Abstract
Study design:
Retrospective cohort study.
Objectives:
To describe the physician utilization patterns (family physicians (FP), specialist and emergency department (ED) visits) of adults with traumatic spinal cord injury (SCI) 1 year after the initial injury.
Setting:
Ontario, Canada.
Methods:
A total of 559 individuals with a traumatic SCI were identified. Five administrative databases were linked to examine health-care utilization in acute care, inpatient rehabilitation, chronic care rehabilitation, outpatient physician visits and ED visits. Factors predicting frequent physician, specialist and ED use were identified.
Results:
The mean number of physician visits for traumatic SCI patients during the first year after their injury onset was 31.7 (median 26). FPs had the greatest number of visits (mean 11.6, median 7) followed by physiatrists (mean 6.1, median 2). Factors predicting 50 or more physician visits included age 70 or above (OR=3.6, 95% CI=2.0–6.5), direct discharge to chronic care (OR=3.6, 95% CI=1.0–13.1) and in-hospital complication (OR=2.34, 95% CI=1.3–4.3). Age 70 or less (OR=0.19, 95% CI=0.0–0.9) and direct discharge to chronic care were associated with 50 or more specialist visits. Only rurality predicted two or more visits to the ED.
Conclusions:
Individuals with traumatic SCI show significant physician utilization, especially among their FPs and physiatrists. Although the factors predicting higher physician and specialist utilization may reflect individuals with the most severe impairment, comorbid conditions or lack of social support, the model for higher ED visits may point to limited accessibility to/availability of primary care services for SCI patients in rural regions.
Similar content being viewed by others
Introduction
A spinal cord injury (SCI) results in a number of motor, sensory and autonomic impairments that predispose a person to multisystem dysfunction, leading to an increased likelihood of a range of related secondary complications.1, 2, 3, 4 In a 6-year follow-up study, Dryden et al.5 demonstrated that among individuals with SCI, 47.6% were treated for a urinary tract infection (UTI), 33.8% for pneumonia, 27.5% for depression and 19.7% for decubitus ulcer (either during initial hospitalization, a subsequent hospitalization or by a physician). A cross-sectional study from the US Model System conducted by Anson and Shepherd6 determined that 95.6% of patients had at least one medical complication at the time of their routine annual checkup and between 28 and 35% of patients (depending on the level of injury) had a UTI and 22.4% had decubitus ulcers. In a population-based survey of persons with SCI in Quebec, researchers found that 56% had experienced a UTI in the previous year, and 28% reported a decubitus ulcer.7 Cardiovascular and psychosocial issues other than depression have also been shown to be prevalent in other studies of post-acute SCI patients.7, 8, 9, 10, 11, 12
Secondary medical complications intensify the experience of disability for people with SCI by negatively impacting on long-term health, productivity/employment, dignity, mobility and independence.13 Health complications following SCI are also costly, in terms of limited health-care resources (direct and indirect costs) and quality of life.14 Dryden et al.5 found that compared with a control group, individuals with SCI required 30 more hours of home-care services, were 2.7 times more likely to have physician contact, were rehospitalized 2.6 times more often and spent 3.3 more days in hospital.
Most of the research on secondary complications in traumatic SCI and subsequent physician utilization has focused on rehospitalization or readmission to acute care. There is a paucity of research in physician utilization by individuals with traumatic SCI, and when it is studied, it is often included in the study of rehospitalization or hospital readmission patterns. There is even less Canadian data in this area. A separate and more detailed examination of physician utilization is necessary to assist health-care providers and policy-makers in the development of effective services and/or programs for person with SCI.5 Therefore, the aim of this study is to describe the physician utilization patterns (that is, family physician (FP), specialist and emergency department (ED) visits) of individuals with traumatic SCI during the first year after their index event. This is the second study in a three-part investigation of SCI incidence, physician utilization and rehospitalization in Ontario, Canada. On the basis of data from the Canadian Institute for Health Information (CIHI), individuals with SCI consist approximately 35% of the Canadian population.15
Methods
Data and population
Data sources
Discharge abstract database: The CIHI hospital Discharge Abstract Database (DAD) captures all acute-care hospital stays in each fiscal year (every record corresponds to one hospital stay). The main data elements are health card number, admission date, patient demographics (gender, date of birth, postal code), most responsible diagnosis (defined as diagnosis most responsible for admission), secondary diagnoses, procedures performed, discharge date, physician and administrative data (institution and hospital number, admission category, length of stay, transfer to another acute-care facility, in-hospital mortality, discharge destination).
