Abstract
Experiences of discrimination are associated with adverse health outcomes, including obesity. However, the mechanisms by which discrimination leads to obesity remain unclear. Utilizing multi-omics analyses of neuroimaging and fecal metabolites, we investigated the impact of discrimination exposure on brain reactivity to food images and associated dysregulations in the brain–gut–microbiome system. We show that discrimination is associated with increased food-cue reactivity in frontal-striatal regions involved in reward, motivation and executive control; altered glutamate-pathway metabolites involved in oxidative stress and inflammation as well as preference for unhealthy foods. Associations between discrimination-related brain and gut signatures were skewed towards unhealthy sweet foods after adjusting for age, diet, body mass index, race and socioeconomic status. Discrimination, as a stressor, may contribute to enhanced food-cue reactivity and brain–gut–microbiome disruptions that can promote unhealthy eating behaviors, leading to increased risk for obesity. Treatments that normalize these alterations may benefit individuals who experience discrimination-related stress.
Similar content being viewed by others
Main
Racial disparities in obesity persist in America, with minority subgroups experiencing disproportionally higher rates of obesity and obesity-related morbidities1,2,3,4,5. Multiple factors could contribute to such disparities, with the existing literature primarily focused on the role of genetics, diet, physical activity and psychological factors6. Despite its relevance to the etiology of obesity, few studies have directly examined the role of discrimination experiences in the pathways that may increase obesity risk.
Discrimination, a type of psychosocial stressor7,8, is an environmental risk factor for various adverse health outcomes9,10,11,12,13,14,15. Experiences of discrimination can stimulate ingestive behavior by increasing appetite, cravings and motivation to consume highly palatable foods, contributing to stress-related weight gain in obesity16. Neuroimaging studies indicate that stress can alter food-cue reactivity to highly palatable foods17,18. Accordingly, experiences of discrimination may lead to an increased obesity risk via altered food-cue reactivity to hypercaloric and hyperpalatable foods, which are ubiquitous in the Western diet19.
One potential mechanism linking discrimination and obesity involves alterations in the brain–gut–microbiome (BGM) system. Individuals who experience discrimination present heightened stress responses20,21,22. Stress in turn influences the bidirectional communication between the brain and gut via pathways involving the vagus nerve, immune-inflammatory mechanisms, altered microbial metabolites, neurotransmitters and the hypothalamic–pituitary–adrenal axis23,24,25,26,27.
Brain pathways associated with discrimination-related stress responses include reward and cognitive control networks7,8,28,29,30,31,32,33. A recent study indicated that exposure to discrimination was associated with brain functional connectivity alterations in the central executive network33. Overlap in neurobiological pathways linked to stress and energy homeostasis may underlie the co-occurrence of dysregulated feeding behaviors and stress responses, both of which can contribute to obesity16,34. Chronic stress alters responses in prefrontal regions associated with executive control and emotion/impulse regulation as well as in limbic regions involved in reward processing and appetitive responses, providing a neural basis for the impact of chronic stress in modulating food-reward processing and cravings19,35,36,37. In response to food cues, stress could result in the deactivation of frontal executive modulation and potentiate brain activity in limbic regions, eliciting a bias towards unhealthy energy-dense foods17,18.
Discrimination can also alter the gut microbiome33. Stress facilitates gut dysbiosis and increases gut-barrier permeability, producing an inflammatory response and a leaky gut38. Stress-induced unhealthy dietary patterns could result in gut dysbiosis and prompt dysregulated eating behaviors catering to the needs of dominant bacterial species39. Dysregulation of glutamate metabolism plays an important role in inflammatory processes of the central nervous system (CNS) that are associated with stress-related disorders (for example, depression and anxiety) and obesity40,41,42,43. A recent study revealed that stress in early life was associated with altered gut metabolites within the glutamate pathway, potentially via glutamatergic excitotoxicity and oxidative stress mechanisms44,45,46. These stress-related gut metabolites were also associated with alterations in the brain functional connectivity involved in cognitive and emotional processes. Glutamate is also involved in executive control and reward processing, two functions that are highly relevant to the processing of food cues47,48. Together, these studies highlight the role of altered glutamate metabolites in the stress response and their relevance in brain and gut communication.
In this study we investigated the impact of discrimination exposure on neural reactivity to unhealthy and healthy food cues, relevant gut metabolites as well as brain–gut associations to elucidate potential mechanisms linking discrimination and obesity. We hypothesized that increased stress due to higher levels of discrimination exposure, would be associated with: (1) altered brain reactivity towards highly palatable unhealthy foods in brain regions that are associated with reward processing and executive control and (2) altered levels of glutamate metabolites that are implicated in inflammation and oxidative stress. In addition, given that discrimination may modulate the crosstalk between the brain and gut microbiome system49, we predicted that important interactions between discrimination-related neural reactivity to unhealthy sweet-tasting (sugar-rich) foods due to their unique rewarding and analgesic nature50,51,52,53 and metabolites from the glutamate pathway would be observed (Fig. 1).
Discrimination exposure is associated with increased food-cue reactivity—especially towards unhealthy sweet foods—in the frontal-striatal regions involved in reward processing, motivation and executive control, as well as altered gut metabolites in the glutamate pathway associated with oxidative stress and inflammation.
Results
Participant characteristics
There were no significant differences in sex, age, body mass index (BMI), education, marital status, income or diet between the two discrimination exposure groups but socioeconomic status (SES) was significantly lower in individuals with high discrimination exposure (Table 1). Discrimination and diet did not have interaction effects on BMI.
Discrimination-related whole-brain analysis
When using magnetic resonance imaging (MRI) to compare responses to unhealthy sweet foods and nonfoods, the group of individuals exposed to discrimination (high discrimination group) had greater food-cue reactivity towards unhealthy sweet foods than the low discrimination group in the insula, inferior frontal gyrus, lateral orbitofrontal cortex and frontal operculum cortex (Fig. 2a).
a–c, Schematics (top) and MRI images (bottom) of the brains of individuals to compare the food-cue reactivities of unhealthy sweet (a), unhealthy savory (b) and healthy (c) food with nonfood. Regions where greater reactivity was observed in the high discrimination group (n = 50) relative to the low discrimination group (n = 57) are highlighted (colored region); the color bar represents the Z score, with warmer colors indicating higher scores. Comparisons controlled for BMI, sex, age, race, diet and SES. All statistical maps were family-wise error cluster-corrected for multiple comparisons. Cluster level correction: Z > 2.3, P < 0.05. Clusters are listed in Table 2. The numbers located at the top left of each MRI image represent the slices. L, left hemisphere; R, right hemisphere.
In the comparison of unhealthy savory foods versus nonfoods, the high discrimination group had greater food-cue reactivity towards unhealthy savory food than the low discrimination group in the caudate, putamen, insula, frontal pole and lateral orbitofrontal cortex (Fig. 2b).
When healthy foods were compared with nonfoods, the high discrimination group had greater food-cue reactivity towards healthy food cues than the low discrimination group in the superior frontal gyrus and middle frontal gyrus (Fig. 2c).
The low discrimination group did not differ significantly from the high discrimination group on the aforementioned contrasts (Table 2).
When unhealthy sweet foods were compared with healthy sweet foods, the high discrimination group had lower food-cue reactivity towards unhealthy sweet foods than the low discrimination group in the ventromedial prefrontal cortex (vmPFC). No significant discrimination-related differences were found in the comparison of unhealthy savory foods versus healthy savory foods.
