Abstract
Objective:
To evaluate the serum melatonin levels in acute period of the spinal cord injury (SCI) caused by trauma in the rats.
Background:
Traumatic SCI induces many types of physiological and pathological damage, including hormonal level variations.
Methods:
Forty male Sprague–Dawley rats were divided randomly into four groups. In the control group, neither laminectomy nor SCI were performed; only a large laminectomy was performed without SCI in the sham group. In the cervical and thoracic spinal trauma groups, laminectomies at C5-6 and a T6-7 were performed, respectively, followed by clip compression of the spinal cord. Blood samples were drawn 2, 6, 12 and 24 h after the procedures and assayed immediately.
Results:
The levels of melatonin in the neurotrauma groups were high in the first 2 h, but at the end of sixth hour, melatonin levels increased in sham-operated group, decreased in neurotrauma groups and did not change in control group. At the 12th hour, melatonin levels continued to decrease in thoracic group significantly. At the 24th hour, the melatonin levels decreased in the cervical, control and sham groups, whereas melatonin levels increased in the thoracic group.
Conclusions:
The present study revealed that (1) activation of endogen melatonin secretion of the organism starts immediately after the SCI, but it shows a great lowering trend between 2 and 6 h post-SCI, (2) the tetraplegic rats, which had complete injuries at the lower cervical spinal cord, could not produce enough melatonin secretion; on the contrary, the paraplegic rats, which had complete injury at the upper thoracic spinal cord, showed normal melatonin secretion.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (SCI) leads to the earliest biochemical reactions, such as enzymatic lipid hydrolysis, production of biologically active eicosanoids, decrease of sodium, potassium and ATP-ase activity, and peroxidation of lipids with the formation of free oxygen radicals.1, 2, 3, 4 The primary traumatic mechanical injury to the spinal cord causes the death of a number of neurons that cannot be recovered and none regenerated, but some neurons continue to die for hours after traumatic SCI. This secondary neuronal death may be caused by substances released from cells in response to the primary injury.5
Recent studies have found that melatonin is a very efficient scavenger of the hydroxyl and peroxyl radicals as well as an electron donor.1, 2, 3, 4, 5, 6, 7, 8, 9 Being lipophylic and hydrophilic, it has an extreme diffusability for scavenging in cells and every subcellular compartment. In addition, it can protect membrane lipids and protein components, nucleus and all the cells.2 As the direct free-radical scavenging activities of melatonin do not require its mediation by a receptor, melatonin ability to protect against oxidative damage is likely the result, at least in part, of its free-radical scavenging activity. As it is highly lipophilic and quite hydrophillic as well, it may potentially protect against the occurrence of oxygen toxicity in nuclear deoxyribonucleic acid. Fujimoto et al.1 showed that their results suggested not only the protection conferred by melatonin on oxidative damage, but also its ability to reduce neutrophil-induced toxicity. It has been suggested that melatonin may also have strong anti-inflammatory effects.5 Additional protective effects of melatonin may lie within the ability of this hormone to reduce oxyradical-related oxidant processes by either directly interfering with the oxidants or up-regulating antioxidant systems, such as superoxide dismutase or enhancing the catalytic activity of glutathione peroxidase.10 Melatonin has also been proposed as an antiapoptotic agent, as it readily penetrates the blood–brain barrier and diffuses into neurons and glia equally well.3, 7, 11
SCI induces many types of physiological and pathological damage including variations in various hormonal levels. A number of hormones are known to be involved in the modulation of neurotrophic, neurogenic and neuroprotective events that take place within the central nervous system. The purpose of this study was to evaluate the serum levels of melatonin, which has been proved before by many neuroprotective effects, in acute period of SCI caused by trauma in rats.
