Abstract
Study design
Population-based cohort study for the western part of Quebec.
Objectives
To determine the impact of declining to participate in a national spinal cord injury (SCI) registry on patient outcomes and continuum of care.
Setting
Level-1 trauma center specialized in SCI care in Montreal, Canada.
Methods
This cohort study compared the outcomes of 444 patients who were enrolled in the Rick Hansen SCI registry and 140 patients who refused. Logistic regression analyses were performed to assess the association between voluntary participation and the outcomes, while adjusting for confounding factors. The main outcomes were: attendance to follow-up 6- to 12-month post injury, 1-year mortality, and the occurrence of pressure injury during acute care.
Results
Declining to be enrolled in the registry was a significant predictor of lower attendance to specialized follow-up (adjusted odds ratio [OR] 0.04, 95% confidence interval [CI] 0.02–0.08). It was also associated with a higher 1-year mortality rate (OR 12.50, CI 4.50–33.30) and higher occurrence of pressure injury (OR 2.56, CI 1.56–4.17).
Conclusions
This study sheds invaluable insight on individuals that researchers and clinicians are usually blind to in SCI cohort studies. This study suggests that decline to participate in a registry during the care hospitalization may be associated with worsened health, poorer outcomes, and reduced follow-up to specialized care. Declining the enrollment to voluntary registry could represent a potential prognostic factor for future research.
Similar content being viewed by others
Introduction
Traumatic spinal cord injury (tSCI) leads to varying degrees of neurological impairments, functional limitations, and may lead to numerous life-threatening complications in some individuals. There are approximately 27 million individuals living with a SCI worldwide, and close to 1 million new cases per year [1]. The incidence of tSCI in Canada is expected to increase in the future, paralleling the expanding proportion of elderly persons [2]. SCIs are most often due to trauma, with falls and road accidents being the leading causes [1]. Among all trauma population admitted for acute care, the tSCI population represents the most resource intense in terms of costs [3].
Disease-specific patient registries provide a real-world view of clinical practice, outcomes, and comparative effectiveness, while facilitating epidemiological and clinical research [4, 5]. Other purposes of registries include the implementation of best practices and quality improvement. There are several registries worldwide recruiting patients with SCI [6,7,8,9,10,11,12,13,14]. As such, the Rick Hansen Spinal Cord Injury Registry (RHSCIR) collects data from 30 acute trauma and rehabilitation centers across Canada specializing in tSCI care, and currently includes nearly 8000 participants. It consists of a prospective observational study that involves data collection in line with international standards, standardized reports provided to clinicians and administrators, the development of accreditation standards, and a collaborative network for conducting research [7, 15].
However, as enrollment to patient registries is voluntary, the evaluation of the tSCI population drawn from patient registries is only as good as their representativeness. Unfortunately, to our knowledge, representativeness of patient registries in the Canadian SCI population has been poorly studied to date. Yet, this information is crucial to improve our understanding of what might be normally missing from SCI cohort studies, allowing an enhanced interpretation of data from voluntary registries. Accordingly, we hypothesized that individuals who declined to be enrolled in a national SCI registry such as the RHSCIR present different characteristics and patient outcomes in terms of mortality, medical complications, follow-up rate, admission to inpatient specialized rehabilitation, and length of stay as compared to participants. To verify this hypothesis, we proposed a population-based retrospective cohort study of patients admitted for an acute tSCI in the western part of Quebec, who did or did not consent to enroll in the registry during the same time period.
Methods
Study population
This retrospective cohort study was performed on a consecutive cohort of patients admitted for an acute tSCI to a single Level I trauma center specialized in tSCI care in the province of Québec between April 2010 and May 2019. This center was designated in 1997 by the Ministère de la santé et services sociaux du Québec (MSSS) as the single trauma center for tSCI for the western part of Quebec. Included patients were aged 16 years or older and had sustained a tSCI (or cauda equina syndrome) with a neurological level of injury (NLI) between C0 and S2. The study was approved by the institutional review board and was performed according to the ethical standards of the Declaration of Helsinki.