Discrimination-related food-cue brain analysis
The Everyday Discrimination Scale (EDS) score correlated positively with greater reactivity to unhealthy sweet food (β = 0.29, q = 0.03), unhealthy savory food (β = 0.32, q = 0.03) and healthy food (β = 0.72, q < 0.001) in the discrimination-related composite food-cue region of interest (ROI).
Discrimination-related gut-metabolite analysis
Two metabolites from the glutamate pathway, N-acetylglutamate (P = 0.04) and N-acetylglutamine (P = 0.002), were present at significantly higher levels in the high discrimination group than in the low discrimination group (Table 3 and Fig. 3a). N-acetylglutamine levels remained significantly different between the two groups after multiple correction (q = 0.025). Neither N-acetylglutamate nor N-acetylglutamine were significantly correlated with SES.
a, N-acetylglutamate and N-acetylglutamine levels in high and low discrimination groups. Glutamate-pathway metabolites were compared between high and low discrimination groups using generalized linear modeling, controlling for BMI, sex, age, race, diet and SES. High discrimination, n = 30; low discrimination, n = 32. b, Willingness to eat ratings for unhealthy and healthy foods. Comparisons between the high and low discrimination groups were made using generalized linear modeling, controlling for BMI, sex, age, race, diet and SES. High discrimination, n = 50; low discrimination, n = 57. a,b, The violin plots represent the data distribution. Boxplots: the boxes indicate the 75th (upper horizontal line), median (middle horizontal line) and 25th (lower horizontal line) percentiles of the distribution; the whiskers indicate the range of data falling within a distance of 1.5× the interquartile range. P < 0.05 was considered significant (the Q value is the adjusted P value after FDR correction for multiple comparisons).
Willingness to eat unhealthy and healthy foods
The high discrimination group had significantly higher ratings of willingness to eat unhealthy foods (P = 0.048) relative to the low discrimination group but this difference did not exist for healthy foods (P = 0.174; Fig. 3b).
Structural equation modeling linking discrimination, brain and gut metabolites
In the unhealthy sweet food model (Fig. 4a), positive associations were observed between high discrimination exposure and brain reactivity (standardized coefficient = 0.31, P = 0.009) as well as between discrimination and glutamate metabolism (that is, N-acetylglutamate and N-acetylglutamine levels; standardized coefficient = 0.42, P = 0.004). The bidirectional association between the brain and gut was significant (standardized coefficient = 0.34, P = 0.048). In terms of the structural equation model (SEM) fit, the root mean square error of approximation (RMSEA) was 0.0, comparative fit index (CFI) was 1.0, goodness-of-fit index (GFI) was 0.955 and standardized root mean square residual (SRMR) was 0.071; all indices suggested a good fit.
a–c, SEM diagrams showing the relationships between brain, gut and discrimination (controlling for BMI, race, diet, and SES) for unhealthy sweet foods (a), unhealthy savory foods (b) and healthy foods (c). Single-headed arrows represent regression and double-headed arrows represent correlation. The values on arrows between latent and observed variables and between latent and observed indicators represent standardized path coefficients and factor loadings (that is, standardized coefficients), respectively. For the arrows between brain, gut and discrimination, black arrows indicate significant correlation or regression coefficients and gray arrows indicate non-significant correlation or regression coefficients. Model fit was assessed using the following indices and criteria: CFI > 0.9, RMSEA < 0.08, GFI > 0.9 and SRMR < 0.08. High discrimination, n = 50; low discrimination, n = 57. *P < 0.05; **P < 0.01; ***P < 0.001.
For the unhealthy savory food model (Fig. 4b), discrimination correlated positively with brain reactivity (standardized coefficient = 0.249, P = 0.043) as well as between discrimination and glutamate metabolism (standardized coefficient = 0.462, P = 0.006). No significant correlations between the brain and gut were observed (standardized coefficient = −0.227, P = 0.216). The RMSEA was 0.0, CFI was 1.0, GFI was 0.964 and SRMR was 0.058, suggesting a good model fit.
In the healthy food model (Fig. 4c), positive associations were observed between high discrimination exposure and brain reactivity (standardized coefficient = 0.454, P < 0.001) as well as between discrimination and glutamate metabolism (standardized coefficient = 0.445, P = 0.004). However, the bidirectional association between the brain and gut was not significant (standardized coefficient = 0.155, P = 0.373). The RMSEA was 0.0, CFI was 1.0, GFI was 0.969 and SRMR was 0.058; thus, all indices suggested a good model fit.
Discussion
We investigated associations between self-reported discrimination exposure and alterations in the BGM system. Discrimination exposure was associated with increased food-cue reactivity in frontal-striatal regions involved in reward processing, motivation and executive control, especially towards unhealthy foods. The alterations in the brain were consistent with observed unhealthy food preference—as indicated by an increased willingness to eat—in individuals who reported higher levels of exposure to discrimination. Discrimination exposure was also associated with altered gut metabolites from the glutamate pathway involved in oxidative stress and inflammation. Complex relationships between discrimination exposure and bidirectional brain–gut alterations were observed, especially when evaluating brain reactivity to unhealthy sweet foods (but not unhealthy savory or healthy foods).
Discrimination-associated brain food-cue reactivity
Unhealthy food cues elicited greater activation in regions associated with reward processing and appetitive responses (insular cortex, orbitofrontal cortex, inferior frontal gyrus, striatum (caudate and putamen) and frontal operculum) in individuals reporting more discrimination experiences than in those with fewer experiences. These frontal-striatal regions have been linked to food-cue reactivity and play a key role in controlling feeding behavior in response to reward and hedonic aspects of food54,55,56. In contrast, healthy food cues were associated with brain reactivity in the frontal pole, middle frontal gyrus and superior frontal gyrus, which partially overlap with the dorsolateral prefrontal cortex (dlPFC). These regions have been implicated in cravings and executive control. These results suggest that stress may lead to exaggerated brain responses associated with reward processing and motivation as well as compromised frontal processes associated with self-regulation in response to unhealthy foods18,57,58,59.
Individuals with greater exposure to discrimination also had altered brain responses in the superior frontal gyrus, which partially belongs to the dlPFC, a brain region associated with executive control, reward appraisal and food-cue-induced craving modulation60,61,62. A recent study revealed a link between racial discrimination and maladaptive eating behaviors (for example, overeating and loss-of-control eating) in young Black women, potentially as a way to cope with stress63. Studies have also shown that those with higher levels of food addiction (that is, addiction-like loss-of-control eating behaviors) exhibited altered food-cue reactivity to unhealthy foods in the superior frontal gyrus64. The dlPFC has been implicated in food-choice-related self-control over appetitive food cravings65,66 and is associated with more effortful exertion of self-control in response to food-cue-induced cravings in obesity67. The enhanced frontal alterations in the high discrimination group might indicate an ineffective (for example, more effortful) regulation of cue-induced cravings, suggesting compromised executive control, particularly for unhealthy foods and even healthy foods with moderate reward value.
The analyses using the composite mask also demonstrated heightened brain food-cue responses in frontal-striatal networks with greater discrimination exposure, suggesting heightened reward processing and compromised executive control in response to unhealthy foods.
