Abstract
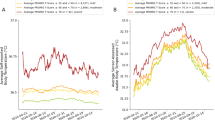
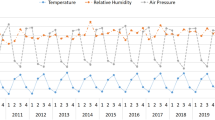
Ambient temperature and the COVID-19 pandemic have both been increasingly associated with mental health issues in many regions of the world, but little is known about the potential role of this pandemic in modifying the association between increased temperature and effects on mental health disorders. We analyzed and compared the associations of mental health disorders (schizophrenia, depression, anxiety, and bipolar disorder) with short-term temperature changes (daily mean temperature and diurnal temperature range) before and during the COVID-19 pandemic in an eastern Chinese city (Hefei). Mean temperature rise (per 1 °C increase) and high diurnal temperature range (99th percentile compared with risk-surge point of diurnal temperature range) were associated with increased risk of emergency department visits for schizophrenia and depression. The effect of mean temperature and diurnal temperature range on depression-related visits was significantly greater during the pandemic than before, whereas there were no significant differences in the effects of temperature changes on emergency department visits for other mental health disorders between the pre-pandemic and pandemic periods. This study provides additional evidence that the COVID-19 pandemic may have modified the effects of short-term temperature changes on mental health disorders, especially depression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Daily emergency department visits for mental health disorders are not authorized to be shared. Hourly meteorological data can be obtained at https://doi.org/10.24381/cds.e2161bac. Daily temperature data from the monitoring station can be obtained at https://www.ncdc.noaa.gov. Hourly air pollutant data can be obtained by submitting the data request to China National Environmental Monitoring Centre (http://www.cnemc.cn/). Estimated annual population data are available from https://doi.org/10.5258/SOTON/WP00647.
Code availability
Codes for data analysis are given in Supplementary Methods 1.
References
Hoegh-Guldberg, O. et al. The human imperative of stabilizing global climate change at 1.5 °C. Science 365, eaaw6974 (2019).
Kalnay, E. & Cai, M. Impact of urbanization and land-use change on climate. Nature 423, 528–531 (2003).
Faurie, C. et al. Association between high temperature and heatwaves with heat-related illnesses: a systematic review and meta-analysis. Sci. Total Environ. 852, 158332 (2022).
Phosri, A., Sihabut, T. & Jaikanlaya, C. Short-term effects of diurnal temperature range on hospital admission in Bangkok, Thailand. Sci. Total Environ. 717, 137202 (2020).
Pan, R. et al. Impacts of heat and cold on hospitalizations for schizophrenia in Hefei, China: an assessment of disease burden. Sci. Total Environ. 694, 133582 (2019).
Qiu, X. et al. Associations of short-term exposure to air pollution and increased ambient temperature with psychiatric hospital admissions in older adults in the USA: a case-crossover study. Lancet Planet. Health 6, e331–e341 (2022).
Sung, T. I. et al. Relationship between mean daily ambient temperature range and hospital admissions for schizophrenia: results from a national cohort of psychiatric inpatients. Sci. Total Environ. 410–411, 41–46 (2011).
Zhao, D. et al. Impact of short-term temperature variability on emergency hospital admissions for schizophrenia stratified by season of birth. Int. J. Biometeorol. 61, 589–599 (2017).
Nori-Sarma, A. et al. Association between ambient heat and risk of emergency department visits for mental health among US adults, 2010 to 2019. JAMA Psychiatry 79, 341–349 (2022).
Lee, S. et al. Mental disease-related emergency admissions attributable to hot temperatures. Sci. Total Environ. 616-617, 688–694 (2018).
Sung, T. I., Chen, M. J. & Su, H. J. A positive relationship between ambient temperature and bipolar disorder identified using a national cohort of psychiatric inpatients. Soc. Psychiatry Psychiatr. Epidemiol. 48, 295–302 (2013).
COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398, 1700–1712 (2021).
Baranova, A., Cao, H. & Zhang, F. Severe COVID-19 increases the risk of schizophrenia. Psychiatry Res. 317, 114809 (2022).
Lin, Y. K. et al. Mortality and morbidity associated with ambient temperatures in Taiwan. Sci. Total Environ. 651, 210–217 (2019).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386, 369–375 (2015).
Warburton, D. E., Nicol, C. W. & Bredin, S. S. Health benefits of physical activity: the evidence. CMAJ 174, 801–809 (2006).
Martin-Latry, K. et al. Psychotropic drugs use and risk of heat-related hospitalisation. Eur. Psychiatry 22, 335–338 (2007).
Yuan, J. et al. Relationship between temperature, dopaminergic neurotoxicity, and plasma drug concentrations in methamphetamine-treated squirrel monkeys. J. Pharmacol. Exp. Ther. 316, 1210–1218 (2006).
Keller, M. C. et al. A warm heart and a clear head. The contingent effects of weather on mood and cognition. Psychol. Sci. 16, 724–731 (2005).
Tian, X., Fang, Z. & Liu, W. Decreased humidity improves cognitive performance at extreme high indoor temperature. Indoor Air 31, 608–627 (2021).
Xue, T. et al. Declines in mental health associated with air pollution and temperature variability in China. Nat. Commun. 10, 2165 (2019).
Grahek, I. et al. Motivation and cognitive control in depression. Neurosci. Biobehav. Rev. 102, 371–381 (2019).
Obradovich, N. et al. Nighttime temperature and human sleep loss in a changing climate. Sci. Adv. 3, e1601555 (2017).
Yu, W. et al. Temperature–mortality association during and before the COVID-19 pandemic in Italy: a nationwide time-stratified case-crossover study. Urban Clim. 39, 100948 (2021).
