Abstract
Study design:
Cross-sectional study.
Objectives:
To evaluate the physical activity scale for individuals with physical disabilities (PASIPD) in people with spinal cord injury (SCI).
Setting:
Eight Dutch rehabilitation centers with a specialized SCI unit.
Methods:
The PASIPD was examined by comparing group scores of people with different personal (age, gender and body mass index) and lesion characteristics (level (paraplegia/tetraplegia), completeness, time since injury (TSI)) in 139 persons with SCI 1 year after discharge from in-patient rehabilitation. Relationships between PASIPD scores and measures of activities (wheelchair skills, Utrecht Activity List, mobility range and social behavior subscales of the SIP68) and fitness (peak oxygen uptake, peak power output and muscular strength) were determined.
Results:
Persons with tetraplegia had significantly lower PASIPD scores than those with paraplegia (P<0.02). Persons with longer TSI had lower PASIPD scores than persons with shorter TSI (P<0.03). PASIPD scores showed moderate correlations with activities (0.36–0.51, P<0.01) and weak-to-moderate correlations with fitness parameters (0.25–0.36, P<0.05).
Conclusion:
In a fairly homogeneous group of persons with SCI, 1 year after in-patient rehabilitation, the PASIPD showed weak-to-moderate relationships with activity and fitness parameters. There seems to be a limited association between self-reported activity level and fitness in people with SCI.
Similar content being viewed by others
Introduction
After in-patient rehabilitation, individuals with a spinal cord injury (SCI) have the lowest level of physical activity compared with other populations with a disability,1 as measured with a body-worn activity monitor. The people with a SCI who are active have a higher physical capacity than sedentary people with a SCI.2 Furthermore, being physically active and fit appears to be associated with several health benefits in persons with SCI.3 Therefore, it is important to promote a physically active lifestyle in people with SCI to prevent secondary complications. To determine the level of active lifestyle and to evaluate the effect of lifestyle interventions, a reliable and valid measure of physical activity for people with SCI is needed.
The physical activity scale for individuals with physical disabilities (PASIPD) was developed to assess the self-reported physical activity level of individuals with a disability.4 The PASIPD was evaluated in people with different physical disabilities.4, 5 Support was found in these studies for the construct validity, reliability and criterion validity of the PASIPD.4, 5 However, the PASIPD has not yet been evaluated in specific disability groups such as people with SCI. Therefore, the purpose of this study is to evaluate the PASIPD in people with SCI.
Methods
Participants
The current cross-sectional study was part of the Dutch prospective cohort study ‘Physical strain, work capacity and mechanisms of restoration of mobility in the rehabilitation of persons with SCI’. Participants from eight rehabilitation centers that are specialized in SCI rehabilitation in the Netherlands were included. They were eligible to enter the project if they had an acute SCI, were between 18 and 65 years of age, were classified as A, B, C or D on the American Spinal Injury Association impairment scale, were (partly) wheelchair dependent, did not have a progressive disease or psychiatric problem, and had sufficient understanding of the Dutch language to understanding the purpose of the study and the testing methods.
All tests and protocols were approved by the medical ethics committee of the rehabilitation center Hoensbroek. After they were given information regarding the testing procedure, all participants completed an informed consent form.
Design
Data for this study were collected 1 year after discharge from in-patient rehabilitation by trained research assistants with a paramedical background using standard procedures and equipment.
Personal and lesion characteristics
Participant information regarding age, gender, level and completeness of the lesion were collected. Time since injury (TSI) was determined as the time between the occurrence of SCI and the measurement date on which the PASIPD was filled out. Height and weight were measured to calculate the body mass index (BMI, in kg m–2).
Physical activity scale for individuals with physical disabilities
Information on level of physical activity (leisure, household and occupational activity) was collected using the PASIPD.4 The PASIPD consists of 13 questions. The first item was included only to familiarize respondents with the item format and was not scored. Two of these questions, question 10 on lawn work or yard care, and question 11 on outdoor gardening, were merged into a single question, because this better represented the Dutch situation. The 11 remaining questions were filled out to obtain the total physical activity score, which is expressed in metabolic equivalent (MET in h day−1, maximum score is 182.3 MET h day−1 (after combining question 10 and 11) and 199.5 MET h day−1 in the original PASIPD). One MET is defined as the amount of oxygen required per minute under quiet resting conditions.