Discrimination-related gut-metabolite alterations
Greater discrimination exposure was associated with higher levels of N-acetylglutamate and N-acetylglutamine, which are linked to glutamate metabolism. This pathway has been implicated in inflammatory processes and oxidative stress, as well as obesity pathophysiology. Similarly, discrimination is associated with increased systemic inflammation and decreased levels of gut metabolites with anti-inflammatory and cardioprotective properties but only when the sample is stratified according to race/ethnicity33. The untargeted analyses conducted in this previous study did not reveal significant changes in the metabolome related to discrimination33, which could be attributed to not accounting for key confounding variables. The specific role of N-acetylglutamate and N-acetylglutamine is still an active area of research but their direct connection to glutamate metabolism suggests potential implications for glutamate levels. N-acetylglutamate is both a host- and microbial-derived metabolite, and is altered in patients with chronic obstructive pulmonary disease and progressive inflammatory lung disease68. Glutamate metabolism is also implicated in obesity-associated mechanisms. The abundance of gut glutamate-fermenting microbiota (Bacteroides thetaiotaomicron) is decreased in individuals with obesity and inversely correlated with serum glutamate levels; weight loss through bariatric surgery can partially reverse such alterations69.
The existing literature demonstrates the key role of microbiota-derived metabolites and their derivatives in gut–brain communication70. Gastrointestinal metabolite signatures have demonstrated that alterations in the gut microbiota are closely correlated with alterations in gut and brain glutamate levels71,72, suggesting gut-modulated CNS glutamatergic neurotransmission. N-acetylglutamate may play a role in regulating N-acetyl-l-aspartyl-l-glutamate and brain function73. N-acetyl-l-aspartyl-l-glutamate, a dipeptide that is most abundant in the brain, acts as a neuromodulator at glutamatergic synapses, inhibiting excessive glutamate signaling74. N-acetylglutamate has also been implicated in the brain sleep–wake cycle75. Although the exact role of N-acetylglutamate and N-acetylglutamine is still under investigation, their direct relationship to glutamate metabolism suggests a potential impact on brain function.
Glutamate, the major excitatory neurotransmitter in the CNS, is a non-essential amino acid associated with numerous stress responses76. Inflammation influences the release, transmission and metabolism of glutamate, leading to accumulated extracellular glutamate in the CNS77. Prolonged presence of glutamate can induce excitotoxicity and oxidative stress, two of the major mechanisms responsible for neuronal damage78. Glutamate may also be involved in the biological mechanisms underlying depression, anxiety-related disorders and obesity risk42,79,80. Early life stress is associated with dysregulation of gut glutamate metabolites, potentially through glutamatergic excitotoxicity and increased oxidative stress44. Circulating glutamate is also associated with excess abdominal adipose tissue in obesity, which is potentially related to expression of the GLUL gene (encoding glutamate-ammonia ligase) and inflammatory genes in adipose tissue81,82.
We see evidence for a strong association between gut levels of glutamate metabolites with greater discrimination exposure—this relationship may certainly contribute to potentially excitotoxic sequelae of glutamate and its derivatives as well as a proinflammatory state in obesity.
Discrimination and communication in the BGM system
The results presented here suggest that unhealthy sweet foods may play a major role in the bidirectional communication between the brain and gut with higher discrimination exposure. The mechanisms underlying this association may involve inflammatory processes in the BGM system involved in stress-induced unhealthy eating behaviors and dysfunctional glutamatergic signaling. Stress could promote unhealthy food choices83, particularly for sweet foods84,85, which could adversely influence the systemic homeostasis within the BGM system, resulting in inflammation in the CNS and an increased risk of obesity and stress-related neuropsychiatric complications86,87,88,89. Sugar, delivered intestinally, can activate gut-to-brain pathways by activating vagal neurons in mice, underlying the highly appetitive effects of sugar53. Interestingly, racial and ethnic differences in sweet preference have also been observed90. Greater desire for sweet taste is associated with higher levels of stress to a greater extent among young Black adults than among similarly aged White adults91,92. Accordingly, discrimination, as a stressor, could promote more consumption of sweet food relative to that for highly savory food93,94.
Sweet-tasting foods present an analgesic effect; individuals consume more sweet foods after acute physical pain50. Furthermore, the consumption of sweet-tasting food increases pain tolerance via the endogenous opioid system in the brain51. Extensive research has highlighted variations in the opioidergic system in the context of racial discrimination stress and its effect on pain perception95,96. Stress can upregulate the amygdala κ-opioid receptor, inducing dysphoria, and modulate the μ-opioid receptor to regulate reward processes97,98. When stress activates the opioidergic system, it could affect the rewarding properties of food and potentially lead to stress-related changes in food choices, eating behaviors and obesity. Hence, future studies should further examine the role of the opioidergic system in the context of the effects of discrimination on brain–gut communication, specifically focusing on its influence on unhealthy food preferences, particularly sugary foods. In addition, discrimination together with the disproportionate level of exposure to targeted marketing of unhealthy foods (especially high-fat high-sugar foods) in Black and Latino consumers may exacerbate the adverse health effects and worsen health disparities99,100.
We found that individuals who experienced more discrimination showed a decreased reactivity in the vmPFC when exposed to unhealthy sweet food but this was not observed with the unhealthy savory foods. It is probable that the observed difference is specific to the sweet feature. The vmPFC, along with the adjacent medial part of the orbitofrontal cortex, encodes the pleasantness or value of taste and flavor101,102, including the perception of carbohydrate content in food cues103. Exposure to stress is associated with attenuated sweet taste104. African Americans have shown heightened and sustained desire for intense sweet tastes, as well as greater perceived stress, relative to White Americans91. It is also possible that this attenuation of sweet perception is a result of increased consumption of sweet food, as higher dietary sugar intake has been found to decrease the perceived sweetness of sweet food105.
The observed discrimination-related BGM disruptions may be associated with an unhealthy diet. Perceived day-to-day racial discrimination is known to be linked to unhealthy eating habits106, which can trigger inflammation in the BGM system, as implicated in obesity pathogenesis86. A high-fat high-sugar diet could alter gut microbiome diversity and increase Gram-negative bacteria rich in endotoxin lipopolysaccharides as well as increase gut permeability, increasing the translocation of lipopolysaccharides across the intestinal epithelium and promoting local and CNS inflammation86. In addition to inflammation, oxidative stress and dyslipidemic processes, high-fat-diet-induced obesity is linked to altered brain neurotransmitter glutamate levels in rats43. Stress and stress-induced unhealthy eating have a detrimental effect on the glutamatergic system. Inflammatory cytokines can influence glutamate metabolism through effects on astrocytes and microglia80. Modulation of glutamatergic receptor activity along the BGM axis may influence gut and brain functions and participate in the pathogenesis of local and brain disorders, such as anxiety and depressive disorders107.
In this study glutamate metabolites were associated with greater neural response to food cues in the frontal-striatal network with higher discrimination exposure. The frontal-striatum (limbic) network is driven by glutamatergic and dopaminergic neurotransmission in humans48. Frontal glutamate plays an important role in reward-guided decision-making in humans108 and modulates fronto-limbic connectivity109. In mice, a high-fat high-sugar diet alters glutamate transmission in the dorsal striatum, a core region implicated in food motivation and reward processing110. Given the limited literature on the exact role of specific glutamate metabolites, further research is warranted to elucidate the finer and more direct associations between these metabolites and their role in communicating with the brain.