Ontario Health Insurance Plan: The Ontario Health Insurance Plan (OHIP) database contains all physicians’ fee-for-service billing or claims.16 The main data elements included in a claim are patient and physician unique identifying number, date of the service/claim, fee code for service provided and fee paid. The DAD and OHIP databases have been validated and shown to be of high quality.17
The National Ambulatory Care Resource System: This database provides information on all visits to EDs in Ontario and was mandated for use in 2001. The main data elements are diagnoses and patient demographics.
National Rehabilitation Reporting System: The National Rehabilitation Reporting System (NRS) was mandated for adult clients (18 years and over) receiving care in designated Ontario rehabilitation beds in October 2002, providing for province-wide inpatient rehabilitation clinical utilization. The main data elements are health card number, admission date, patient demographics and discharge date. The primary outcome measure used in the NRS is the Functional Independence Measure instrument. This is a global assessment measure that was developed for use as part of the Uniform Data System for Medical Rehabilitation in the United States in 1995 on which the NRS is based.
Continuing Care Reporting System: The Continuing Care Reporting System (CCRS) was created as a resource for standardized clinical and administrative information on continuing subacute care in Canada. The database includes detailed clinical, functional and service information that identifies residents’ preferences, needs and strengths, and the services they use. The CCRS captures information on individuals in publicly funded facilities of two types: (1) hospitals that have beds designated and funded as continuing care beds, commonly known across Canada as extended, auxiliary, chronic or complex care beds; and (2) residential care facilities, commonly known across Canada as nursing homes, personal care homes or long-term care facilities.
Study population
The initial population consisted men and women with incident cases of traumatic SCI between the fiscal years of 2003/04 and 2006/07. Cases of ‘spinal cord dysfunction’ were identified using the International Classification of Diseases (ICD-10) codes obtained from the Rick Hansen Foundation (Appendix 1). The following exclusion criteria were then applied to capture the incident cases of traumatic SCI: (1) invalid unique identifiers, (2) age at index admission < 18 years, (3) previous admission for traumatic SCI in the year before the index admission, (4) codes that were not a most responsible diagnosis code of traumatic SCI and (5) transfers that were not to an SCI hospital. Further exclusion criteria were applied to assemble the health-care utilization cohort: (1) in-hospital mortality, (2) index discharge after 31 March 2006 (a minimum of 1 year was needed for follow-up of the 2005/06 cohort) and (3) died within 1 year after the index discharge (a minimum of 1 year was needed for follow-up). It should be noted that index discharge refers to discharge from the acute-care center.
Procedures
Design
This study used a retrospective cohort design during the years 2003/04–2005/06 and examined physician utilization, including FP, specialist and ED visits of adult patients with SCI during the first year after their index event.
Privacy/Ethics
This study was approved by the research ethics board at the Institute for Clinical Evaluative Sciences (ICES) and Sunnybrook Health Sciences Centre in Toronto. The ICES Confidentiality Committee maintains compliance with current Ontario health information legislation and data protection practices.
Measures
Charlson Index
The Charlson Index is the most well-known index of comorbidity. Charlson used statistical methodology to determine and then weigh the 16 illnesses that most predicted 1-year mortality to produce a summative scale that yields a continuous variable from 0 to 31. The scores are typically skewed far right, because most patients have a score of zero. The Charlson Index is widely used in all aspects of outcome research and has been translated to an administrative data format.18
Rurality
The Rurality Index of Ontario (RIO) is made up of 10 components that include measures of population size, travel times to referral centers, population to FP ratios, availability of ambulance and other services, weather conditions, hospital presence and social indicators. The RIO, which can be disaggregated into a geographic and a services component, has been calculated for all Ontario census subdivisions. The RIO is a scaled index between 0 and 100, such that communities with higher values are relatively more rural compared to communities with lower values.19 A cut-point of 45 is considered ‘rural’.
Analysis
Parametric and nonparametric statistics were used to describe the socioeconomic, clinical and physician utilization characteristics of this cohort of patients with traumatic SCI. The analyses were stratified by gender. Multivariate logistic regressions were conducted to examine factors associated with 50 or more physician visits, 50 or more specialist visits and 2 or more visits to the ED. The cut-points of 50 or more and 2 or more, for physician and specialist visits and ED visits, respectively, were used to indicate high utilization. Median values were used in each case to establish the cut-points.
Results
The number of incident traumatic SCI cases over the 5-year study period was 936 (after the exclusion criteria were applied). Further exclusions were used to assemble the physician utilization cohort: 231 for index admission in 2006/07, 86 for discharged dead, 20 for discharged after March 2006 and 40 who died within 1 year after index discharge. These criteria yielded 559 incident cases for the physician utilization cohort.
