Abstract
Study design:
Systematic review.
Background:
The applied definition of traumatic central cord syndrome (TCCS) lacks specific quantified diagnostic criteria.
Objective:
To review currently applied TCCS diagnostic criteria and quantitative data regarding the ‘disproportionate weakness’ between the upper and lower extremities described in original studies reporting on TCCS subjects.
Methods:
A MEDLINE (1966 to 2008) literature search was conducted. The descriptors applied to define TCCS were extracted from all included articles. We included original studies that reported on the differences in motor score (based on the Medical Research Council scale) between the total upper extremity motor score (UEMS) and the total lower extremity motor score (LEMS), in a minimum of five TCCS patients at the time of hospital admission. The mean difference between the total UEMS and the total LEMS of the patients included in each study was calculated. Case reports were excluded.
Results:
None of the identified studies on TCCS patients reported inclusion and/or exclusion criteria using a quantified difference between the UEMS and LEMS. Out of 30 retrieved studies, we identified seven different clinical descriptors that have been applied as TCCS diagnostic criteria. Nine studies reporting on a total of 312 TCCS patients were eligible for analysis. The mean total UEMS was 10.5 motor points lower than the mean total LEMS.
Conclusions:
There is no consensus on the diagnostic criteria for TCCS. Nevertheless, this review revealed an average of 10 motor points between the UEMS and LEMS as a possible TCCS diagnostic criterion. However, further discussion by an expert panel will be required to establish definitive diagnostic criteria.
Similar content being viewed by others
Introduction
Traumatic central cord syndrome (TCCS) is a clinical diagnosis that was first described by Schneider et al. in 1954.1 TCCS is characterized by (1) a disproportionate impairment (weakness and reduced function) of the upper limbs as compared with the lower limbs, (2) neurogenic bladder dysfunction, and (3) varying degrees of sensory loss at and below the level of the lesion.1 A TCCS is considered the most prevalent incomplete spinal cord injury (SCI) syndrome, accounting for ∼9% of all traumatic SCI's.2, 3 In TCCS patients, recovery of a certain degree of ambulation, participation in daily life activities, bowel and bladder function has been reported to be favorable in several studies.2, 3, 4, 5, 6, 7, 8, 9, 10
TCCS also occurs frequently in elderly subjects due to rather minor spine trauma (hyperextension injury) based on underlying cervical spondylosis. The pathophysiological mechanisms inducing the TCCS are probably multimodal. One hypothesis is that a spinal cord compression occurs between bony spurs anteriorly and buckling of the ligamentum flavum posteriorly.1, 11 This cord compression may cause direct damage of neural structures located in the central gray matter and/or attenuation of the segmental blood supply. These mechanisms affect the cervical enlargement at the levels of the alpha motor neurons supplying predominantly hand muscles and to a lesser extent fibers of the corticospinal tracts (CSTs). Such a pattern of injury that spares the descending CSTs but damages the alpha motor neurons is assumed to result in a syndrome of disproportionate arm and leg weakness.12 An alternative hypothesis is that the TCCS results from an injury to the CSTs. The CST tends to produce relatively greater dysfunction in the hand and arms than in the legs, as the main function of the CST is to support fine motor movements in the distal musculature, especially of the upper limbs.13, 14
Since the introduction of the TCCS diagnostic criteria more than five decades ago, it has been one of the most frequently cited definitions of an incomplete SCI syndrome.3 However, the TCCS lacks uniform and broadly accepted diagnostic criteria. In other words, the diagnosis of TCCS is based on non-specific criteria and interpretation of physical examination. Therefore, the utility of currently applied TCCS diagnostic criteria can be considered as limited.
The primary objective of this review was to investigate the current literature on applied TCCS diagnostic criteria. The secondary objective was to analyze the quantitative differences between the total upper extremity motor score (UEMS) and the total lower extremity motor score (LEMS) described in these original studies.
Methods
Retrieval of publications
All clinical studies reporting on TCCS were eligible for this review. Case reports were excluded in this review. A MEDLINE (PubMed interface) search was performed to compile a reference list of articles published between 1966 and November 2008 identified by the following keywords: SCI, central cord syndrome, cruciate paralysis, incomplete SCI, spinal cord syndromes, ASIA motor score, LEMS, UEMS, and cervical spondylosis. Furthermore, the retrieved list of references was manually checked for additional studies potentially meeting the inclusion criteria.