Materials and methods
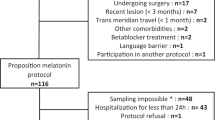
Forty male Sprague–Dawley rats weighting from 250 to 340 g were handled according to Principles of Laboratory Animal Care. All experimental procedures were approved by the Institutional Animal Care and Use committee. They were housed three per cage under diurnal lighting conditions (12 h darkness and 12 h light), fed by pellets (Purina Rodent Chow) and allowed free access to water before the experiment. They were kept under controlled temperature (25±2 °C). All the rats were anesthetized by intraperitoneal (i.p.) injection of sodium pentobarbital (50 mg kg–1 BW, Sigma Chemical Company, St Louis, MO, USA) and allowed to breathe room air. The depth of anesthesia was monitored by frequent testing of leg reflexes and muscle tonus. The rats were divided randomly into four groups. Group C was the control group (n=9) and neither laminectomy nor SCI were performed. It constituted the basal levels for the other study groups. Group S was the sham group (n=9), which performed C6-T2 laminectomy without SCI. Group SCI-C was the cervical spinal trauma group (n=13), nine of them survived within 24 h period). The animals had a C5-C6 laminectomy and then spinal trauma was performed at this level using the method described below. Group SCI-T was the thoracic spinal trauma group (n=9). The animals had a T6-T7 laminectomy and then the same trauma procedure was performed.
The surgical operations were conducted in 3 days. First day, the sham group, the second day, SCI-C group and the third day, SCI-T group of animals were operated. We started the operations at 8 a.m. when the appropriate level of anesthesia was reached and all the animals were completed at around 9 a.m. for three groups (∼20 min for each animal). By this way, we would be able to collect blood samples at the same time for the groups. The first blood sample (2 h after the operation) was collected at around 11 a.m., the second blood sample (6 h after the operation) was collected at around 3 p.m., the third blood sample (12 h after the operation) was collected at around 9 p.m. and the last blood sample (24 h after the operation) was collected the next day at around 9 a.m. (Table 1). The animals underwent skin incision, paravertebral muscle dissection and performed either cervical or thoracal laminectomies under loop magnification. The prominent spinous process of T2 was used as a surgical guide. We used the clip compression model described by Rivlin and Tator.12 SCI was accomplished by extradural compression of the exposed spinal cord for 30 s using an aneurysmal clip with a closing force of 50 g on the cord. The same clip was used in all the animals in which SCI was induced. This clip force was chosen, as it produces a complete SCI as described by Rivilin and Tator.12 A complete injury is characterized by loss of tone and flaccid paralysis below the level of the lesion.
Blood samples were drawn 2, 6, 12 and 24 h after surgery and spinal traumas and assayed immediately (Table 1). For melatonin measurements, blood samples were taken from the orbital sinus of each animal under light ether anesthesia. Samples during the dark phase were collected under dim red light. The withdrawn blood was substituted by an equal volume of 0.9% NaCl immediately injected i.p. after blood collection. After the surgical procedures, hemodynamic measurements were recorded continuously for 60 min and they averaged for each animal (Table 2). Blood samples were centrifuged at 4 °C for 30 min at 4000 rpm and serum aliquots were frozen at −20 °C. Hormones were measured by commercial ELISA kits according to the manufacturer's instructions. Serum melatonin levels were measured in duplicate using 96-well microtiter plate coated with captured antibody goat antirabbit Ig (Immuno-Biological Laboratories-Turkey Ltd Sti. Yenimahalle, Ankara, Turkey). After extraction of samples, standards and controls with extraction columns, each microtiter plate was filled either with 50 μl of blanking reagent, zero calibrators, standard solutions containing 5, 10, 20, 50, 500 and 1000 pg ml–1 of melatonin and samples. An auotomatic well-washer was used for washing (Wellwash 4 Mk2, Thermo Electron Corporation, Vantaa, Finland). Optical densities were determined at 450 nm in an automatic microplate reader (Multiscan Ascent, Thermo Electron Corporation, Vantaa, Finland). Serum melatonin concentrations were expressed as pg ml–1. The sensitivity of the melatonin assay was 3.0 pg ml–1. Both the intra- and inter-assay coefficients of variation were <10% in the assays.
Statistical analysis
Data were analyzed by using Sigma Plot (SYSTAT Software Inc., Ver. 11.0, Chicago, IL, USA). Hormone levels were analyzed by Friedman Repeated Measures Analysis of Variance on Ranks followed by Tukey's multiple range test. Values were considered statistically significant at P<0.05. Data were presented as mean±s.e.m.