Data collection
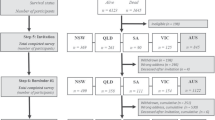
Of the 625 eligible patients, 41 were excluded: 6 lived outside of Québec (follow-up impossible), 24 had absent or incomplete neurological examination, and 11 had missing data. The final cohort consisted of 444 patients enrolled in the RHSCIR after having provided voluntary consent during the acute hospitalization (registry group), and 140 patients who refused to be enrolled in the RHSCIR after being approached by the team (no-registry group).
In our healthcare system, all patients sustaining an acute tSCI are managed in collaborating acute and intensive functional rehabilitation (IFR) centers of expertise, which deliver specialized and coordinated SCI care [16]. In our acute center of expertise, the care team focuses on medical and surgical management, prevention of medical complications, initiation of the multidisciplinary rehabilitation process, and organization of the subsequent rehabilitation plan. Thereafter, the IFR team focuses on maximizing functional recovery and community reintegration. The acute care and the IFR phases take place in two different facilities designated by our provincial government (MSSS) [17]. The eligibility of patients for specialized IFR is determined by the acute rehabilitation team, based on concerted criteria priorly established by the acute and the IFR teams [18]. In our system of care, healthcare resources (including acute and rehabilitation care required for tSCI as well as for all fees related to the care of patients) are covered by our universal healthcare system.
Patients are enrolled during the acute care hospitalization (after medical stability and prior to discharge) and receive a voluntary consent form and a booklet including the history, mission, and objectives of the RHSCIR, as well as contact information of a research team member for further questions. Participating patients consent to the collection and use of data pertaining to their medical condition, as well as the completion of questionnaires at follow-up visits. Follow-up visits in the RHSCIR throughout Canada are planned at 6 months, 1, 2, and 5 years post injury and continues each 5 years thereafter. However, only the 6- and 12-month follow-up assessments are considered in the current study. Data are collected prospectively by team members dedicated to the registry throughout the continuum of care (acute, rehabilitation, and return to community phase). Caregivers remain blind to the patient’s decision to be enrolled in the registry throughout inpatient care (acute and rehabilitation). Data for the no-registry group were retrieved from medical and administrative records from the Quebec’s Government trauma registry (Quebec Injury Registry information system—Système d’information du Registre des traumatismes du Québec (by the MSSS)), collecting data for all trauma patients throughout our province (no voluntary consent required) [17].
Age at injury, sex, Injury Severity Score (ISS) [19] for assessing trauma severity, co-occurrence of traumatic brain injury, and distance between place of residence and trauma center were obtained for all patients. The neurological examination was performed according to the International Standards for Neurological Classification of Spinal Cord Injury. The initial severity of the tSCI was described by the American Spinal Injury Association impairment scale (AIS) grade, and NLI (high cervical: C1–C4, low cervical: C5–C8, thoracic: T1–T8, thoracolumbar and lumbosacral: T9–S2) [20].
Outcomes
Different variables pertaining to patient outcomes and continuum of care were collected. The main outcomes of this study were:
-
Attendance to at least one medical follow-up visit 6–12 months after the tSCI, when surviving more than 6 months after the tSCI. All patients are routinely given outpatient appointments with the medical team at 6 and 12 months after the tSCI.
-
1-year mortality after the tSCI, assessed as a binary variable (survival vs. death).
-
Occurrence of pressure injury during the acute care hospitalization.
Secondary outcomes were also considered: the acute length of stay in trauma hospital (in days), admission to specialized inpatient functional rehabilitation following acute hospitalization, the IFR length of stay (in days) if transferred for inpatient rehabilitation, and the occurrence of pneumonia during the acute care hospitalization.
Statistical analysis
We first compared the baseline characteristics and outcomes using χ2 tests for categorical variables and Student t tests for continuous variables. Normality of distribution was tested using skewness and kurtosis. Non-normal variables were transformed (using square root or log transformation) in order to obtain a normal distribution prior to performing analyses.