Significant gender differences were observed across age, cause of injury and discharge disposition (Table 1). Compared to their male counterparts, women had a higher mean age (51.5 versus 45.9 years, P=0.002), and a greater proportion of ‘falls’ listed as their cause of injury (49.3% for women versus 42.1% for men, P=0.006). A greater proportion of men were discharged directly to rehabilitation (60.8% of men versus 49.3% of women, P=0.006).
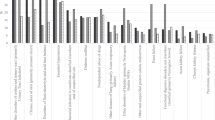
Significant gender differences were observed across all physician, physiatrist and FP visits during the first year after the index event (Table 2). Women with traumatic SCI had a higher mean number of visits to all physicians (37.0 for women versus 30.0 for men, P=0.006) and a higher mean number of visits to their FP (15.4 for women versus 10.3 for men, P<0.001). On the other hand, men had a higher mean number of visits to their physiatrist (4.5 for women versus 6.6 for men, P=0.028).
The associations between sociodemographic and clinical variables and likelihood of physician utilization (50 or more physician visits and 50 or more specialist visits) expressed as odds ratios (ORs) are shown in Tables 3 and 4. Older age (OR=3.64), direct discharge to chronic care (OR=3.62) and an in-hospital complication (OR=2.34) were associated with having 50 or more physician visits. Meanwhile, younger age (OR=0.19) and direct discharge to chronic care (OR=11.52) were associated with 50 or more specialist visits. Only rurality predicted two or more visits to the ED (OR=2.16).
Discussion
The results of this study reveal that individuals with traumatic SCI show significant physician utilization especially among their FPs and physiatrists. Factors related to a high number of physician visits included older age, direct discharge to chronic care and an in-hospital complication. Younger age and direct discharge to chronic care were associated with a high number of specialist visits. Finally, rurality was the only factor predicting the likelihood of frequent ED visits.
Sociodemographic and clinical characteristics
The male/female proportions were consistent with previous research on physician utilization among individuals with traumatic SCI.5 In this study, 75.7% of the cohort was male, consistent with a previous Ontario-based study.5 There were significant gender by age associations, with a higher mean age among women (51.5) rather than men (45.9). This finding may be due to the fact that the most common cause of injury in this cohort was ‘falls’ (women, 49.3%; men, 42.1%), which disproportionately affect older women.20 Previous studies have consistently reported that a motor vehicle collision is the most common cause of traumatic SCI in Canada.5 Therefore, the results of this study may reflect a changing trend in the etiology of traumatic SCI. The finding that falls were the leading cause of injury may also be due to the manner in which the causes of injury were classified in this study or may be related to the ICD-10 codes used in the inclusion criteria. Most studies use motor vehicle collisions, falls, violence and sports, whereas this study used the categories of traffic collisions, nontraffic collision, falls and other, perhaps obscuring the leading cause of injury. This is an important distinction for health-care utilization as those with falls may have higher rates of complications and longer length of stays.
Physician utilization
Patients with traumatic SCI were high health-care users. The mean number of (all) physician visits during the first year after the index event was 31.7; the median number was 26 (interquartile range (IQR), 15–39). FPs had the highest mean number of visits (11.6), followed by physiatrists (6.1). These findings are consistent with those of Dryden et al.,5 as they found that the median number of contacts with all physicians was 22 (IQR, 12–37). Similarly, they found that in the first post-injury year, their SCI group visited FPs, physical medicine specialists and internists most frequently. In the subsequent 5 years, FPs, internists and psychiatrists were seen most often.
This study also alludes to previous research that has shown that persons with SCI experience significantly more health problems than the general population and report a higher prevalence of medical symptoms, greater use of medication, more ED visits and more hospital admissions.21 Future research should involve a more comprehensive list of specialities associated with SCI follow-up care, as well as a more in-depth analysis of the type of services provided by certain specialties (for example, filling of routine prescriptions versus dealing with complications). Finally, it should also be noted that there were significant gender differences in the mean number of FP and physiatrist visits during the first year after the index event, with women having a higher number of visits to their FP (15.4 versus 10.3) and men having a higher number of visits to their physiatrist (6.6 versus 4.5). Future research is needed in this area to tease out the reasons for these differences.