Analysis of applied TCCS diagnostic criteria
All retrieved original studies reporting on TCCS patients, irrespective of whether the total UEMS and LEMS were reported, were analyzed with regard to the TCCS diagnostic criteria applied. All descriptors used to define the TCCS were extracted from the included articles.
Analysis of scores
To calculate the mean difference between the total UEMS and total LEMS, we included only original studies that reported on the total UEMS and total LEMS (based on the Medical Research Council scale), for a minimum of five TCCS patients, on their admission to the hospital. Each study's reported difference between the total UEMS and LEMS in TCCS patients was recorded to identify which difference in motor loss the authors regarded as a ‘disproportionate impairment of the upper limbs as compared with the lower limbs.’ To calculate these ‘disproportionate’ differences, the mean differences between the total UEMS and LEMS were multiplied by the number of patients reported in each study. These numbers were added and divided by the total number of pooled patients.
Results
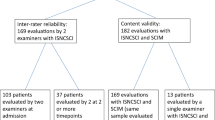
Out of 177 articles from MEDLINE identified by the predefined keywords, only 30 studies could be accepted after accounting for the inclusion/exclusion criteria. In these 30 articles, seven different clinical descriptors were provided that have been applied as criteria to diagnose TCCS (Table 1).
As the UEMS and LEMS were not reported in TCCS patients, 21 studies,1, 2, 3, 4, 7, 8, 9, 14, 18, 19, 20, 22, 23, 24, 27, 28, 29, 30, 31, 32, 33 were excluded in the analysis of the scores. Out of the 30 retrieved studies, nine studies5, 6, 10, 15, 16, 17, 21, 25, 26 that reported the UEMS and LEMS at admission were included in our analysis. In two articles,6, 21 a scatter diagram6 and a bar graph21 were used to determine the UEMS and LEMS. An overview of the studies included for analysis is shown in Table 2. Furthermore, no study on TCCS patients was identified that reported inclusion and/or exclusion criteria using a quantified difference between the UEMS and LEMS.
Differences in motor scores between the upper and lower extremities
Guest et al.16 investigated the neurological outcome in 50 patients who underwent early (⩽24 h after injury) or late (>24 h after injury) surgery. The preoperative mean difference between the UEMS and LEMS of these 50 patients was 10.1 motor points. Another retrospective study21 reported on the long-term outcome in 32 conservatively treated patients with symptoms consistent with the TCCS. Patients were divided by age into three groups. In this study, the mean difference between the UEMS and LEMS of these three groups was 15.9 motor points.21 Tow and Kong10 reported the UEMS and LEMS at admission in patients who were identified to have greater weakness of the upper than the lower extremities. In 73 TCCS patients, a mean difference of nine motor points was identified. Another retrospective study5 assessed the improvement in ASIA motor score in 70 TCCS patients. This study5 identified a mean difference between the UEMS and LEMS of 6.8 motor points. Waters et al.26 identified a mean difference between the UEMS and LEMS of 11.1 motor points in a prospective study reporting on nine patients with TCCS. The study by Ishida and Tominaga6 examined neurological recovery in 22 TCCS patients. Only patients with an LEMS of 50 were included. The mean difference between the UEMS and LEMS in this study was 17.8 motor points.
Three studies15, 17, 25 evaluated the radiological findings in TCCS patients. In 15 patients, Miranda et al.17 identified a mean difference between the UEMS and LEMS of 8.6 motor points. Collignon et al.15 performed a retrospective study of 18 TCCS patients to assess the presence of intramedullary blood in the spinal cord. The mean difference identified between the UEMS and LEMS was 10.3 motor points. Another study25 evaluated the value of radiological findings in 23 TCCS patients. We identified a mean difference between the UEMS and LEMS of 13.4 motor points.
Analysis
We calculated the mean difference between the total UEMS and total LEMS for the nine studies5, 6, 10, 15, 16, 17, 21, 25, 26 depicted in Table 2. This analysis showed that in 312 TCCS patients, the mean total UEMS was 10.5 (range, 6.8–17.8) motor points lower than the mean total LEMS.