We performed logistic regression analyses to determine the effect of declining to be enrolled in the registry on the outcomes (all binary) on the main outcomes. In addition to participation in the registry, co-variables significant at the univariate level (comparisons between registry and no-registry groups) were included in the multivariable analyses. Considering their potential clinical significance, AIS grade and NLI were also included in multivariable analyses. Goodness of fit was assessed with the Hosmer–Lemeshow test and area under the receiver operating characteristic curve for logistic regression. Collinearity diagnostics were performed to verify the absence of multicollinearity with variance inflation factors <2. The level of significance was set at 0.05. The analyses were performed using IBM SPSS version 25.
Results
The no-registry and registry groups were similar in terms of sex, trauma severity, distance from place of residence to trauma center, co-occurrence of traumatic brain injury, AIS grade, and NLI (Table 1). However, patients in the non-registry group were older (58.5 vs. 49.6 years old; p < 10−5). Of all patients surviving more than 6 months, 93.6% of those recruited in the registry attended at least one follow-up visit between 6 and 12 months after the tSCI, compared to 42.1% for those who did not consent to be enrolled in the registry (p < 10−38) (Table 2). The admission rate to specialized inpatient rehabilitation was lower for the no-registry group (53% vs. 69%; p = 0.001). The 1-year mortality rate was also increased for the no-registry group (19.3% vs. 1.4%; p < 10−14) (Table 2). The majority of deaths within the first year following the tSCI occurred during the acute hospitalization (81%) in the no-registry group, compared to 17% in the registry group.
The acute length of stay was significantly longer when not enrolled in the registry (36.9 vs. 27.8 days; p = 0.04), but the rehabilitation length of stay was similar between the two groups. The occurrence of pneumonia (31.4% vs. 21.8%; p = 0.02) and pressure injury (37.9% vs. 17.6%; p < 10−6) was increased in the no-registry group (Table 2).
Results of the logistic regression analyses are shown in Table 3. Declining to be enrolled in the registry was the single significant predictor of improved follow-up with an adjusted odds ratio (OR) = 0.04 and a 95% confidence interval (CI) = 0.02–0.08. The 1-year mortality rate was significantly higher when not enrolled in the registry (adjusted OR = 12.50, 95% CI = 4.50–33.30). Older age was associated with 1-year mortality (adjusted OR = 1.10, 95% CI = 1.06–1.15). However, more severe AIS grade was the most important predictor of increased 1-year mortality, with adjusted OR = 54.87 (95% CI = 11.25–267.64) for AIS grade A, adjusted OR = 66.82 (95% CI = 10.98–406.59) for AIS grade B, and adjusted OR = 7.58 (95% CI = 1.65–34.68) for AIS grade C lesions.
The occurrence of pressure injury was higher in the no-registry group (adjusted OR = 2.56, 95% CI = 1.56–4.17). Age was weakly associated with increased occurrence of pressure injury (adjusted OR = 1.02, 95% CI = 1.00–1.03), but the most important predictor was the AIS grade (adjusted OR = 12.82 with 95% CI = 6.72–24.43 for AIS grade A, adjusted OR = 7.11 with 95% CI = 3.23–15.62 for AIS grade B, and adjusted OR = 3.76 with 95% CI = 1.95–7.26 for AIS grade C). A pressure injury was more likely with high cervical (adjusted OR = 5.02, 95% CI = 2.59–9.71) and thoracic tSCI (adjusted OR = 2.39, 95% CI = 1.06–5.36).
After adjusting for co-variables, enrollment in the registry was no longer associated with pneumonia (adjusted OR = 0.71, 95% CI = 0.45–1.13) or the acute length of stay (adjusted OR = 0.01, 95% CI = −0.06 to 0.09).