Limitations and future directions
Some of the limitations of this study, in which discrimination-related differences in neural responses to food cues and gut metabolites were examined, merit consideration. Although we controlled for sex in the analyses, we acknowledge that men were under-represented. Previous studies suggested that gut-induced alterations in CNS neurochemicals may be sex-specific111,112. Our study did not have sufficient samples of specific racial/ethnic groups to conduct stratified analyses by group. Therefore, future research with larger and more balanced samples should attempt to replicate these results and explore the potential moderating effects of sex and race/ethnicity and source of discrimination. Finally, this was a correlational study; accordingly, longitudinal studies are needed to explore the causal effects of discrimination exposure and altered BGM signatures.
Conclusions
In this study we have elucidated the impact of self-reported discrimination on brain food-cue reactivity and gut microbiome interactions utilizing a systems-biology approach. We demonstrated that experiences of discrimination lead to disruptions in the BGM system, with altered neural response to food cues in regions associated with reward processing and executive control as well as gut glutamate metabolites implicated in stress and inflammation. These alterations may confer vulnerability to obesity and obesity-related comorbidities in individuals with more exposure to discrimination. Thus, brain-targeted treatments (for example, brain stimulation) that could dampen an overactive food-reward system or enhance frontal control could potentially be used as a neuromodulatory tool to normalize altered brain circuits associated with discrimination exposure113. It is also possible to target glutamatergic pathways, such as by a probiotic supplement or Mediterranean diet with anti-inflammatory benefits, as a therapeutic approach for the treatment of stress-related experiences such as discrimination114,115,116.
Methods
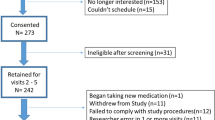
Study participants
The study group was comprised of 107 individuals (87 women) recruited from the Los Angeles community through advertisements and local clinics. Peri- and post-menopausal women were excluded, as determined by the self-reported last day of the previous cycle, and enrolled women were scanned during the follicular phase of the menstrual cycle. Participants were excluded if they had any major medical/neurological conditions, current or past psychiatric illnesses, comorbidities such as vascular disease or diabetes, weight loss/abdominal surgeries, substance-use disorders, tobacco dependence (half a pack or more daily) or metal implants and if they used medications that interfere with the CNS, regularly used analgesics, were pregnant or breastfeeding, or performed extreme strenuous exercise (>8 h of continuous exercise per week). Participants whose weight exceeded 181 kg (400 pounds) were excluded due to weight constraints of the MRI scanner.
All procedures complied with institutional guidelines and were approved by the Institutional Review Board at UCLA’s Office of Protection for Research Subjects. All participants provided written informed consent.
Participant data included BMI, race, age, sex, SES117 and diet (Supplementary Methods and Supplementary Table 1). Diet was categorized into standard or nonstandard American diet based on self-reported questionnaires where participants report which diet is consumed on a regular basis in our analyses as defined in previous studies (Supplementary Table 1)33. Multimodal data, including functional MRI imaging (fMRI), fecal metabolomics and clinical and behavioral measures were also collected.
Clinical and behavioral assessments
Participants completed the validated and widely used EDS118, which measures chronic experiences of unfair treatment118,119,120. The EDS is a validated and widely used measure that captures chronic experiences of unfair treatment in various domains of life. The EDS does not specifically target discrimination based on race, gender, age or poverty but rather assesses overall experiences of discrimination in daily life. For example, one of the questions in the EDS asks participants ‘In your day-to-day life, how often do any of the following things happen to you? You are treated with less courtesy than other people are.’. This demonstrates that our measure of discrimination is not limited to any specific type but encompasses a broad range of unfair treatment experiences. Because there is no consensus on the cut-offs of the EDS, scores were dichotomized to categorize participants into two groups—high discrimination exposure (EDS > 10, n = 50) and low discrimination exposure (EDS ≤ 10, n = 57)—based on the median score of this sample, as used in previous studies33,120,121,122. Participants were excluded if their EDS score was zero due to their distinct nature in reporting discrimination (unwilling or unable to report)123.
Baseline characteristics
Baseline demographic and clinical characteristics were compared in the R software124 using a Student’s t-test for continuous variables and a χ2 test for categorical variables. A two-way analysis of variance was conducted to examine the interaction effect between discrimination groups (high versus low discrimination) and dietary style (American versus non-American) on BMI.
Food-cue task-MRI acquisition, processing and analyses
Brain data were acquired using a 3.0 T Prisma MRI scanner (Siemens); acquisition details are provided in Supplementary Methods. Participants were asked to fast for approximately 6 h previous to scanning and this was confirmed by the study coordinator before scanning took place. Participants completed the food-cue task in the scanner to evaluate neural responses to different types of foods. Pictures were organized into five groups: unhealthy (high calorie) savory, unhealthy (high calorie) sweet, healthy (low calorie) savory, healthy (low calorie) sweet and nonfood, comprising pixelated images created from food pictures (as a control comparison). All food images were uploaded to the E-prime software125; half were copied and pixelated to control for color, brightness and contrast. Images were arranged into blocks of six, comprising either unaltered or pixelated images only, with a total of 18 blocks. Each image was shown for 3 s. A black screen with a white crosshair was displayed for 12 s before the first block of images, between each block of images and after the final block of images. Two slideshows (order 1 and order 2) were created using the same 18 blocks of images arranged in different orders. Participants watched both sets of images in the scanner.
At the end of the scan, participants reported their willingness to eat the food items they saw in the scanner by answering the question ‘How much do you want to eat what you just saw?’. The response options ranged from zero (not at all) to ten (very much).
Neuroimaging data were processed using the fMRI Expert Analysis Tool (FEAT; version 6.0) included in the FMRIB Software Library (FSL)126. Preprocessing included motion correction, brain extraction, 100-s high-pass filtering and spatial smoothing with a 5-mm full-width at half-maximum Gaussian kernel. Functional data were aligned to the structural image of each participant and then registered into Montreal Neurological Institute (MNI) standard space using affine transformation through FSL’s Linear Image Registration Tool (FLIRT).
Whole-brain analysis
To determine discrimination-related differences in food-cue reactivity towards specific food types, we specified the following contrasts: (1) unhealthy sweet food versus nonfood, (2) unhealthy savory food versus nonfood, (3) healthy food versus nonfood, (4) unhealthy sweet food versus healthy sweet food and (5) unhealthy savory food versus healthy savory food. The corresponding reversed contrasts were specified. For each participant, ten contrast maps were created in the first-level analysis, which were then imputed into random-effects group-level analyses using FSL’s Local Analysis of Mixed Effects (FLAME1) in a whole-brain analysis with outlier de-weighting. Group-level (high versus low discrimination) unpaired Student’s t-tests were performed in FEAT using a mixed-effects model with BMI, age, sex, race, diet and SES as covariates. All statistical maps were family-wise error cluster-corrected for multiple comparisons (cluster height threshold, Z > 2.3; cluster significance, P < 0.05).