Discussion
In this review, seven different descriptors to define the TCCS were identified among 30 retrieved articles. Furthermore, no study on TCCS patients reported inclusion and/or exclusion criteria regarding a quantified difference between the UEMS and LEMS. Our analysis showed that out of the 312 pooled subjects with TCCS, the mean total UEMS was ∼10 motor points lower than the mean total LEMS.
The currently applied TCCS diagnostic criteria can be interpreted broadly, so that patients with incomplete tetraplegia are diagnosed with TCCS and vice versa. As quantified, diagnostic criteria for TCCS are lacking, and the incidence of TCCS can be expected to increase in SCI patients older than 60 years.34 Thus, it is necessary to define not only univocal TCCS diagnostic criteria, but also a quantified difference between the UEMS and LEMS.
Quantifying the term ‘disproportionate’ to a specific minimum of motor points could lead to a more adequate and reliable TCCS diagnosis. In addition, TCCS diagnostic criteria would also be valuable for research purposes. If quantified TCCS diagnostic criteria are applied, investigators would be able to stratify and constrain the heterogeneity of SCI patient samples. This is important, as TCCS patients probably have a favorable recovery pattern compared with incomplete tetraplegia.2, 3, 4, 5, 6, 7, 8, 9, 10 In future SCI trials, analyzing outcome data for TCCS patients as a separate group could be important for a more sensitive detection of treatment effects.
Although Schneider et al.1 reported bladder dysfunction to be a characteristic of TCCS, the International Standards for Neurological and Functional Classification of Spinal Cord Injury Patients35 did not include the presence of bladder dysfunction as a diagnostic criterion for TCCS. Therefore, the analysis of the scores in our review has been focused on the difference between the total UEMS and the total LEMS.
As a ‘disproportionate’ weakness of the arms with better (or normal) strength in the legs can occur in both TCCS and cruciate paralysis,36, 37 we also searched for articles in which patients with cruciate paralysis were described. Cruciate paralysis is characterized by an isolated injury to the cervicomedullary junction that results in paralysis of the arms with minimal or absent lower extremity involvement.37, 38 The pathophysiology is based on neuroanatomy: the motor tract of the upper extremities crosses rostrally in the cervicomedullary junction, whereas that of the lower extremities crosses caudally in the superior cervical spinal cord.37, 39, 40 Despite the fact that TCCS and cruciate paralysis have been reported separately in the literature, it is suggested that both syndromes are expressions of the same mechanism rather than two separate entities based on damage to the pyramidal crossing arm fibers.40 As the clinical presentations of TCCS and cruciate paralysis are comparable, and we were only interested in the quantitative details of the difference between the upper and lower extremity motor scores, TCCS and cruciate paralysis were grouped in our analysis.36
In one of our earlier studies,41 we decided to define TCCS as a total LEMS of 10 or more points higher than the total UEMS. Although no study was identified that reported inclusion and/or exclusion criteria using a quantified difference between the UEMS and LEMS, Hayes et al.23 described an approach to classify patients with incomplete SCI according to SCI syndromes. In this study,23 the choice was made to diagnose TCCS based on a total LEMS of five or more points higher than the total UEMS. However, both proposals were arbitrary and had not been validated earlier.23, 41
Conclusion
To our knowledge, no study on TCCS patients reported inclusion and/or exclusion criteria using a quantified difference between the UEMS and LEMS. In addition, seven different clinical descriptors were identified that have been applied as criteria to diagnose TCCS. This study is a first attempt to provide a quantified approach to determine whether an incomplete SCI can be labeled as TCCS. Our analysis showed that out of the 312 pooled subjects with TCCS, the mean total UEMS was ∼10 motor points lower than the mean total LEMS.
Further discussion by an expert panel will be required to establish definitive diagnostic criteria for TCCS.
References
Schneider RC, Cherry G, Pantek H . The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine. J Neurosurg 1954; 11: 546–577.
Bosch A, Stauffer ES, Nickel VL . Incomplete traumatic quadriplegia. A ten-year review. JAMA 1971; 216: 473–478.