Factors associated with physician utilization
Being discharged directly to chronic care was the strongest predictor for both 50 or more physician visits and 50 or more specialist visits among all the variables examined. This finding, together with the other significant predictors of older age and in-hospital complication (50 or more physician visits) and younger age (50 or more specialist visits) may possibly indicate that high utilization is associated with more severe cases of SCI. Further, this result makes sense as patients are often sent to chronic care if/when their discharge environment is not available/accessible/affordable after rehabilitation, they cannot obtain the necessary attendant care resources in their region, they are unable to direct their care (that is, cognitive deficit), they require significant nursing resources (that is, >4 h per day), they have pressure sores and they have no/limited social supports in their community.
The only significant predictor of two or more ED visits was rurality. A previous study on geographical proximity and health-care utilization in veterans with SCI indicated that outpatient and inpatient services decreased when travel distance to a facility increased.22 The findings of this study may be somewhat related, in that those individuals with SCI in more rural locations have limited access to physicians and/or specialists (with SCI expertise or otherwise), and thus their only option is to receive care in the ED. Therefore, although high physician and specialist utilization may be related to severity, high ED utilization may be related to accessibility. Future research is needed to provide a more detailed picture of the predictors of physician utilization (for example, specific types of complications, functional status).
Limitations
The data were limited to health-care services that were provided in the province of Ontario. Therefore, it is not possible to determine the extent to which patients sought out-of-province care or the nature of services. This would result in an underestimate of service utilization among individuals with traumatic SCI. Further, the data sources do not provide measures of severity such as the American Spinal Injury Association Impairment Scale, neurological outcomes or functional recovery of persons with SCI, which might be associated with utilization of heath services. Despite the above limitations, to the best of our knowledge, this work represents the only population-based study to examine exclusively physician utilization in patients with traumatic SCI. It includes data on all fee-for-service physician contact, ED visits, home-care services and long-term care admissions in a large geographically defined region. Thus, the results of this study can be generalized to areas with similar access to health-care services.
Conclusion
Patients with traumatic SCI are significant users of physician services, especially among their FPs and physiatrists. Although severity, as indicated by discharge to chronic care and in-hospital complication, may be associated with high utilization of physicians and specialists, limited accessibility to primary care may be associated with a high number of ED visits. Future research is needed to provide a more complete picture of physician utilization among patients with SCI and with other rehabilitation professionals so that successful follow-up and treatment courses can be planned. A more detailed understanding of the services provided and provider expertise may assist in the future development of appropriate services for adult patients with traumatic SCI.
References
Paker N, Soy D, Kesikta° N, Nur Bardak A, Erbil M, Ersoy S et al. Reasons for rehospitalization in patients with spinal cord injury: 5 years’ experience. Int J Rehabil Res 2006; 29: 71–76.
Savic G, Short DJ, Weitzenkamp D, Charlifue S, Gardner BP . Hospital readmissions in people with chronic spinal cord injury. Spinal Cord 2000; 38: 371–377.
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W . Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil 2004; 85: 1757–1763.
Berkowitz M . Assessing the socioeconomic impact of improved treatment of head and spinal cord injuries. J Emerg Med 1993; 11 (Suppl 1): 63–67.
Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord 2004; 42: 513–525.
Anson CA, Shepherd C . Incidence of secondary complications in spinal cord injury. Int J Rehabil Res 1996; 19: 55–66.
Noreau L, Proulx P, Gagnon L, Drolet M, Laramée MT . Secondary impairments after spinal cord injury: a population-based study. Am J Phys Med Rehabil 2000; 79: 526–535.
Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG . Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1998; 36: 45–50.
Jackson AB, Groomes TE . Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil 1994; 75: 270–275.
McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ . Long-term medical complications after traumatic spinal cord injury: a regional model system analysis. Arch Phys Med Rehabil 1999; 80: 1402–1410.
Ragnarsson KT, Hall KM, Wilmot CB, Carter RE . Management of pulmonary, cardiovascular, and metabolic conditions after spinal cord injury. In: Stover SL, DeLisa JA, Whiteneck GG (eds). Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen: Gaithersburg, MD, 1995 pp 79–99.
Hitzig SL, Tonack M, Campbell KA, McGillivray CF, Boschen KA, Richards K et al. Secondary health complications in an aging Canadian spinal cord injury sample. Arch Phys Med Rehabil 2008; 87: 545–555.
Post M, Noreau L . Quality of life after spinal cord injury. J Neurol Phys Ther 200; 29: 139–146.
Dorsett P, Geraghty T . Health-related outcomes of people with spinal cord injury—a 10 year longitudinal study. Spinal Cord 2008; 46: 386–391.