Discrimination-related food-cue ROI analysis
Significant clusters in the contrasts from the whole-brain analysis (high versus low discrimination) were combined to create a discrimination-related food-cue ROI mask. Brain signal changes (β values from the first-level statistical models) were extracted separately for each participant. Multiple linear regression analyses were conducted to test the effect of discrimination exposure on brain signal change in the composite food-cue ROI for each contrast, adjusting for BMI, age, sex, race, diet and SES, and correcting for multiple comparisons using the false discovery rate (FDR) according to the Benjamini–Hochberg procedure127. This step was used to confirm the robustness of discrimination-related food-cue activity in a linear fashion, and the brain signal extracted from the composite food-cue ROI was further used in an SEM analysis.
Fecal metabolites collection, processing and analyses
Fecal collection and processing was conducted on a subsample of participants (n = 62) as previously described128 and detailed in Supplementary Methods. The fecal samples were stored at −80 °C and shipped to Metabolon for processing and analysis as a single batch on their global metabolomics and bioinformatics platform using ultrahigh-performance liquid chromatography and tandem mass spectrometry129. Raw data were curated by mass spectrometry using specialized software as previously described129. The amount of missing data was low (<3%). However, missing values of raw data were filled using the median value and ineffective peaks were removed through the interquartile range denoising method. In addition, the internal standard normalization method was employed in the data analysis. A dataset for multiple classification analysis was compiled from the metabolite profiling results and a three-dimensional matrix involving metabolite numbers, sample names and normalized peak intensities was used as input to the MetaboAnalyst web software version 3.0 (http://www.metaboanalyst.ca). Because of our a priori interest in the metabolites from the glutamate pathway associated with the processes of stress, only glutamate metabolites were included in our analyses.
Gut metabolites
Twelve metabolites from the glutamate pathway were compared between the high and low discrimination groups using generalized linear modeling, controlling for BMI, age, sex, race, diet and SES. Multiple comparisons were corrected for using the FDR method127. Pearson’s correlations were used to assess the associations between the gut metabolites and key psychosocial variables (for example, SES) that showed significant differences between the high and low discrimination groups.
Willingness to eat unhealthy and healthy foods
The willingness of participants to eat based on the ratings of unhealthy or healthy food was compared separately between the high and low discrimination groups using generalized linear modeling, controlling for BMI, sex, age, race, diet and SES.
SEM
The Lavaan package in R130 was used to perform SEM modeling. One latent variable was created for gut metabolites affected by discrimination exposure, as determined in the initial analyses. Three models were developed to illustrate the pathways that link EDS scores and discrimination-related brain and gut signatures. The unhealthy sweet food model included neural reactivity to unhealthy sweet food cues (versus nonfood) extracted from the composite food-cue ROI as the brain feature. The unhealthy savory food model included neural reactivity to unhealthy savory food cues (versus nonfood) extracted from the composite food-cue ROI as the brain feature. The healthy food model included neural reactivity to healthy food cues (versus nonfood) extracted from the composite food-cue ROI as the brain feature. Glutamate metabolites found to differ significantly between the high and low discrimination groups were included as the gut feature. We controlled for BMI, race, diet and SES as covariates. Model fit was assessed using the following indices and criteria: CFI > 0.9, RMSEA < 0.08, GFI > 0.9 and SRMR < 0.08 (ref. 131). The significance level was set at P < 0.05 for all SEM statistical significance testing.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
De-identified individual participant data (brain) can be shared on request and will be made available through the Center’s pain repository portal (https://www.painrepository.org/). To access the data, participants will fill out a user agreement, following which access to the data will be made available through a secure password-protected portal. The raw microbiome sequences can be accessed at NIH NCBI BioProject (BioProject ID: PRJNA946906).
Code availability
All data analyses used readily available programs (for example, FSL, FEAT and so on) and open-source R code.
References
Flegal, K. M., Carroll, M. D., Kit, B. K. & Ogden, C. L. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 307, 491–497 (2012).
Kenney, M. K., Wang, J. & Iannotti, R. Residency and racial/ethnic differences in weight status and lifestyle behaviors among US youth. J. Rural Health 30, 89–100 (2014).
Jackson, C. L. et al. Black–white disparities in overweight and obesity trends by educational attainment in the United States, 1997–2008. J. Obes. 2013, 140743 (2013).
Sharma, S., Malarcher, A. M., Giles, W. H. & Myers, G. Racial, ethnic and socioeconomic disparities in the clustering of cardiovascular disease risk factors. Ethn. Dis. 14, 43–48 (2004).
Singleton, C. R., Affuso, O. & Sen, B. Decomposing racial disparities in obesity prevalence: variations in retail food environment. Am. J. Prev. Med. 50, 365–372 (2016).
Byrd, A. S., Toth, A. T. & Stanford, F. C. Racial disparities in obesity treatment. Curr. Obes. Rep. 7, 130–138 (2018).
Clark, U. S., Miller, E. R. & Hegde, R. R. Experiences of discrimination are associated with greater resting amygdala activity and functional connectivity. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 3, 367–378 (2018).
Fani, N., Carter, S. E., Harnett, N. G., Ressler, K. J. & Bradley, B. Association of racial discrimination with neural response to threat in Black women in the US exposed to trauma. JAMA Psychiatry 78, 1005–1012 (2021).
Yip, T. Ethnic/racial identity—a double-edged sword? Associations with discrimination and psychological outcomes. Curr. Dir. Psychol. Sci. 27, 170–175 (2018).
Williams, D. R., Lawrence, J. A., Davis, B. A. & Vu, C. Understanding how discrimination can affect health. Health Serv. Res. 54, 1374–1388 (2019).
Kessler, R. C., Mickelson, K. D. & Williams, D. R. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J. Health Soc. Behav. 40, 208–230 (1999).
Bastos, J. L., Celeste, R. K., Silva, D. A. S., Priest, N. & Paradies, Y. C. Assessing mediators between discrimination, health behaviours and physical health outcomes: a representative cross-sectional study. Soc. Psychiatry Psychiatr. Epidemiol. 50, 1731–1742 (2015).
Paradies, Y. et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS ONE 10, e0138511 (2015).
Shankar, A. & Hinds, P. Perceived discrimination: associations with physical and cognitive function in older adults. Health Psychol. 36, 1126–1134 (2017).
Kim, S., Im, E.-O., Liu, J. & Ulrich, C. Maternal age patterns of preterm birth: exploring the moderating roles of chronic stress and race/ethnicity. Ann. Behav. Med. 54, 653–664 (2020).
Sinha, R. Role of addiction and stress neurobiology on food intake and obesity. Biol. Psychol. 131, 5–13 (2018).
Rudenga, K. J., Sinha, R. & Small, D. M. Acute stress potentiates brain response to milkshake as a function of body weight and chronic stress. Int. J. Obes. 37, 309–316 (2013).
Tryon, M. S., Carter, C. S., DeCant, R. & Laugero, K. D. Chronic stress exposure may affect the brain’s response to high calorie food cues and predispose to obesogenic eating habits. Physiol. Behav. 120, 233–242 (2013).
Berthoud, H.-R. The neurobiology of food intake in an obesogenic environment. Proc. Nutr. Soc. 71, 478–487 (2012).
Miller, A. L. & Lumeng, J. C. Pathways of association from stress to obesity in early childhood. Obesity 26, 1117–1124 (2018).
Seeman, T. E., Singer, B. H., Rowe, J. W., Horwitz, R. I. & McEwen, B. S. Price of adaptation—allostatic load and its health consequences. MacArthur studies of successful aging. Arch. Intern. Med. 157, 2259–2268 (1997).