Discussion
To our knowledge, this study is the first to examine non-participants to a national SCI registry, providing an important insight on how we may interpret data from voluntary registries. Our findings for non-participants are invaluable because this important subgroup (24% of the studied population) is usually not represented in SCI cohort studies. Results of this study show that declining enrollment to the registry was associated with decreased attendance to follow-up in the subacute to chronic period, higher mortality, and incidence of pressure injuries during acute care. Thus, individuals who declined enrollment may represent a particularly vulnerable group for which tailored approaches (e.g., psychological support, community resources, peer support/mentoring, etc.) could be provided in an effort to improve the outcomes for the entire tSCI population. This finding also raises the question as to whether unblinding the enrollment status of patients to care providers should be considered to promote the engagement of non-participants in a shared decision planning. Furthermore, these individuals may also benefit from greater efforts to receive follow-up care, particularly within the first year following the injury.
Declining to be enrolled in the registry during the acute care phase hospitalization was the only significant predictor of failing to attend follow-up appointment 6–12 months post injury. Major losses to follow-up is a well-recognized issue for this population [21, 22], while adequate follow-up is essential for preventing and treating long-term complications after tSCI. Preventing long-term complications and enhancing psychological adjustments can be a strong motivation for SCI individuals to participate in research [23]. Follow-up rates after tSCI can be enhanced when patients have positive views of their relationship with healthcare providers and feel they are getting something in return for their efforts [22], which might have resulted from the contacts of patients who were enrolled in the registry to the team members (for consent, information, etc.) throughout the acute and rehabilitation phases. The additional time spent with patients for their enrollment in the registry and the perspective of improved outcomes could facilitate the engagement in their care [24].
The rate of follow-up in the registry group was superior to that reported for patients enrolled in the Spinal Cord Injury Model Systems (SCIMS) in the United States (23% loss to 1-year follow-up) [21]. Different reasons could explain the higher follow-up rate in this study. First, the SCIMS only involves rehabilitation centers at which tSCI patients are recruited [25]. On the opposite, the RHSCIR enrolls patients early during the acute care and data collection continues throughout inpatient rehabilitation. The importance of the medical and surgical care provided early after a tSCI may have demonstrated the substantial benefits for continuing to improve patient care through research activities, which may have favored enrollment in the registry. Follow-up could also be enhanced by our multidisciplinary outpatient clinic through which patients have joint appointments with a spine surgeon and a physiatrist.
The early mortality rate was similar to that observed in previous reports [26, 27]. In agreement with the literature, the AIS grade was the most important predictor of early mortality [26, 27]. However, this research highlights that retrieving data from a registry requiring patient consent may underestimate the burden of mortality and morbidity in the tSCI population. Indeed, almost 20% of the no-registry group died within the first year following the tSCI, as opposed to less than 2% of patients in the registry group. While it is unlikely that refusal to be enrolled in the registry is a direct cause of mortality, it is possible that the subset of patients with poor prognosis will not anticipate any actual gain from the enrollment in a registry and therefore decline participation. Accordingly, 16 of the 22 the no-registry group deceased during the acute care had severe (AIS grade A or B) cervical injuries. Since psychological factors are important predictors of mortality at the chronic stage after tSCI [28], refusal to be enrolled in the registry can foreshadow a need for additional psychological support in these patients.
While it is known that more severe AIS grade and higher NLI are associated with increased occurrence of pressure injuries [29,30,31], our study also showed that declining to be enrolled in the registry was independently associated with an increased occurrence of pressure injuries during acute care. Since frequent repositioning and early mobilization are critical measures for preventing pressure injuries [32], it is possible that participating patients are more likely to engage in repositioning and early mobilization programs. This study may thus suggest that the acute care team should give a particular attention to pressure injury prevention in individuals declining to be enrolled in a voluntary registry, which further reinforces the potential benefits of disclosing this information to the medical team.
Length of stay was mainly influenced by the severity of the tSCI. Despite a mean acute length of stay of 9 days longer in the non-registry group, enrollment in the registry was not associated with the acute length of stay after adjusting for confounding factors. Rehabilitation length of stay was also not associated with declining to be enrolled in the registry, although patient engagement is a key factor for successful rehabilitation after tSCI [33, 34]. This finding must be counterbalanced by the fact that patients at our institution must demonstrate sufficient engagement and collaboration during the acute care to be eligible and accepted for specialized inpatient rehabilitation. Patients enrolled in the registry more likely underwent specialized rehabilitative care (as shown in Table 1). This could be explained by the fact that these individuals were identified as candidates for inpatient rehabilitation by the acute care team (blinded to patient’s enrollment status in the registry), notably by demonstrating sufficient engagement in rehabilitative care.