Outcome measures activities
The Wheelchair Circuit6 was performed. All eight tasks that were performed adequately, independently and within a certain time were assigned one point. All points were summed to get an overall ability score, ranging from 0 to 8. The performance time score is the sum of the performance times of the figure-of-8 shape and the 15-m sprint, which were performed at maximum speed.
The Utrecht activities list (UAL)7 was used to assess the time spent on vocational and leisure activities such as work, study, voluntary work, hobbies and sports activities, in hours per week. This questionnaire is a Dutch adaptation of the Craig Handicap Assessment and Reporting Technique.8
The sum of the subscales Mobility Range and Social Behavior of the SIP68 (SIPSOC) was used to assess perceived limitations in participation.6
Outcome measures physical capacity
To determine peak aerobic power output and peak oxygen consumption subjects performed a standardized graded peak wheelchair exercise test on a motor-driven treadmill according to a standardized protocol.9 Metabolic cost was continuously measured during the exercise blocks with a metabolic cart (Oxycon Delta, Jaeger, Germany). The peak oxygen consumption (VO2peak; l min−1) was defined as the highest oxygen uptake value over 30 s during the test. POpeak was defined by the power output, which corresponded to the highest slope maintained for at least 30 s.9
To determine the strength of the upper extremity, the shoulder abductors, internal and external rotators, elbow flexors and extensors, and wrist extensors in both arms were tested with the manual muscle test (MMT). The strength was rated on a scale ranging from 0 to 5. Summing the scores of the 12 muscle groups gave a MMT sum score (range: 0–60). The muscle groups (with exception of the wrist extensors) that scored 3 or greater on the MMT were tested with handheld dynamometry. The maximum force (in Newton) of the 10 muscle groups was summed. Both tests were performed according to a standardized protocol.9
Statistics
Descriptive statistics for personal and lesion characteristics, physical capacity, activity parameters and the PASIPD were calculated.
A factor analysis was performed to determine whether item responses loaded on the same dimensions as those found in a group with diverse disabilities.4 The items expressed in MET h day−1 were used in the factor analysis. An 11-item inter-correlation matrix was computed, which was used for a factor analysis with principal component extraction and oblique rotations. Factor determination was based on the criteria: an eigenvalue ⩾1 and a factor loading ⩾0.40, without loading on more than one factor. Cronbach's alpha was calculated to determine the internal consistency of the PASIPD.
Furthermore, the group was divided, based on the median split, in respectively three groupings with two categories each: young–old age, low–high BMI and short–long TSI. Thereafter, PASIPD scores of people with different personal (age, gender and BMI) and lesion characteristics (paraplegia/tetraplegia, motor complete–incomplete and TSI) were compared with a non-parametric Mann–Whitney test. The effect size was calculated.
Spearman correlation coefficients were calculated to determine the associations among the PASIPD items, PASIPD total score and the outcome measures of activities (wheelchair performance time and ability score, UAL, SIPSOC) and physical capacity (POpeak, VO2peak, MMT and handheld dynamometry). Correlations between the PASIPD items and the activity and physical capacity variables that should measure the same construct were of specific interest. A correlation coefficient ⩾0.6 was considered to be strong, moderate when between 0.3 and 0.6, and weak if the coefficient was ⩽0.3.10
Results
Descriptives
Of the total group, 73% were male, 68% had a paraplegia and 64% had a complete lesion. The participants were on average 41.6±14.1 years, with a mean BMI of 24.5±4.5 kg m−2 and a TSI of 705±169 days. The descriptives of the PASIPD, activity and physical capacity parameters are shown in Table 1. Some activities, such as wheeling outside, are performed often by the majority of participants while more than 70% of the participants never performed activities such as heavy housework, lawn work and paid work (Figure 1).
Factor analysis
Table 2 shows the mean score of each item and the results of the factor analysis. The Cronbach α for the PASIPD total score was 0.63. Wheeling outside correlated best with the total PASIPD score followed by moderate and strenuous sport or recreational activities. Four factors were identified: light–moderate activities and muscle strength training (factor 1), light and heavy housework (factor 2), home repair and lawn work (factor 3) and care for another person, paid work, wheeling outside and strenuous activities (factor 4). A majority of the variance was explained by factor 1 (26%), that is, light–moderate activities and muscle strength training. All four factors combined accounted for approximately 62% of the total item variance.