Miller, H. N., LaFave, S., Marineau, L., Stephens, J. & Thorpe, R. J. Jr The impact of discrimination on allostatic load in adults: an integrative review of literature. J. Psychosom. Res. 146, 110434 (2021).
Ávila, P. R. M. et al. Effects of microbiota transplantation and the role of the vagus nerve in gut–brain axis in animals subjected to chronic mild stress. J. Affect. Disord. 277, 410–416 (2020).
Doney, E., Cadoret, A., Dion‐Albert, L., Lebel, M. & Menard, C. Inflammation‐driven brain and gut barrier dysfunction in stress and mood disorders. Eur. J. Neurosci. 55, 2851–2894 (2022).
Maltz, R. M. et al. Social stress affects colonic inflammation, the gut microbiome, and short chain fatty acid levels and receptors. J. Pediatr. Gastroenterol. Nutr. 68, 533–540 (2019).
Wiley, N. C., Cryan, J. F., Dinan, T. G., Ross, R. P. & Stanton, C. Production of psychoactive metabolites by gut bacteria. Mod. Trends Psychiatry 32, 74–99 (2021).
Hantsoo, L. et al. Childhood adversity impact on gut microbiota and inflammatory response to stress during pregnancy. Brain Behav. Immun. 75, 240–250 (2019).
Hatzenbuehler, M. L. et al. Smaller hippocampal volume among Black and Latinx youth living in high-stigma contexts. J. Am. Acad. Child Adolesc. Psychiatry https://doi.org/10.1016/j.jaac.2021.08.017 (2021).
Vargas, T. G. & Mittal, V. A. Testing whether implicit emotion regulation mediates the association between discrimination and symptoms of psychopathology in late childhood: an RDoC perspective. Dev. Psychopathol. https://doi.org/10.1017/S0954579421000638 (2021).
Wang, H., Braun, C. & Enck, P. How the brain reacts to social stress (exclusion)—a scoping review. Neurosci. Biobehav. Rev. 80, 80–88 (2017).
Masten, C. L., Telzer, E. H. & Eisenberger, N. I. An fMRI investigation of attributing negative social treatment to racial discrimination. J. Cogn. Neurosci. 23, 1042–1051 (2011).
Meyer, C. S., Schreiner, P. J., Lim, K., Battapady, H. & Launer, L. J. Depressive symptomatology, racial discrimination experience, and brain tissue volumes observed on magnetic resonance imaging: the CARDIA Study. Am. J. Epidemiol. 188, 656–663 (2019).
Dong, T. S. et al. How discrimination gets under the skin: biological determinants of discrimination associated with dysregulation of the brain–gut microbiome system and psychological symptoms. Biol. Psychiatry 94, 203–214 (2022).
McEwen, B. S. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol. Rev. 87, 873–904 (2007).
Liston, C., McEwen, B. S. & Casey, B. J. Psychosocial stress reversibly disrupts prefrontal processing and attentional control. Proc. Natl Acad. Sci. USA 106, 912–917 (2009).
Dias-Ferreira, E. et al. Chronic stress causes frontostriatal reorganization and affects decision-making. Science 325, 621–625 (2009).
Neseliler, S., Han, J.-E. & Dagher, A. in Appetite and Food Intake 2nd edn (ed. Harris, R. B. S.) 117–1134 (CRC Press, 2017).
Madison, A. & Kiecolt-Glaser, J. K. Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr. Opin. Behav. Sci. 28, 105–110 (2019).
Breton, J. et al. Gut commensal E. coli proteins activate host satiety pathways following nutrient-induced bacterial growth. Cell Metab. 23, 324–334 (2016).
Cruzat, V., Macedo Rogero, M., Noel Keane, K., Curi, R. & Newsholme, P. Glutamine: metabolism and immune function, supplementation and clinical translation. Nutrients 10, 1564 (2018).
McNally, L., Bhagwagar, Z. & Hannestad, J. Inflammation, glutamate, and glia in depression: a literature review. CNS Spectr. 13, 501–510 (2008).
Bermudo-Soriano, C. R., Perez-Rodriguez, M. M., Vaquero-Lorenzo, C. & Baca-Garcia, E. New perspectives in glutamate and anxiety. Pharmacol. Biochem. Behav. 100, 752–774 (2012).
Labban, R. S. M. et al. High-fat diet-induced obesity and impairment of brain neurotransmitter pool. Transl. Neurosci. 11, 147–160 (2020).
Coley, E. J. L. et al. Early life adversity predicts brain-gut alterations associated with increased stress and mood. Neurobiol. Stress 15, 100348 (2021).
Schiavone, S., Colaianna, M. & Curtis, L. Impact of early life stress on the pathogenesis of mental disorders: relation to brain oxidative stress. Curr. Pharm. Des. 21, 1404–1412 (2015).
Dong, X.-X., Wang, Y. & Qin, Z.-H. Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacol. Sin. 30, 379–387 (2009).
Jett, J. D., Bulin, S. E., Hatherall, L. C., McCartney, C. M. & Morilak, D. A. Deficits in cognitive flexibility induced by chronic unpredictable stress are associated with impaired glutamate neurotransmission in the rat medial prefrontal cortex. Neuroscience 346, 284–297 (2017).
Gleich, T. et al. Frontal glutamate and reward processing in adolescence and adulthood. Brain Struct. Funct. 220, 3087–3099 (2015).
Grenham, S., Clarke, G., Cryan, J. F. & Dinan, T. G. Brain–gut–microbe communication in health and disease. Front. Physiol. 2, 94 (2011).
Darbor, K. E., Lench, H. C. & Carter-Sowell, A. R. Do people eat the pain away? The effects of acute physical pain on subsequent consumption of sweet-tasting food. PLoS ONE 11, e0166931 (2016).
Mysels, D. J. & Sullivan, M. A. The relationship between opioid and sugar intake: review of evidence and clinical applications. J. Opioid Manag. 6, 445–452 (2010).
Greenberg, D. & St Peter, J. V. Sugars and sweet taste: addictive or rewarding? Int. J. Environ. Res. Public Health 18, 9791 (2021).
Tan, H.-E. et al. The gut–brain axis mediates sugar preference. Nature 580, 511–516 (2020).
Benarroch, E. E. Neural control of feeding behavior: overview and clinical correlations. Neurology 74, 1643–1650 (2010).
van der Laan, L. N., de Ridder, D. T., Viergever, M. A. & Smeets, P. A. M. The first taste is always with the eyes: a meta-analysis on the neural correlates of processing visual food cues. Neuroimage 55, 296–303 (2011).
Tang, D. W., Fellows, L. K., Small, D. M. & Dagher, A. Food and drug cues activate similar brain regions: a meta-analysis of functional MRI studies. Physiol. Behav. 106, 317–324 (2012).
Maier, S. U., Makwana, A. B. & Hare, T. A. Acute stress impairs self-control in goal-directed choice by altering multiple functional connections within the brain’s decision circuits. Neuron 87, 621–631 (2015).
Neseliler, S. et al. Academic stress and personality interact to increase the neural response to high-calorie food cues. Appetite 116, 306–314 (2017).
Lyu, Z. & Jackson, T. Acute stressors reduce neural inhibition to food cues and increase eating among binge eating disorder symptomatic women. Front. Behav. Neurosci. 10, 188 (2016).