Results
All the animals in the cervical spinal lesion group (SCI-C) had flaccid tetraplegia and sphincter control loss immediately after cervical trauma. Three animals showed apnoea or dispnoea after the procedure, but none was connected to respirator. As four animals died in the first 6-h period, they were excluded from the experiment. No important breathing alteration was observed in the rest of the animals in this group. All the animals in the thoracic spinal lesion group (SCI-T) presented severe flaccid hind limb plegia and loss of sphincter after spinal trauma. No apparent variation in respiratory rhythm was observed in this group, and except cervical group, there are no any statistical differences in mean hemodynamic values (Table 2).
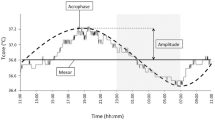
Serum melatonin levels were represented in Figure 1. At the second hour, Friedman Test did not detect a significant difference between the control and sham-operated groups (F=2.15, P=0.092, df=5), but cervical (∼240 pg ml–1) (F=13.33, P=0.002, df=2) and thoracic (∼300 pg ml–1) (F=17.21, P=0.001, df=2) groups were statistically higher than control (∼130 pg ml–1) and sham-operated animals (∼138 pg ml–1). At the sixth hour, Friedman Test detected significant changes in sham-operated, cervical and thoracic groups; melatonin levels increased in sham-operated group (F=4.88, P=0.043, df=5), decreased in cervical (F=5.27, P=0.031, df=4) and thoracic groups (F=6.14, P=0.012, df=3), and did not change in control group (F=0.91, P=0.412, df=5); however, at that time, the groups were similar to each other (F=0.56, P=0.878, df=6), except controls (F=4.55, P=0.045, df=4). At the 12th hour of the experiment, Friedman Test detected significant changes in control and thoracic groups; melatonin levels increased in control (F=5.64, P=0.035, df=5), decreased in thoracic groups (F=8.91, P=0.0042, df=3), but did not change significantly in sham-operated (F=1.63, P=0.402, df=4) and cervical groups (F=1.92, P=0.380, df=4). The groups were similar to each other (F=4.22, P=0.060, df=5), except the thoracic groups (F=4.63, P=0.048, df=5). At the 24th hour of the experiment, Friedman Test detected significant changes in all groups; melatonin levels decreased in control (F=6.50, P=0.009, df=3), sham-operated (F=5.44, P=0.028, df=4) and cervical groups (F=5.12, P=0.032, df=5); however, increased in thoracic group (F=7.31, P=0.006, df=3). Control, sham-operated and cervical groups were similar to each other (F=2.66, P=0.076, df=4); however, thoracic group was significantly higher from the others (F=5.34, P=0.029, df=4).
Twenty-four hour serum melatonin levels (mean±s.e.m.) in four study groups are seen. At the 24th hour, melatonin levels decrease in control, sham-operated and cervical groups; however, increase in thoracic group, which shows a significant difference from the other study groups. Different letters indicate the statistically significant difference among the groups (P<0.05).
Discussion
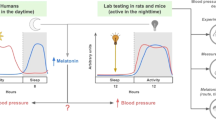
The hormone, melatonin (N-acetyl-5-methoxy-tryptamine), which mainly produced by the pineal gland takes part in many important physiological activities, such as regulating of circadian rhythms and modulation of immune function.11 Its rhythmic production by the pineal gland was described in human beings over 20 years ago. The presumptive protein responsible for binding melatonin in blood is albumin.13 The production of melatonin is cyclic with highest concentrations being present during the dark phase of the light/dark cycle. This rhythmic pattern is directly or indirectly associated with other physiological functions. In most mammals, the pineal gland produces and releases melatonin into the circulation almost entirely at night. This nocturnal secretion is circadian in nature and depends on stimuli initiating from the supra chiasmatic nuclei, the site of the biological clock. During the daily light phase, transmission of adrenergic stimuli that initiate the biochemical transformation of serotonin to melatonin is inhibited by light.13, 14 The day–night rhythm of melatonin levels is due to the release of norepinephrine from the sympathetic nerve endings in the pineal gland. The differences between leptin and melatonin rhythms are the different peak levels of leptin and melatonin; leptin is found during the day and melatonin is found at night. Supra chiasmatic nucleus controls the sympathetic input to the pineal gland. Thus, the circadian control of leptin levels is important and shows similarity with melatonin.14