Differences between groups
Persons with a tetraplegia or long TSI (long: TSI>672 days) had significantly lower PASIPD scores compared with those with paraplegia (P=0.02; effect size: 0.17) or those with a short TSI (P=0.03; effect size: 0.30). A partial correlation showed that the relationship between TSI and the PASIPD score was not confounded by level of injury.
The lesion characteristic completeness of the lesion did not lead to a significantly different PASIPD score (P=0.97; effect size: 0.04). Similar results were found for the personal characteristics age (old: age >40.8 years; P=0.16; effect size: 0.33), gender (P=0.96; effect size: 0.02), and BMI (high: BMI >24.7 kg m−2; P=0.59; effect size: 0.08).
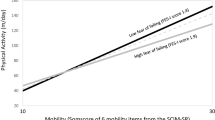
Associations with activities and physical capacity
Moderate correlations were found between the PASIPD total score and activities (0.36–0.51, P<0.01) (Table 3). PASIPD total score showed weak correlations with most physical capacity parameters (r=0.15–0.29), except for the MMT sum score that showed a moderate correlation (r=0.35) (Table 3).
Mostly moderate correlations were found between the PASIPD items and the activity and physical capacity parameters that should measure the same construct (Table 3). A strong correlation (r=0.62) was found between strenuous sport or recreational activities and the number of hours per week a persons participates in sport activities (measured by the UAL) (Table 3). In contrast, weak correlations were found between light and moderate sport or recreational activities and VO2peak or POpeak, and between muscle strength training and muscle strength measured by MMT or handheld dynamometry (Table 3).
Discussion
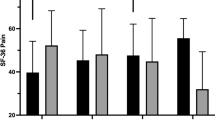
Many activities were never performed by more than 70% of the group, leading to the low PASIPD score. PASIPD scores were significantly different between persons with a tetraplegia and paraplegia. Also a significant difference was found between those with a short and long TSI. The PASIPD score did not discriminate between those with a young–old age, low–high BMI and male–female despite the fact that in the literature a difference in activity levels between these groups was found.4 The PASIPD seems to discriminate between groups of people with different disabilities. The average total PASIPD score (17.8 MET h day−1) was comparable to that of other studies that included mostly persons with SCI or elderly with chronic conditions (PASIPD scores varied between 11.0 and 36.3 MET h day−1)4, 11, 12, 13, 14, 15, 16 (Figure 2). This study used 11 items in contrast to the other studies (12 items). However, one extra item would raise the score to a roughly estimated (17.8/11) × 12=19.4, which also lies in the mentioned range. Van der Ploeg et al.5 found much higher scores in 46 participants with a disability (74.9 MET h day−1) (Figure 2). This might be explained by the inclusion of people with less severe disabilities such as chronic pain, whiplash and back disorders.5 In general, low PASIPD scores are found in people with a disability taking the maximal score into account (182.5–199.5 MET h day−1 dependent on the number of items included).
Average physical activity scale for individuals with physical disabilities (PASIPD) total score found in the literature for different populations. The study of Gutierrez et al. (2007) only gave the median PASIPD score. The present study and the study of Van der Ploeg5 used the 11 items PASIPD questionnaire in contrast to the other studies (12 items).
The internal consistency of the PASIPD was weak (Cronbach α=0.63)10 in our group with SCI. This low alpha might be explained by the complementary activities in the PASIPD, that is, if you perform some activities then you have less time and energy to perform other activities. Factor analysis showed four dimensions of the PASIPD in this group. The item strenuous activities were, together with the item care for another person, clustered with the factor ‘occupation’ (paid work and wheeling outside). It is hard to classify this fourth factor into a specific category because of the very diverse items. It might be that in this group with a SCI these items are not properly phrased or applicable and, therefore, fall in another dimension then what was found earlier in a group with all kind of disabilities using the 12 items PASIPD.4 However, the percentage of variance explained in both studies was comparable (around 62%).