This study also has its limitations. Although we found associations between enrollment status in the registry and outcomes, the mechanisms by which these outcomes relate to participating in the registry remain to be clarified. Hazard ratio for evaluating the impact of declining to be enrolled in a registry on the mortality rate may be used in a future longitudinal study comprising many time points for follow-up. Consenting to be enrolled in the registry may reflect an increased level of patient engagement and collaboration in care, but needs to be investigated further using standardized measures. Candidate predictors were limited by the available data, but the authors recognize that other predictors such as psychosocial or socio-economic factors (e.g., familial structure, cultural beliefs, insurance status, etc.) should be addressed in future studies. We would like to mention that socioeconomic factors were not considered in this study that is unlikely to have influenced results since this study took place in a universal healthcare system (where healthcare resources are covered by the hospital’s budget).
In conclusion, added to the enhanced research capability and quality care improvement, this study brings an important insight of the representativeness of tSCI cohorts and allows capturing a better picture of the Canadian tSCI population. This study suggests that individuals who declined to be enrolled in the RHSCIR may represent a vulnerable group of patients displaying characteristics associated with worsened health outcomes and reduced follow-up to specialized care. This study raises the opportunity for identifying patients more likely to present poorer outcomes after refusing to be enrolled in the registry, to better tailor their management thus improving the health of the entire tSCI population. Declining enrollment to a national voluntary SCI registry in the acute care phase may thus represent an important predictive factor of higher mortality, incidence of pressure injuries, and decreased follow-up. It may also represent an important prognosis factor for future research and requires particular attention from the specialized SCI team.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the regulations defined by the ethics committee of the CIUSS Nord-de-l’Île-de-Montréal but are available from the corresponding author on reasonable request.
References
James SL, Theadom A, Ellenbogen RG, Bannick MS, Montjoy-Venning W, Lucchesi LR, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:56–87.
Ahn H, Lewis R, Santos A, Cheng CL, Noonan VK, Dvorak MF, et al. Forecasting financial resources for future traumatic spinal cord injury care using simulation modeling. J Neurotrauma. 2017;34:2917–23.
Porgo TV, Moore L, Truchon C, Berthelot S, Stelfox HT, Cameron PA, et al. Patient-level resource use for injury admissions in Canada: a multicentre retrospective cohort study. Injury. 2019;50:1192–201.
Gliklich RE, Dreyer NA, Leavy MB, editors. Registries for evaluating patient outcomes: a user’s guide. Rockville (MD): AHRQ Methods for Effective Health Care; 2014.
Nelson EC, Dixon-Woods M, Batalden PB, Homa K, Van Citters AD, Morgan TS, et al. Patient focused registries can improve health, care, and science. BMJ. 2016;354:i3319.
Stover SL, DeVivo MJ, Go BK. History, implementation, and current status of the National Spinal Cord Injury Database. Arch Phys Med Rehabil. 1999;80:1365–71.
Noonan VK, Kwon BK, Soril L, Fehlings MG, Hurlbert RJ, Townson A, et al. The Rick Hansen Spinal Cord Injury Registry (RHSCIR): a national patient-registry. Spinal Cord. 2012;50:22–7.
Azadmanjir Z, Jazayeri SB, Habibi Arejan R, Ghodsi Z, Sharif-Alhoseini M, Kheiri G, et al. The data set development for the National Spinal Cord Injury Registry of Iran (NSCIR-IR): progress toward improving the quality of care. Spinal Cord Ser Cases. 2020;6:17.
Nachtegaal J, van Langeveld SA, Slootman H, Post MWM. Dutch-Flemish Spinal Cord Society Implementation of a standardized dataset for collecting information on patients with spinal cord injury. Top Spinal Cord Inj Rehabil. 2018;24:133–40.