Ott, T. & Nieder, A. Dopamine and cognitive control in prefrontal cortex. Trends Cogn. Sci. 23, 213–234 (2019).
Busemeyer, J. R., Gluth, S., Rieskamp, J. & Turner, B. M. Cognitive and neural bases of multi-attribute, multi-alternative, value-based decisions. Trends Cogn. Sci. 23, 251–263 (2019).
Rose, J. E. et al. Repetitive transcranial magnetic stimulation of the superior frontal gyrus modulates craving for cigarettes. Biol. Psychiatry 70, 794–799 (2011).
Brown, K. L., Graham, A. K., Perera, R. A. & LaRose, J. G. Eating to cope: advancing our understanding of the effects of exposure to racial discrimination on maladaptive eating behaviors. Int. J. Eat. Disord. 55, 1744–1752 (2022).
Schulte, E. M., Yokum, S., Jahn, A. & Gearhardt, A. N. Food cue reactivity in food addiction: a functional magnetic resonance imaging study. Physiol. Behav. 208, 112574 (2019).
Hare, T. A., Camerer, C. F. & Rangel, A. Self-control in decision-making involves modulation of the vmPFC valuation system. Science 324, 646–648 (2009).
Kober, H. et al. Prefrontal–striatal pathway underlies cognitive regulation of craving. Proc. Natl Acad. Sci. USA 107, 14811–14816 (2010).
Scharmüller, W., Übel, S., Ebner, F. & Schienle, A. Appetite regulation during food cue exposure: a comparison of normal-weight and obese women. Neurosci. Lett. 518, 106–110 (2012).
Bowerman, K. L. et al. Disease-associated gut microbiome and metabolome changes in patients with chronic obstructive pulmonary disease. Nat. Commun. 11, 5886 (2020).
Liu, R. et al. Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Nat. Med. 23, 859–868 (2017).
Ahmed, H. et al. Microbiota-derived metabolites as drivers of gut–brain communication. Gut Microbes 14, 2102878 (2022).
Matsumoto, M. et al. Cerebral low-molecular metabolites influenced by intestinal microbiota: a pilot study. Front. Syst. Neurosci. 7, 9 (2013).
Kawase, T. et al. Gut microbiota of mice putatively modifies amino acid metabolism in the host brain. Br. J. Nutr. 117, 775–783 (2017).
Alonso, E., García-Pérez, M. A., Bueso, J. & Rubio, V. N-acetyl-l-glutamate in brain: assay, levels, and regional and subcellular distribution. Neurochem. Res. 16, 787–794 (1991).
Morland, C. & Nordengen, K. N-acetyl-aspartyl-glutamate in brain health and disease. Int. J. Mol. Sci. 23, 1268 (2022).
Bourdon, A. K. et al. Metabolomic analysis of mouse prefrontal cortex reveals upregulated analytes during wakefulness compared to sleep. Sci. Rep. 8, 11225 (2018).
Yelamanchi, S. D. et al. A pathway map of glutamate metabolism. J. Cell Commun. Signal. 10, 69–75 (2016).
Cui, W. et al. Crosstalk between inflammation and glutamate system in depression: signaling pathway and molecular biomarkers for ketamine’s antidepressant effect. Mol. Neurobiol. 56, 3484–3500 (2019).
Oh, S. M. & Betz, A. L. Interaction between free radicals and excitatory amino acids in the formation of ischemic brain edema in rats. Stroke 22, 915–921 (1991).
Haroon, E., Miller, A. H. & Sanacora, G. Inflammation, glutamate, and glia: a trio of trouble in mood disorders. Neuropsychopharmacology 42, 193–215 (2017).
Haroon, E. & Miller, A. H. Inflammation effects on brain glutamate in depression: mechanistic considerations and treatment implications. Curr. Top. Behav. Neurosci. 31, 173–198 (2016).
Maltais-Payette, I. et al. Large-scale analysis of circulating glutamate and adipose gene expression in relation to abdominal obesity. Amino Acids 54, 1287–1294 (2022).
Petrus, P. et al. Glutamine links obesity to inflammation in human white adipose tissue. Cell Metab. 31, 375–390.e11 (2020).
Kiecolt-Glaser, J. K. Stress, food, and inflammation: psychoneuroimmunology and nutrition at the cutting edge. Psychosom. Med. 72, 365–369 (2010).
Epel, E., Lapidus, R., McEwen, B. & Brownell, K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology 26, 37–49 (2001).
Kim, Y., Yang, H. Y., Kim, A.-J. & Lim, Y. Academic stress levels were positively associated with sweet food consumption among Korean high-school students. Nutrition 29, 213–218 (2013).
Jamar, G., Ribeiro, D. A. & Pisani, L. P. High-fat or high-sugar diets as trigger inflammation in the microbiota-gut-brain axis. Crit. Rev. Food Sci. Nutr. 61, 836–854 (2021).
Gupta, A., Osadchiy, V. & Mayer, E. A. Brain–gut–microbiome interactions in obesity and food addiction. Nat. Rev. Gastroenterol. Hepatol. 17, 655–672 (2020).
Kelly, J. R. et al. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front. Cell. Neurosci. 14, 392 (2015).
Foster, J. A., Rinaman, L. & Cryan, J. F. Stress & the gut–brain axis: regulation by the microbiome. Neurobiol. Stress 7, 124–136 (2017).
Pepino, M. Y. & Mennella, J. A. Factors contributing to individual differences in sucrose preference. Chem. Senses 30, i319–i320 (2005).
Schiffman, S. S., Graham, B. G., Sattely-Miller, E. A. & Peterson-Dancy, M. Elevated and sustained desire for sweet taste in African-Americans: a potential factor in the development of obesity. Nutrition 16, 886–893 (2000).
Dallman, M. F. et al. Chronic stress and obesity: a new view of ‘comfort food’. Proc. Natl Acad. Sci. USA 100, 11696–11701 (2003).
Oliver, G., Wardle, J. & Gibson, E. L. Stress and food choice: a laboratory study. Psychosom. Med. 62, 853–865 (2000).
Kandiah, J., Yake, M., Jones, J. & Meyer, M. Stress influences appetite and comfort food preferences in college women. Nutr. Res. 26, 118–123 (2006).
Letzen, J. E. et al. Ethnic disparities in pain processing among healthy adults: μ-opioid receptor binding potential as a putative mechanism. Pain 161, 810–820 (2020).
Gordon, J. L., Johnson, J., Nau, S., Mechlin, B. & Girdler, S. S. The role of chronic psychosocial stress in explaining racial differences in stress reactivity and pain sensitivity. Psychosom. Med. 79, 201–212 (2017).
Varastehmoradi, B. et al. Kappa opioid activation changes protein profiles in different regions of the brain relevant to depression. Eur. Neuropsychopharmacol. 72, 9–17 (2023).
Anderson, G. Pathoetiology and pathophysiology of borderline personality: role of prenatal factors, gut microbiome, mu- and kappa-opioid receptors in amygdala–PFC interactions. Prog. Neuropsychopharmacol. Biol. Psychiatry 98, 109782 (2020).
Grier, S. A. & Kumanyika, S. K. The context for choice: health implications of targeted food and beverage marketing to African Americans. Am. J. Public Health 98, 1616–1629 (2008).
