other hand, this study found that those receiving financial compensation were less likely to be in employment. In Malaysia, a significant proportion of the workers is covered under work insurance scheme, enabling them to receive monthly income in the event that they are unable to return to work. The education level in this study did not affect employment outcome. This is in stark contrast to most other studies that found education to be the most significant factor. One possible reason could be that, overall this study population did not have a high educational background. The mean number of years in education is only 9.3 years (s.d.=3.6) at the time of injury. A total of 3 persons (3.6%) had no formal education and there were only 8 persons (9.6%) with college or university level education. The significant impact of functional independence level on employment outcome underscores the importance of rehabilitation and this agrees with many other studies’ findings as well.10, 16 The ability to drive or ride a modified vehicle was very significant in determining outcome. This potentially removes the barrier of inaccessible public transportation system. This was also a significant finding in a few other studies.10, 11 Being younger at the time of injury (less than 20 years old) was also positively related to employment, whereby among those who were older than 40 years at time of injury, none returned to work. Krause and Anson16 also found similar finding in that those older than 50 years at injury were unlikely to return, unless they return to their preinjury job. It was also mentioned that a large percentage who return to work after SCI terminate employment in their 50s, and therefore early retirement may be an attractive and viable option. Hospitalization in the last 1 year (up to the time of interview) was also significant in disrupting employment outcome and needs to be investigated further whether such admissions were truly necessary or if they can be avoided or prevented, given their adverse impact on employment outcomes.
Conclusion
In conclusion, this study found a relatively high return to work rate of 57.7% (at time of study), and overall 76.2% have worked at some point since injury. The significant positive factors related to employment were being of younger age at the time of injury, independence in personal care, mobility and ability to drive modified vehicle, whereas being hospitalized in the last 1 year and receiving financial incentives were negatively related to employment after injury.
References
Wood-Dauphinĕe S, Exner G, The SCI Consensus Group. Quality of life in patients with spinal cord injury-basic issues, assessment and recommendations: results of a consensus meeting. Restor Neurol Neurosci 2002; 20: 135–149.
Krause JS, Sternberg M, Maides J, Lottes S . Employment after spinal cord injury: differences related to geographic region, gender and race. Arch Phys Med Rehabil 1998; 79: 615–624.
Krause JS, Anson CA . Adjustment after spinal cord injury: relationship to participation in employment or educational activities. Rehabil Counsel Bull 1997; 40: 202–214.
Krause JS . Dimensions of subjective well-being after spinal cord injury: an empirical analysis by gender and race/ethnicity. Arch Phys Med Rehabil 1998; 79: 900–909.
Krause JS, Sternberg M, Lottes S, Maides J . Mortality after spinal cord injury: an 11-year prospective study. Arch Phys Med Rehabil 1997; 78: 815–821.
Yasuda S, Wehman P, Targett P, Cifu DX, West M . Return to work after spinal cord injury: a review of recent research. NeuroRehabilitation 2002; 17: 177–186.
Lidal IB, Huynh TK, Biering-Sorensen F . Return to work following spinal cord injury: a review. Disabil Rehabil 2007; 29: 1341–1375.
Young AE, Murphy GC . Employment status after spinal cord injury (1992–2005): a review with implications for interpretation, evaluation, further research, and clinical practice. Int J Rehabil Res 2009; 32: 1–11.
Castle R . An investigation into the employment and occupation of patients with spinal cord injury. Paraplegia 1994; 32: 182–187.
Jang Y, Wang Y-H, Wang J-D . Return to work after spinal cord injury in Taiwan: the contribution of functional independence. Arch Phys Med Rehabil 2005; 86: 681–686.
Conroy L, McKenna K . Vocational outcome following spinal cord injury. Spinal Cord 1999; 37: 624–633.
Pflaum C, McCollister G, Strauss DJ, Shavelle RM, DeVivo MJ . Worklife after traumatic spinal cord injury. J Spinal Cord Med 2006; 29: 377–386.
Anderson D, Dumont S, Azzaria L, Le Bourdais M, Noreau L . Determinants of return to work among spinal cord injury patients: a literature review. J Vocat Rehabil 2007; 27: 57–68.
ILO. Sources and Methods: Labour Statistics (Malaysia Labour Force Survey) Economically Active Population, Employment, Unemployment and Hours of Work, 3rd edn, vol. 3. ILO: Geneva, 2004.
ILO. Resolution concerning statistics of the economically active population, employment, unemployment and underemployment. Adopted by The 13th International Conference of Labour Statisticians (ICLS). ILO: Geneva, October 1982.
Krause JS, Anson CA . Employment after spinal cord injury: relation to selected participant characteristics. Arch Phys Med Rehabil 1996; 77: 737–743.
Acknowledgements
This project was funded by the short-term project grant from the University Malaya, Malaysia; #IPPP/UPDiT/Geran(PJP)/F0176/2005A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ramakrishnan, K., Chung, T., Hasnan, N. et al. Return to work after spinal cord injury in Malaysia. Spinal Cord 49, 812–816 (2011). https://doi.org/10.1038/sc.2010.186
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.186
Keywords
This article is cited by
-
Labour market participation among rehabilitated individuals with spinal cord injury in Brazil: a cross-sectional study
Spinal Cord (2023)
-
Return to work status in rehabilitated South Indian persons with spinal cord injury: a cross-sectional survey
Spinal Cord Series and Cases (2021)
-
Characteristics of persons with spinal cord injury who drive in Malaysia and its barriers: a cross sectional study
Spinal Cord (2018)
-
Leisure time physical activity participation in individuals with spinal cord injury in Malaysia: barriers to exercise
Spinal Cord (2018)