The PASIPD correlated moderately (r=0.51) with the UAL, which also measures self-reported activities. The UAL is reported in hours per week while the PASIPD estimated MET expenditure. The correlation between the PASIPD and the SIPSOC was also moderate (r=0.47). The questions of the SIPSOC focus on the limitations experienced in mobility range and social behavior and are, therefore, quite different from the PASIPD questions that measure the activity level. Furthermore, not every item of the SIPSOC or UAL relates to one or more items of the PASIPD. The expectation was that the PASIPD would correlate better with activity data measured by accelerometry, however, low correlation coefficients (r=0.30) were found in non-wheelchair-dependent persons with a physical disability.5
Weak-to-moderate relationships between the PASIPD total score and the physical capacity parameters were found. Although the expectation was that those with a high activity level measured by the PASIPD would have a better fitness, these variables do not measure exactly the same concepts and correlation coefficients will not be very high. The correlation coefficients between the items of the PASIPD and fitness or activity items that measure the same concept showed higher values (up to 0.62) but also very low coefficients were found (for example, muscle strength, 0.03–0.09). These low-to-moderate correlations might be due to the homogeneity of our group with a SCI, which has a low PASIPD score. With a restricted range of scores, the correlation will be reduced.
Two other self-reported activity scales for people with disabilities came available after the Dutch prospective cohort study started; the physical acitivity and disability survey17 and the physical activity recall assessment for people with spinal cord injury.18 The validity of the physical acitivity and disability survey was evaluated in individuals with disabilities and/or chronic health conditions and showed similar low correlations with peak VO2 (r=0.23), maximum work load (r=0.18) and exhaustion (r=0.23)17 as this study. In contrast the physical activity recall assessment for people with spinal cord injury showed quite strong correlation coefficients with the percentage VO2 reserve (the difference between resting and maximal VO2), that is, 0.63 for moderate intensity activities, 0.88 for heavy intensity activities and 0.79 for total activities. However, the correlations with mild intensity activities (r=0.27)18 as well as with VO2peak (r=0.21) and muscle strength of the biceps (r=0.15) and chest (r=0.16) were low.19 To analyze which of the three self-reported activity scales (PASIPD, physical activity recall assessment for people with spinal cord injury and physical acitivity and disability survey) is most useful in studying physical activity in people with SCI, a future study should compare these three scales in the same group and relate them to fitness and objective activity measures. Objective activity measures, such as motion sensors, do not always relate strongly to fitness parameters.20 Therefore, it would also be interesting to analyze whether objective activity measures (for example, doubly labeled water, activity monitor and oxygen uptake) relate to fitness and self-reported activity in people with SCI. On the basis of the above-mentioned results, the physical activity recall assessment for people with spinal cord injury might have the most potential to be used in people with SCI because it has been developed specifically for that population and shows good correlations with moderate-to-heavy intensity activities.
Conclusion
The PASIPD showed a moderate relationship with activity parameters and weak-to-moderate relationship with fitness measures in people with SCI. In general, there seems to be a limited association between self-reported activity level, fitness and objective measures of activity.
References
van den Berg-Emons RJ, Bussmann JB, Haisma JA, Sluis TA, Van Der Woude LH, Bergen MP et al. A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil 2008; 89: 2094–2101.
Muraki S, Tsunawake N, Tahara Y, Hiramatsu S, Yamasaki M . Multivariate analysis of factors influencing physical work capacity in wheelchair-dependent paraplegics with spinal cord injury. Eur J Appl Physiol 2000; 81: 28–32.
Fernhall B, Heffernan K, Jae SY, Hedrick B . Health implications of physical activity in individuals with spinal cord injury: a literature review. J Health Hum Serv Adm 2008; 30: 468–502.
Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF . The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil 2002; 83: 193–200.
van der Ploeg HP, Streppel KR, van der Beek AJ, van der Woude LH, Vollenbroek-Hutten M, van MW . The Physical Activity Scale for Individuals with Physical Disabilities: test-retest reliability and comparison with an accelerometer. J Phys Act Health 2007; 4: 96–100.
Kilkens OJ, Post MW, Dallmeijer AJ, van Asbeck FW, Van Der Woude LH . Relationship between manual wheelchair skill performance and participation of persons with spinal cord injuries 1 yr after discharge from inpatient rehabilitation. J Rehabil Res Dev 2005; 42 (3 Suppl 1): 65–73.
van Asbeck FWA . Handboek Dwarslaesierevalidatie. Bohn Stafleu Van Loghum: Houten, 2007.
Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN . Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil 1992; 73: 519–526.
Haisma JA, Bussmann JB, Stam HJ, Sluis TA, Bergen MP, Dallmeijer AJ et al. Changes in physical capacity during and after inpatient rehabilitation in subjects with a spinal cord injury. Arch Phys Med Rehabil 2006; 87: 741–748.
Visser-Meily JM, Post MW, Riphagen II, Lindeman E . Measures used to assess burden among caregivers of stroke patients: a review. Clin Rehabil 2004; 18: 601–623.
Ellis R, Kosma M, Cardinal BJ, Bauer JJ, McCubbin JA . Physical activity beliefs and behaviour of adults with physical disabilities. Disabil Rehabil 2007; 29: 1221–1227.
Giacobbi Jr PR, Stancil M, Hardin B, Bryant L . Physical activity and quality of life experienced by highly active individuals with physical disabilities. Adapt Phys Activ Q 2008; 25: 189–207.
Gutierrez DD, Thompson L, Kemp B, Mulroy SJ . The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med 2007; 30: 251–255.
Liu-Ambrose T, Ashe MC, Marra C, Conditions Research Team. Among older adults with multiple chronic conditions, physical activity is independently and inversely associated with health care utilization. Br J Sports Med 2008 (e-pub ahead of print 12 June 2008).
Pang MY, Eng JJ, Dawson AS, McKay HA, Harris JE . A community-based fitness and mobility exercise program for older adults with chronic stroke: a randomized, controlled trial. J Am Geriatr Soc 2005; 53: 1667–1674.
Stevens SL, Caputo JL, Fuller DK, Morgan DW . Physical activity and quality of life in adults with spinal cord injury. J Spinal Cord Med 2008; 31: 373–378.
Rimmer JH, Riley BB, Rubin SS . A new measure for assessing the physical activity behaviors of persons with disabilities and chronic health conditions: the Physical Activity and Disability Survey. Am J Health Promot 2001; 16: 34–42.
Ginis KA, Latimer AE, Hicks AL, Craven BC . Development and evaluation of an activity measure for people with spinal cord injury. Med Sci Sports Exerc 2005; 37: 1099–1111.
Latimer AE, Ginis KA, Craven BC, Hicks AL . The physical activity recall assessment for people with spinal cord injury: validity. Med Sci Sports Exerc 2006; 38: 208–216.
Shephard RJ . Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med 2003; 37: 197–206.
Acknowledgements
We thank the eight participating rehabilitation centers and especially the research assistants for collecting all the data: Sacha van Langeveld (De Hoogstraat, Utrecht), Peter Luthart (Rehabilitation Center Amsterdam), Marijke Schuitemaker (Het Roessingh, Enschede), Karin Postma (Rijndam Revalidatiecentrum, Rotterdam), Jos Bloemen (Hoensbroeck Revalidatiecentrum, Hoensbroek), Hennie Rijken (Sint Maartenskliniek, Nijmegen), Ferry Woldring (Beatrixoord, Haren) and Linda Valent (Heliomare, Wijk aan Zee). This study was supported by the Dutch Health Research and Development Council, Zon-Mw Rehabilitation program, grant no. 1435.0003 and 1435.0025.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
de Groot, S., van der Woude, L., Niezen, A. et al. Evaluation of the physical activity scale for individuals with physical disabilities in people with spinal cord injury. Spinal Cord 48, 542–547 (2010). https://doi.org/10.1038/sc.2009.178
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.178
Keywords
This article is cited by
-
Exercise intensity during exergaming in wheelchair-dependent persons with SCI
Spinal Cord (2023)
-
Electrical stimulation to prevent recurring pressure ulcers in individuals with a spinal cord injury compared to usual care: the Spinal Cord Injury PREssure VOLTage (SCI PREVOLT) study protocol
Trials (2022)
-
Predicting resting energy expenditure in people with chronic spinal cord injury
Spinal Cord (2022)
-
The neurological level of spinal cord injury and cardiovascular risk factors: a systematic review and meta-analysis
Spinal Cord (2021)
-
Leisure time physical activity participation in individuals with spinal cord injury in Malaysia: barriers to exercise
Spinal Cord (2018)