Canadian Institute of Health Information. Inpatient Rehabilitation in Canada 2006–2007. CIHI: Ottawa, 2008.
OHIP. Schedule of Benefits. Bulletin on BMD. Ontario MHLTC: Toronto, Canada, 1999.
Ray WA, Griffin MR, West R, Strand L, Melton III LJ . Incidence of hip fracture in Saskatchewan, Canada 1976–1985. Am J Epidemiol 1990; 131: 502–509.
Hall SF, Groome PA, Streiner DL, Rochon PA . Interrater reliability of measurements of comorbid illness should be reported. J Clin Epidemiol 2006; 59: 926–933.
Kralj B . Measuring ‘rurality’ for purposes of health-care planning: an empirical measure for Ontario. Ont Med Rev 2000; Oct: 37–40.
Kannus P, Parkkari J, Koskinen S, Niemi S, Palvanen M, Järvinen M et al. Fall-induced injuries and deaths among older adults. JAMA 1999; 281: 1895–1899.
Levi R, Hultling C, Seiger A . The Stockholm Spinal Cord Injury Study: 2. Associations between clinical patient characteristics and post-acute medical problems. Paraplegia 1995; 33: 585–594.
LaVela SL, Smith B, Weaver FM, Miskevics SA . Geographical proximity and health care utilization in veterans with SCI&D in the USA. Soc Sci Med 2004; 59: 2387–2399.
Acknowledgements
This research was supported by a grant from the Ontario Neurotrauma Foundation (ONF). Dr Jaglal is the Toronto Rehabilitation Institute Chair at the University of Toronto in Health Services Research. Dr Couris’ post-doctoral fellowship was supported by the Toronto Rehabilitation Institute and the University of Toronto.
Author information
Authors and Affiliations
Corresponding author
Appendix 1: Definition of SCI from Discharge Abstract Database:
Appendix 1: Definition of SCI from Discharge Abstract Database:
Traumatic SCI ICD-10 codes (obtained from Rick Hansen Foundation)
S14.0 Concussion and oedema of cervical spinal cord
S14.10 Complete lesion of cervical spinal cord
S14.11 Central cord lesion of cervical spinal cord
S14.12 Anterior cord syndrome of cervical spinal cord
S14.13 Posterior cord syndrome of cervical spinal cord
S14.18 Other injuries of cervical spinal cord
S14.19 Unspecified lesion of cervical spinal cord
S24.0 Concussion and oedema of thoracic spinal cord
S24.10 Complete lesion of thoracic spinal cord
S24.11 Central cord lesion of thoracic spinal cord
S24.12 Anterior cord syndrome of thoracic spinal cord
S24.13 Posterior cord syndrome of thoracic spinal cord
S24.18 Other injuries of thoracic spinal cord
S24.19 Unspecified lesion of thoracic spinal cord
S34.0 Concussion and oedema of lumbar spinal cord
S34.10 Complete lesion of lumbar spinal cord
S34.11 Central cord lesion of lumbar spinal cord
S34.12 Anterior cord syndrome of lumbar spinal cord
S34.13 Posterior cord syndrome of lumbar spinal cord
S34.18 Other injuries of lumbar spinal cord
S34.19 Unspecified lesion of lumbar spinal cord
S34.30 Laceration of cauda equina
S34.38 Other and unspecified injury of cauda equina
T06.0 Injuries of brain and cranial nerves with injuries of nerves and spinal cord at neck level
T06.1 Injuries of nerves and spinal cord involving other multiple body regions.
Rights and permissions
About this article
Cite this article
Munce, S., Guilcher, S., Couris, C. et al. Physician utilization among adults with traumatic spinal cord injury in Ontario: a population-based study. Spinal Cord 47, 470–476 (2009). https://doi.org/10.1038/sc.2008.173
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.173
Keywords
This article is cited by
-
Identifying prescribers of antibiotics in a primary care spinal cord injury cohort
Spinal Cord Series and Cases (2024)
-
Identifying Ontarians with Type 2 Diabetes Mellitus in Administrative Data: A Comparison of Two Case Definitions
Diabetes Therapy (2024)
-
Exploring caregivers’ perceptions of community-based service requirements of patients with spinal cord injury: a qualitative study
BMC Primary Care (2023)
-
Examining the impact of COVID-19 on health care utilization among persons with chronic spinal cord injury/dysfunction: a population study
Spinal Cord (2023)
-
The effect of rurality and distance from care on health outcomes, environmental barriers, and healthcare utilization patterns in persons with traumatic spinal cord injury
Spinal Cord (2023)