Aschauer-Wallner S, Mattiassich G, Aigner L, Resch H. The Austrian Spinal Cord Injury Study: a registry for patients living with a traumatic spinal cord injury. Spinal Cord Ser Cases. 2017;3:17076.
Tee JW, Chan PC, Rosenfeld JV, Gruen RL. Dedicated spine trauma clinical quality registries: a systematic review. Glob Spine J. 2013;3:265–72.
Charlifue S, Tate D, Biering-Sorensen F, Burns S, Chen Y, Chun S, et al. Harmonization of databases: a step for advancing the knowledge about spinal cord injury. Arch Phys Med Rehabil. 2016;97:1805–18.
Howard-Brown C, Civil I. New Zealand Spinal Cord Registry: a new milestone. N Z Med J. 2016;129:6–7.
O’Connor PJ. Development and utilisation of the Australian spinal cord injury register. Spinal Cord. 2000;38:597–603.
Dvorak MF, Cheng CL, Fallah N, Santos A, Atkins D, Humphreys S, et al. Spinal Cord Injury Clinical Registries: improving care across the SCI care continuum by identifying knowledge gaps. J Neurotrauma. 2017;34:2924–33.
Moutquin JM LK, Mayot MH, Rossignol M. Lésions médullaires traumatiques et non traumatiques: analyse comparative des caractéristiques et de l’organisation des soins et services de réadaptation au Québec. ETMIS. 2013;9:1–44.
Québec MdlSeSSd. Cadre normatif du système d’information du Registre des traumatismes du Québec (SIRTQ) Publications du ministère de la Santé et des Services sociaux du Québec; 2020. Available from: https://publications.msss.gouv.qc.ca/msss/document-001684/?&date=DESC. Accessed 12 Oct 2020.
Network GR. Inpatient Rehab/LTLD Referral Guidelines 2009. Available from: gtarehabnetwork.ca.
Baker SP, O’Neill B, Haddon W Jr., Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
Kirshblum S, Waring W III. Updates for the International Standards for Neurological Classification of Spinal Cord Injury. Phys Med Rehabil Clin N Am. 2014;25:505–17. vii.
Kim H, Cutter GR, George B, Chen Y. Understanding and preventing loss to follow-up: experiences from the Spinal Cord Injury Model Systems. Top Spinal Cord Inj Rehabil. 2018;24:97–109.
Canupp KC, Waites KB, DeVivo MJ, Richards JS. Predicting compliance with annual follow-up evaluations in persons with spinal cord injury. Spinal Cord. 1997;35:314–9.
Heselmans A. Research participation for patients with spinal cord injury. Lancet Neurol. 2020;19:109.
Jerofke-Owen T, Dahlman J. Patients’ perspectives on engaging in their healthcare while hospitalised. J Clin Nurs. 2019;28:340–50.
Chen Y, DeVivo MJ, Richards JS, SanAgustin TB. Spinal Cord Injury Model Systems: review of program and national database From 1970 to 2015. Arch Phys Med Rehabil. 2016;97:1797–804.
Wilson JR, Cadotte DW, Fehlings MG. Clinical predictors of neurological outcome, functional status, and survival after traumatic spinal cord injury: a systematic review. J Neurosurg Spine. 2012;17:11–26.
Shibahashi K, Nishida M, Okura Y, Hamabe Y. Epidemiological state, predictors of early mortality, and predictive models for traumatic spinal cord injury: a multicenter nationwide cohort study. Spine (Philos Pa 1976). 2019;44:479–87.
Krause JS, Cao Y, DiPiro N. Psychological factors and risk of mortality after spinal cord injury. J Spinal Cord Med. 2019;43:667–75.
Gour-Provencal G, Mac-Thiong JM, Feldman DE, Begin J, Richard-Denis A. Decreasing pressure injuries and acute care length of stay in patients with acute traumatic spinal cord injury. J Spinal Cord Med. 2020;11:1–9.