McKinley W, Santos K, Meade M, Brooke K . Incidence and outcomes of spinal cord injury clinical syndromes. J Spinal Cord Med 2007; 30: 215–224.
Aito S, D'Andrea M, Werhagen L, Farsetti L, Cappelli S, Bandini B et al. Neurological and functional outcome in traumatic central cord syndrome. Spinal Cord 2007; 45: 292–297.
Dvorak MF, Fisher CG, Hoekema J, Boyd M, Noonan V, Wing PC et al. Factors predicting motor recovery and functional outcome after traumatic central cord syndrome: a long-term follow-up. Spine 2005; 30: 2303–2311.
Ishida Y, Tominaga T . Predictors of neurologic recovery in acute central cervical cord injury with only upper extremity impairment. Spine 2002; 27: 1652–1658.
Merriam WF, Taylor TK, Ruff SJ, McPhail MJ . A reappraisal of acute traumatic central cord syndrome. J Bone Joint Surg Br 1986; 68: 708–713.
Penrod LE, Hegde SK, Ditunno Jr JF . Age effect on prognosis for functional recovery in acute, traumatic central cord syndrome. Arch Phys Med Rehabil 1990; 71: 963–968.
Roth EJ, Lawler MH, Yarkony GM . Traumatic central cord syndrome: clinical features and functional outcomes. Arch Phys Med Rehabil 1990; 71: 18–23.
Tow AM, Kong KH . Central cord syndrome: functional outcome after rehabilitation. Spinal Cord 1998; 36: 156–160.
Parke WW . Correlative anatomy of cervical spondylotic myelopathy. Spine 1988; 13: 831–837.
Eidelberg E . Consequences of spinal cord lesions upon motor function, with special reference to locomotor activity. Prog Neurobiol 1981; 17: 185–202.
Levi AD, Tator CH, Bunge RP . Clinical syndromes associated with disproportionate weakness of the upper versus the lower extremities after cervical spinal cord injury. Neurosurgery 1996; 38: 179–183.
Quencer RM, Bunge RP, Egnor M, Green BA, Puckett W, Naidich TP et al. Acute traumatic central cord syndrome: MRI-pathological correlations. Neuroradiology 1992; 34: 85–94.
Collignon F, Martin D, Lenelle J, Stevenaert A . Acute traumatic central cord syndrome: magnetic resonance imaging and clinical observations. J Neurosurg 2002; 96: 29–33.
Guest J, Eleraky MA, Apostolides PJ, Dickman CA, Sonntag VK . Traumatic central cord syndrome: results of surgical management. J Neurosurg 2002; 97: 25–32.
Miranda P, Gomez P, Alday R . Acute traumatic central cord syndrome: analysis of clinical and radiological correlations. J Neurosurg Sci 2008; 52: 107–112.
Chen L, Yang H, Yang T, Xu Y, Bao Z, Tang T . Effectiveness of surgical treatment for traumatic central cord syndrome. J Neurosurg Spine 2009; 10: 3–8.
Saruhashi Y, Hukuda S, Katsuura A, Asajima S, Omura K . Clinical outcomes of cervical spinal cord injuries without radiographic evidence of trauma. Spinal Cord 1998; 36: 567–573.
Yamazaki T, Yanaka K, Fujita K, Kamezaki T, Uemura K, Nose T . Traumatic central cord syndrome: analysis of factors affecting the outcome. Surg Neurol 2005; 63: 95–99.
Newey ML, Sen PK, Fraser RD . The long-term outcome after central cord syndrome: a study of the natural history. J Bone Joint Surg Br 2000; 82: 851–855.
Noonan VK, Kopec JA, Zhang H, Dvorak MF . Impact of associated conditions resulting from spinal cord injury on health status and quality of life in people with traumatic central cord syndrome. Arch Phys Med Rehabil 2008; 89: 1074–1082.
Hayes KC, Hsieh JT, Wolfe DL, Potter PJ, Delaney GA . Classifying incomplete spinal cord injury syndromes: algorithms based on the International Standards for Neurological and Functional Classification of Spinal Cord Injury Patients. Arch Phys Med Rehabil 2000; 81: 644–652.
Chen TY, Lee ST, Lui TN, Wong CW, Yeh YS, Tzaan WC et al. Efficacy of surgical treatment in traumatic central cord syndrome. Surg Neurol 1997; 48: 435–440.