Seposo, X. et al. COVID-19 pandemic modifies temperature and heat-related illness ambulance transport association in Japan: a nationwide observational study. Environ. Health 20, 122 (2021).
Thompson Coon, J. et al. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ. Sci. Technol. 45, 1761–1772 (2011).
Ridley, M. et al. Poverty, depression, and anxiety: causal evidence and mechanisms. Science 370, eaay0214 (2020).
Nicola, M. et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 78, 185–193 (2020).
Mao, Y. et al. The impact of COVID-19 on the employment status and psychological expectations of college graduates: empirical evidence from the survey data of Chinese recruitment websites. Front. Psychol. 13, 1039945 (2022).
Asimakopoulos, L. O. et al. Investigating the association between temperature and hospital admissions for major psychiatric diseases: a study in Greece. J. Psychiatric Res. 144, 278–284 (2021).
Kaciuba-Uscilko, H. & Grucza, R. Gender differences in thermoregulation. Curr. Opin. Clin. Nutr. Metab. Care 4, 533–536 (2001).
Hossain, M. M. et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 9, 636 (2020).
Muñoz Sabater, J., ERA5-Land hourly data from 1950 to present., Copernicus Climate Change Service (C3S) Climate Data Store (CDS), https://doi.org/10.24381/cds.e2161bac (2019).
Tan, H. M. J. et al. The impact of COVID-19 pandemic on the health-seeking behaviour of an Asian population with acute respiratory infections in a densely populated community. BMC Public Health 21, 1196 (2021).
Yi, W. et al. Quantifying the impacts of temperature variability on hospitalizations for schizophrenia: a time series analysis in Hefei, China. Sci. Total Environ. 696, 133927 (2019).
International Statistical Classification of Diseases and Related Health Problems 10th Revision, WHO, https://icd.who.int/browse10/2019/en (2019).
Li, H. et al. Interactive effects of cold spell and air pollution on outpatient visits for anxiety in three subtropical Chinese cities. Sci. Total Environ. 817, 152789 (2022).
Chu, L. et al. Associations between short-term temperature exposure and kidney-related conditions in New York State: the influence of temperature metrics across four dimensions. Environ. Int. 173, 107783 (2023).
Janes, H., Sheppard, L. & Lumley, T. Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology 16, 717–726 (2005).
Maclure, M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am. J. Epidemiol. 133, 144–153 (1991).
Pan, R. et al. Temporal trends of the association between temperature variation and hospitalizations for schizophrenia in Hefei, China from 2005 to 2019: a time-varying distribution lag nonlinear model. Environ. Sci. Pollut. Res. Int. 29, 5184–5193 (2022).
Jahan, S. & Wraith, D. Immediate and delayed effects of climatic factors on hospital admissions for schizophrenia in Queensland Australia: a time series analysis. Environ. Res. 197, 111003 (2021).
Bundo, M. et al. Ambient temperature and mental health hospitalizations in Bern, Switzerland: a 45-year time-series study. PLoS ONE 16, e0258302 (2021).
Peng, Z. et al. Effects of ambient temperature on daily hospital admissions for mental disorders in Shanghai, China: a time-series analysis. Sci. Total Environ. 590–591, 281–286 (2017).
Coronavirus Disease (COVID-19) Weekly Epidemiological Updates and Monthly Operational Updates (WHO, accessed 21 January 2020); https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
Tao, J. et al. Impacts of PM2.5 before and after COVID-19 outbreak on emergency mental disorders: a population-based quasi-experimental and case-crossover study. Environ. Pollut. 334, 122175 (2023).
Song, J. et al. Acute effects of ambient particulate matter pollution on hospital admissions for mental and behavioral disorders: a time-series study in Shijiazhuang, China. Sci. Total Environ. 636, 205–211 (2018).
Altman, D. G. & Bland, J. M. Interaction revisited: the difference between two estimates. Brit. Med. J. 326, 219 (2003).
WorldPop (www.worldpop.org - School of Geography and Environmental Science, University of Southampton; Department of Geography and Geosciences, University of Louisville; Departement de Geographie, Universite de Namur) and Center for International Earth Science Information Network (CIESIN), Columbia University., Global High Resolution Population Denominators Project - Funded by The Bill and Melinda Gates Foundation (OPP1134076)., https://doi.org/10.5258/SOTON/WP00647 (2018).
Burkart, K. G. et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. Lancet 398, 685–697 (2021).
Acknowledgments
This research is funded by the National Natural Science Foundation of China (grant number: 42105165 to J.C.), the High-level Scientific Research Foundation of Anhui Medical University (grant number: 0305044201 to J.C.), and the Discipline Construction of Anhui Medical University (grant number: 0301001836 to J.C.).
Author information
Authors and Affiliations
Contributions
J.C. conceived and designed the study. J.Y., M.Y., Q.X., and C.Z. collected and organized data. K.W. and Q.W. performed the analysis. K.W., H.Z., X.W., J.T., and M.Z.H. contributed to the interpretation of the findings. K.W. wrote the first draft of the manuscript. J.C., N.W., and H.S. edited the manuscript. K.W., M.Y., and Q.W. contributed to visualization. J.C. has verified the data and taken responsibility for the decision to submit the manuscript. All authors read and approved the final version of the manuscript and ensure it is the case.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Francesco Sera and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–3, Tables 1–6, and Methods 1.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, K., Yan, J., Yang, M. et al. Ambient temperature and emergency department visits for mental disorder before and during the COVID-19 pandemic. Nat. Mental Health 2, 278–286 (2024). https://doi.org/10.1038/s44220-023-00193-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00193-y