The human circadian pacemaker, located in the paired hypothalamic suprachiasmatic nuclei, regulates the timing and amplitude of several endocrinological functions, including cortisol and melatonin through a neural or neurohumoral circuit. Cortisol, controlled by neurohumoral signaling in the hypothalamus—pituitary–adrenal axis, is a pulsatile hormone secreted with daily rhythmicity. Melatonin is typically produced in a single night episode, with onset occurring just before bedtime and offset occurring soon after weaktime. Unlike cortisol, melatonin is thought to be influenced by the suprachiasmatic nuclei primarily through an efferent neural pathway passing through the brain and spinal cord, with innervations of the pineal gland by the superior cervical ganglia.15 However, in the absence of innervation from the superior cervical ganglion, it is unclear whether non-rhythmic pineal production of melatonin continues.6, 16
In addition, it has been hypothesized that parasympathetic nerves and nerves that arise from the pretectum, which circumvent the spinal cord, innervate the pineal and may be able to significantly influence its production of melatonin.3, 17 Neurologically complete SCI would interrupt sympathetic hypothalamic, but not parasympathetic or pretectal, signaling to the pineal gland if the level of the injury were above the nerve roots that innervate the superior cervical ganglia. It has been hypothesized that such disruption abolishes rhythmic melatonin production.6, 16 SCI also disrupts afferent signaling to the hypothalamus from somatic nerves below the level of the lesion. Such disruption may indirectly affect the secretion of cortisol. In the literature, anatomic studies in human beings indicate that the innervation of the pineal arises from thoracic roots 1–4.18 In another study, their data further suggest that neither the putative pathway that leads directly from the pretectum to the pineal nor parasympathetic innervation is sufficient to generate measurable pineal melatonin secretion in human beings.3, 17 In contrast to the disruption of the melatonin circuit, the neurohumoral influence of the hypothalamus on cortisol remains intact in SCI, although the spinal influences on the adrenal cortex that convey information about acute environmental changes may be disrupted. However, very little data on the variation in serum melatonin level during the acute phase of SCI are available.
In the present study, levels of melatonin in the neurotrauma groups were high in the first 2 h, but at the end of sixth hour, melatonin levels increased in sham-operated groups, whereas decreased in cervical and thoracic groups; however, at that time, the groups were similar to each other except controls (Figure 1). At the end of 12th hour of the experiment, melatonin levels increased in control (P<0.05), whereas decreased in thoracic group (P<0.05), but did not change significantly in sham-operated and cervical groups (P>0.05). At the end of 24th hour of the experiment, melatonin levels decreased in control and sham-operated groups; so we thought that they returned the normal diurnal rhythm. The levels decreased much more in the cervical group agonist to starting point, whereas melatonin levels increased in the thoracic group (P<0.05). This results may support that the tetraplegic rats, which had complete injury at the lower cervical spinal cord, could not produce enough melatonin secretion. This can be explained as without peripheral sympathetic innervations of the pineal gland, any parasympathetic or direct innervations of the pineal by the pretectum is insufficient to generate significant melatonin secretion in rats similar to human beings.6, 16, 17 In other words, our data support the hypothesis that the human pineal must be stimulated by the sympathetic nerves system to produce melatonin. On the contrary, the paraplegic rats, which had complete injury at the upper thoracic spinal cord, showed normal melatonin secretion similar to human beings.6, 17
Although it is known that surgery induces a release of some hormones especially cortisol, surgical stress does not seem to affect the serum levels of melatonin significantly in our study, as it remained not changed so much after surgery in sham group animals according to the control group. Particularly, in the first 2 h, the levels of melatonin were found significantly high in the neurotrauma groups according to both control and sham groups. We thought that this elevation might be directly related to parasympathetic nerves and the nerves that arise from the pretectum, which circumvent the spinal cord, innervate the pineal and may be able to significantly influence its production of melatonin.3, 17 However, it was seen that this stimulation was not enough to continue producing melatonin secretion in the cervical trauma group.
In conclusion, we can say that activation of endogen melatonin secretion of the organism starts immediately after the injury, but it shows a great hesitation period between 2 and 6 h of post-SCI. This may support the importance of beginning the neuroproductive treatment in the first 3-h period after SCI as reported in NASCIS III.19 These findings invite further investigation of their potential roles and the timing of medical treatment in neuroprotective process of neurological injury.
References
Fujimoto T, Nakamura T, Ikeda T, Katsumasa T . Potent protective affects of melatonin on experimental spinal cord injury. Spine 2000; 25: 769–775.