Song J, Mizuno J, Inoue T, Nakagawa H . Clinical evaluation of traumatic central cord syndrome: emphasis on clinical significance of prevertebral hyperintensity, cord compression, and intramedullary high-signal intensity on magnetic resonance imaging. Surg Neurol 2006; 65: 117–123.
Waters RL, Adkins RH, Sie IH, Yakura JS . Motor recovery following spinal cord injury associated with cervical spondylosis: a collaborative study. Spinal Cord 1996; 34: 711–715.
Bose B, Northrup BE, Osterholm JL, Cotler JM, Ditunno JF . Reanalysis of central cervical cord injury management. Neurosurgery 1984; 15: 367–372.
Brodkey JS, Miller Jr CF, Harmody RM . The syndrome of acute central cervical spinal cord injury revisited. Surg Neurol 1980; 14: 251–257.
Dai L, Jia L . Central cord injury complicating acute cervical disc herniation in trauma. Spine 2000; 25: 331–335.
Pollard ME, Apple DF . Factors associated with improved neurologic outcomes in patients with incomplete tetraplegia. Spine 2003; 28: 33–39.
Song J, Mizuno J, Nakagawa H, Inoue T . Surgery for acute subaxial traumatic central cord syndrome without fracture or dislocation. J Clin Neurosci 2005; 12: 438–443.
Uribe J, Green BA, Vanni S, Moza K, Guest JD, Levi AD . Acute traumatic central cord syndrome—experience using surgical decompression with open-door expansile cervical laminoplasty. Surg Neurol 2005; 63: 505–510.
Weingarden SI, Graham PM . Falls resulting in spinal cord injury: patterns and outcomes in an older population. Paraplegia 1989; 27: 423–427.
www.spinalcord.uab.edu. Facts and Figures at a Glance. National Spinal Cord Injury Statistical Center: Birmingham, Alabama. 2008.
Maynard Jr FM, Bracken MB, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Hatzakis Jr MJ, Bryce N, Marino R . Cruciate paralysis, hypothesis for injury and recovery. Spinal Cord 2000; 38: 120–125.
Inamasu J, Hori S, Ohsuga F, Aikawa N . Selective paralysis of the upper extremities after odontoid fracture: acute central cord syndrome or cruciate paralysis? Clin Neurol Neurosurg 2001; 103: 238–241.
Bell HS . Paralysis of both arms from injury of the upper portion of the pyramidal decussation: “cruciate paralysis”. J Neurosurg 1970; 33: 376–380.
Ciappetta P, Salvati M, Raco A, Artico M . Cruciate hemiplegia: a clinical syndrome, a neuroanatomical controversy. Report of two cases and review of the literature. Surg Neurol 1990; 34: 43–47.
Kuitwaard K, Vandertop WP . A patient with an odontoid fracture and atrophy of the tongue: a case report and systematic review of the literature. Surg Neurol 2005; 64: 525–532 discussion.
van Middendorp JJ, Hosman AJ, Pouw MH, Van de MH . ASIA impairment scale conversion in traumatic SCI: is it related with the ability to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord 2009; 47: 555–560.
Acknowledgements
This study was supported by the ‘Internationale Stiftung für Forschung in Paraplegie’ (IFP). We thank Mrs Alice Tillema (librarian) for her assistance in identifying eligible articles for this review.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pouw, M., van Middendorp, J., van Kampen, A. et al. Diagnostic criteria of traumatic central cord syndrome. Part 1: A systematic review of clinical descriptors and scores. Spinal Cord 48, 652–656 (2010). https://doi.org/10.1038/sc.2009.155
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.155
Keywords
This article is cited by
-
Central cord syndrome definitions, variations and limitations
Spinal Cord (2023)
-
Is it time to redefine or rename the term “Central Cord Syndrome”?
Spinal Cord (2021)
-
Recovery after traumatic thoracic- and lumbar spinal cord injury: the neurological level of injury matters
Spinal Cord (2020)
-
Degenerative cervical myelopathy — update and future directions
Nature Reviews Neurology (2020)
-
The case for revisiting central cord syndrome
Spinal Cord (2020)