Barnhill, A. et al. The racialized marketing of unhealthy foods and beverages: perspectives and potential remedies. J. Law Med. Ethics 50, 52–59 (2022).
Okamoto, M. & Dan, I. Extrinsic information influences taste and flavor perception: a review from psychological and neuroimaging perspectives. Semin. Cell Dev. Biol. 24, 247–255 (2013).
Ohla, K., Toepel, U., le Coutre, J. & Hudry, J. Visual–gustatory interaction: orbitofrontal and insular cortices mediate the effect of high-calorie visual food cues on taste pleasantness. PLoS ONE 7, e32434 (2012).
Suzuki, S., Cross, L. & O’Doherty, J. P. Elucidating the underlying components of food valuation in the human orbitofrontal cortex. Nat. Neurosci. 20, 1780–1786 (2017).
Al’Absi, M., Nakajima, M., Hooker, S., Wittmers, L. & Cragin, T. Exposure to acute stress is associated with attenuated sweet taste. Psychophysiology 49, 96–103 (2012).
Wise, P. M., Nattress, L., Flammer, L. J. & Beauchamp, G. K. Reduced dietary intake of simple sugars alters perceived sweet taste intensity but not perceived pleasantness. Am. J. Clin. Nutr. 103, 50–60 (2016).
Rodrigues, Y. E., Fanton, M., Novossat, R. S. & Canuto, R. Perceived racial discrimination and eating habits: a systematic review and conceptual models. Nutr. Rev. 80, 1769–1786 (2022).
Baj, A. et al. Glutamatergic signaling along the microbiota–gut–brain axis. Int. J. Mol. Sci. 20, 1482 (2019).
Jocham, G., Hunt, L. T., Near, J. & Behrens, T. E. J. A mechanism for value-guided choice based on the excitation–inhibition balance in prefrontal cortex. Nat. Neurosci. 15, 960–961 (2012).
Duncan, N. W. et al. Glutamate concentration in the medial prefrontal cortex predicts resting-state cortical–subcortical functional connectivity in humans. PLoS ONE 8, e60312 (2013).
Fritz, B. M., Muñoz, B., Yin, F., Bauchle, C. & Atwood, B. K. A high-fat, high-sugar ‘Western’ diet alters dorsal striatal glutamate, opioid, and dopamine transmission in mice. Neuroscience 372, 1–15 (2018).
Heijtz, R. D. et al. Normal gut microbiota modulates brain development and behavior. Proc. Natl Acad. Sci. USA 108, 3047–3052 (2011).
Kelly, J. R. et al. Lost in translation? The potential psychobiotic Lactobacillus rhamnosus (JB-1) fails to modulate stress or cognitive performance in healthy male subjects. Brain Behav. Immun. 61, 50–59 (2017).
Göbel, C. H., Tronnier, V. M. & Münte, T. F. Brain stimulation in obesity. Int. J. Obes. 41, 1721–1727 (2017).
Park, C. et al. Probiotics for the treatment of depressive symptoms: an anti-inflammatory mechanism? Brain Behav. Immun. 73, 115–124 (2018).
Tosti, V., Bertozzi, B. & Fontana, L. Health benefits of the Mediterranean diet: metabolic and molecular mechanisms. J. Gerontology A 73, 318–326 (2018).
De Filippis, F. et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 65, 1812–1821 (2016).
Adler, N. E., Epel, E. S., Castellazzo, G. & Ickovics, J. R. Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy, White women. Health Psychol. 19, 586–592 (2000).
Williams, D. R., Yan, Y., Jackson, J. S. & Anderson, N. B. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J. Health Psychol. 2, 335–351 (1997).
Gee, G. C., Spencer, M. S., Chen, J. & Takeuchi, D. A nationwide study of discrimination and chronic health conditions among Asian Americans. Am. J. Public Health 97, 1275–1282 (2007).
Beatty Moody, D. L., Chang, Y., Brown, C., Bromberger, J. T. & Matthews, K. A. Everyday discrimination and metabolic syndrome incidence in a racially/ethnically diverse sample: study of women’s health across the nation. Psychosom. Med. 80, 114–121 (2018).
Gregoski, M. J. et al. Interactive influences of ethnicity, endothelin-1 gene, and everyday discrimination upon nocturnal ambulatory blood pressure. Ann. Behav. Med. 45, 377–386 (2013).
Ajrouch, K. J., Reisine, S., Lim, S., Sohn, W. & Ismail, A. Perceived everyday discrimination and psychological distress: does social support matter? Ethn. Health 15, 417–434 (2010).
Beccia, A. L., Jesdale, W. M. & Lapane, K. L. Associations between perceived everyday discrimination, discrimination attributions, and binge eating among Latinas: results from the National Latino and Asian American Study. Ann. Epidemiol. 45, 32–39 (2020).
R Core Team R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2013).
E-Prime (Psychology Software Tools, Inc., 2002).
Smith, S. M. et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage 23, S208–S219 (2004).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Series B 57, 289–300 (1995).
Osadchiy, V. et al. Analysis of brain networks and fecal metabolites reveals brain–gut alterations in premenopausal females with irritable bowel syndrome. Transl. Psychiatry 10, 367 (2020).
Evans, A. M., DeHaven, C. D., Barrett, T., Mitchell, M. & Milgram, E. Integrated, nontargeted ultrahigh performance liquid chromatography/electrospray ionization tandem mass spectrometry platform for the identification and relative quantification of the small-molecule complement of biological systems. Anal. Chem. 81, 6656–6667 (2009).
Rosseel, Y. lavaan: an R package for structural equation modeling. J. Stat. Softw. 48, 1–36 (2012).
Little, T. D. Longitudinal Structural Equation Modeling (Guilford Press, 2013).
Acknowledgements
This research was supported by grants from the National Institutes of Health (to A.G.; grant nos. R01 MD015904, K23 DK106528, R03 DK121025 and ULTR001881/DK041301 (UCLA CURE/CTSI Pilot and Feasibility Study)) and pilot funds provided for brain scanning by the Ahmanson–Lovelace Brain Mapping Center. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. We acknowledge the analytical and data curation efforts provided by the Neuroimaging Core, the Integrative Biostatistics and Bioinformatics Core, and the Database and Clinical Core of the Goodman–Luskin Microbiome Center at UCLA.
Author information
Authors and Affiliations
Contributions
X.Z.: statistical analysis, drafting of the paper and critical revision of the paper for important intellectual content. H.W.: statistical analysis, data interpretation and visualization. J.S.L.: data interpretation. A.V.: data collection. L.A.K., T.S.D., G.C.G., V.O., H.B.-S. and M.C.W.: data interpretation and critical revision of the paper for important intellectual content. A.G.: funding, study concept and design, statistical analysis and interpretation of data, critical revision of the paper for important intellectual content, technical support and study supervision.
Corresponding author
Ethics declarations
Competing interests
A.G. is a scientific advisor to Yamaha. All other authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks George Anderson, Inigo Ruiz de Azua and Daniel Radford Smith for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Methods and Table 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, X., Wang, H., Kilpatrick, L.A. et al. Discrimination exposure impacts unhealthy processing of food cues: crosstalk between the brain and gut. Nat. Mental Health 1, 841–852 (2023). https://doi.org/10.1038/s44220-023-00134-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00134-9