Grigorian A, Sugimoto M, Joe V, Schubl S, Lekawa M, Dolich M, et al. Pressure ulcer in trauma patients: a higher spinal cord injury level leads to higher risk. J Am Coll Clin Wound Spec. 2017;9:24–31.e1.
Brienza D, Krishnan S, Karg P, Sowa G, Allegretti AL. Predictors of pressure ulcer incidence following traumatic spinal cord injury: a secondary analysis of a prospective longitudinal study. Spinal Cord. 2018;56:28–34.
European Pressure Ulcer Advisory Panel NPIAPaPPPIA. Prevention and treatment of pressure ulcers/injuries: clinical practice guideline. The International Guideline: EPUAP/NPIAP/PPPIA. 2019;405.
Lindberg J, Kreuter M, Taft C, Person LO. Patient participation in care and rehabilitation from the perspective of patients with spinal cord injury. Spinal Cord. 2013;51:834–7.
Melin J, Persson LO, Taft C, Kreuter M. Patient participation from the perspective of staff members working in spinal cord injury rehabilitation. Spinal Cord. 2018;56:614–20.
Acknowledgements
The authors thank Jean Bégin, PhD, for his assistance in the statistical analyses, as well as Geneviève LeBlanc, Erika Rinaldi, and Laura Impériale for their assistance in collecting the data.
Funding
The Praxis Spinal Cord Institute supported the data collection for patients enrolled in the Rick Hansen Spinal Cord Injury Registry. This study was supported by the Medtronic Research Chair in Spinal Trauma at Université de Montréal, Fonds de recherche du Québec – Santé, and PREMIER summer student program at Université de Montréal. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
AR-D and J-MM-T are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Concept and design: AR-D, J-MM-T. Acquisition, analysis, or interpretation of data: AR-D, L-FG, AD, ÉB-M, GM, PK, J-MM-T. Drafting of manuscript: AR-D. Critical revision of the manuscript for important intellectual content: AR-D, L-FG, AD, ÉB-M, GM, PK, J-MM-T. Statistical analysis: AR-D, J-MM-T. Obtained funding: AR-D, J-MM-T. Supervision: AR-D, J-MM-T.
Corresponding author
Ethics declarations
Conflict of interest
AR-D has received a scholarship and research grants from the Fonds de recherche du Québec – Santé, an investigator-initiated research grant from Medline Industries, as well as research grants from Praxis Spinal Cord Institute, Craig H. Neilsen Foundation, Social Sciences and Humanities Research Council, Canadian Institutes of Health Research, and Natural Sciences and Engineering Research Council. L-FG has received a scholarship from the Medtronic Research Chair in Spinal Trauma at Université de Montréal. AD has received a scholarship from the PREMIER summer student program at Universtié de Montréal. ÉB-M has received educational grants from Medtronic and Depuy-Synthes. GM has received educational grants from Medtronic and Depuy-Synthes. PK has received educational grants from Medtronic and Depuy-Synthes. J-MM-T is chairholder of Medtronic research chair in spinal trauma at Université de Montréal, owns stocks and is a board member in Spinologics, and has received a scholarship and research grants from the Fonds de recherche du Québec – Santé, an investigator-initiated research grant from Medline Industries, educational grants from Medtronic and Depuy-Synthes, as well as research grants from the US Department of Defense – Congressionally directed medical research programs, Craig H. Neilsen Foundation, from Social Sciences and Humanities Research Council, Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council, Canada foundation for innovation, Praxis Spinal Cord Institute, Fondation de recherche et d’Éducation en Orthopédie de Montréal, and Vertex Pharmaceutical.
Ethical approval
This study was approved by the “Comité d’éthique de la recherche du CIUSSS du Nord-de-l’Île-de-Montréal” at Hôpital Sacré-Cœur de Montréal. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Richard-Denis, A., Gravel, LF., Dionne, A. et al. An evaluation of the representativeness of a national spinal cord injury registry: a population-based cohort study. Spinal Cord 59, 1072–1078 (2021). https://doi.org/10.1038/s41393-021-00622-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00622-8