Melchiorri D, Reiter RJ, Attia AM, Hara M, Burgos A, Nistico G . Potent protective effect of melatonin on vivo paraquat-induced oxidative damage in rats. Life Sci 1995; 56: 83–89.
Sparks DL . Anatomy of a new paired tract of the pineal gland in humans. Neurosci Lett 1998; 248: 179–182.
Topsakal C, Kilic N, Ozveren F, Akdemir I, Kaplan M, Tiftikci M et al. Effects of prostaglandin E1, melatonin, and oxytetracycline on lipid peroxidation, antioxidant defense system, peroxonase (PON1) activities, and homocysteine levels in an animal model of spinal cord injury. Spine 2003; 28: 1643–1652.
Genovese T, Mazzon E, Muia C, Bramanti P, De Sarro A, Cuzzocrea S . Attenuation in the evolution of experimental spinal cord trauma by treatment with melatonin. J Pineal Res 2005; 38: 198–208.
Li Y, Jiang DH, Wang MI, Jiao Pang SF . Rhythms of serum melatonin in patients with spinal lesions at the cervical, thoracic or lombar region. Clin Endocrinol (Oxf) 1989; 30: 47–56.
Persengiev SP . The neuroprotective and antiapoptotic effects of melatonin in cerebellar neurons involve glucocorticoid receptor and p130 signal pathways. J Steroid Biochem Mol Biol 2001; 77: 151–158.
Reiter RJ, Tan DX, Poeggeler B, Menendez-Pelaez A, Chen LD, Searela S . Melatonin as a free radical scavenger: implications for aging and age-related diseases. Ann N Y Acad Sci 1994; 719: 1–12.
Reppert SM, Perlow MJ, Underleider LG, Mishkin M, Tamarkin L, Orloff DG et al. Effects of damage to the suprachiasmatic area of the anterior hypothalamus on the daily melatonin and cortisol rhythms in the rhesus monkey. J Neurosci 1981; 1: 1414–1425.
Antolin I, Rodriguez C, Sainz RM, Mayo JC, Uria H, Kotler ML et al. Neurohormone melatonin prevents cell damage: effect on gene expression for antioxidant enzymes. FASEB J 1996; 10: 882–890.
Pieri C, Marra M, Maroni F, Recchioni R, Marcheselli F . Melatonin: a peroxyl radical scavenger more effective than vitamin E. Life Sci 1994; 55: 271–276.
Rivlin AS, Tator CH . Effect of duration of acute spinal cord compression in a new acute cord injury model in the rat. Surg Neurol 1978; 10: 39–43.
Kennaway DJ, Voultsios A . Circadian rhythm of free melatonin in human plasma. J Clin Endocrinol Metab 1998; 83: 1013–1101.
Gündüz B . Daily rhythm in serum melatonin and leptin levels in the Syrian hamster (Mesocricetus auratus). Comp Biochem Physiol A Mol Integr Physiol 2002; 132: 393–401.
Klein DC . The mammalian melatonin rhythm generating system. In: Watterberg L (ed). Light and Biological Rhythms in Man. Pergamon Pres: New York, 1993, pp 55–70.
Kneisley LW, Moskovitz MA, Lynch HJ . Cervical spinal cord lesions disrupt the rhythm in human melatonin excretion. J Neural Transm 1978; 13 (Supp): 311–323.
Zeitzer JM, Ayas NT, Shea SA, Brown R, Czeisler CA . Absence of detactable melatonin and preservation of cortisol and thyrotropin rhythms in tetraplegia. J Clin Endocrinol Metab 2000; 85: 2189–2196.
Liu J, Tang T, Yang H, Xiao D . Antioxidation of melatonin against spinal cord injury in rats. Chin Med J 2004; 117: 571–575.
Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M et al. Methylprednisolone or trilazad mesylate administration after acute spinal cord injury. 1-year follows up. Results of the third National Acute Spinal Cord Injury randomized controlled trial. J Neurosurg 1998; 89: 699–706.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gezici, A., Karakaş, A., Ergün, R. et al. Rhythms of serum melatonin in rats with acute spinal cord injury at the cervical and thoracic regions. Spinal Cord 48, 10–14 (2010). https://doi.org/10.1038/sc.2009.73
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.73