Abstract
Missing older adults (MOAs) are older adults whose whereabouts cannot be established at present or at any time previously. The MOAs represent a notable intersection of old age and missingness, given the accelerating population aging and sizable missing persons in many societies. However, the prevalence and patterns of mental and cognitive conditions of MOAs have received little attention. This study aimed to address this gap. This study collected data from the Toutiao Alert, a large missing-person appeal platform in China. The analytical sample included 32885 MOAs (mean age, 73.6 years; female, 40.2%) who were reported missing on the platform between 2017 and 2021. The mental and cognitive impairments and other measures were extracted from the reported information. The results show that the overall levels of mental and cognitive impairments among MOAs were 10.6 and 41.5%, respectively. Moreover, these levels varied by gender, age, and spatiotemporal factors such as the region and year of missingness. Women exhibited higher levels of mental and cognitive impairments. Age was associated with lower levels of mental impairments but higher levels of cognitive impairments. Across regions, MOAs from Northeast China had lower levels of mental and cognitive impairments. From 2017 to 2021, the mental or cognitive impairment levels initially decreased, but then increased until the most recent year. The prevalence and patterns of mental and cognitive impairments revealed in this study contributed to our understanding of the health and well-being of MOAs as one of the distinct groups within the expanding elderly population. Future healthcare policies and services targeting MOAs may benefit from these findings.
Similar content being viewed by others
Introduction
Missing persons have long been a subject of interest in crime and deviant-behavior studies (Huey and Ferguson, 2022; Morewitz, 2016). Much attention, however, has been focused on missing children and youth, which has involved reflections on victimizations of parental and peer abuse (Morewitz, 2016) or child abduction and trafficking (Randone and Thomas, 2022; Stevenson and Thomas, 2018; Xin and Cai, 2019). Indeed, the “missing person” entry in Wikipedia covers content exclusively on missing children (Wikipedia contributors, 2022). By contrast, only a handful of studies examined the psychological and cognitive health of missing adults, based primarily on data from police records (Bonny et al. 2016; Huey and Ferguson, 2022; O’Brien et al. 2022) or newspaper reports (Lai et al. 2012; Rowe and Bennett, 2003; Rowe et al. 2011). This study focused on a seldom studied group: the missing older adults (MOAs). Our purpose was to outline the prevalence and patterns of mental and cognitive impairments in this distinct group, using a large digital dataset.
The focus on MOAs is of great relevance in the context of the widespread and continuing acceleration of population aging worldwide. The global percentage of older adults over 60 years will almost double, increasing from 12% in 2015 to 22% in 2050 (World Health Organization, 2020). Consequently, growing efforts have been devoted to specific segments within the older population, such as those with physical disabilities (Van Houtven et al. 2020), in nursing homes (Freedman and Spillman, 2014), or the oldest old (Zeng et al. 2017). However, MOAs as a distinct group have received little direct attention. Although most missing persons will return or be found within just a few days (Lissemore et al. 2019; Newiss and Webb, 1999), a sudden disappearance of a loved one inevitably incurs a grave psychological toll on the family members involved. Also, older adults with missing experience face high risks of repeated missing (Bantry-White and Montgomery, 2015; McShane et al. 1998). Taken together, the MOAs represent an important intersection of missingness and old age (Biehal et al. 2003; Ruiz-Rizzo et al. 2022).
Despite the lack of discussions in prior research, MOAs are quite noticeable in scale, particularly in countries with a large older population. Consider Japan and China as two examples. Japan has the world’s most aging population. In 2021, over 79 thousand missing persons were reported, and over 27 percent of them were older adults (National Police Agency (Japan), 2022). China had 264 million older adults aged 60 and above in 2020, accounting for 18.7% of the population. In 2015, almost 500 thousand older adults were reported missing across the country (Xiong, 2017).
The mental and cognitive issues among older adults have gained increasing prominence: one study reported a global prevalence of depression in older persons approaching 30% (Hu et al. 2022), and the share of this group affected by mild cognitive impairment ranged from 6.7 % for ages 60–64 to 25.2% for ages 80–84 (Petersen et al. 2018). Overall levels of mental and cognitive issues may be higher if both diagnostic and nondiagnostic instruments are used, as well as severe and mild symptoms taken into account. The healthcare for older adults with mental and cognitive impairments represents a grave challenge to the caregiving family members (Victor et al. 2021) and the public health systems (Brookmeyer et al. 2007; Morewitz and Goldstein, 2007; Nichols et al. 2019).
However, there remains a lack of research with explicit attention to the health profiles of MOAs. In gerontological and geriatric research, many studies have narrowly discussed the getting-lost issues among older adults with dementia (Bantry-White and Montgomery, 2015; Bowen et al. 2011; Lai et al. 2012; McShane et al. 1998; Murata et al. 2021), without further attention to those with cognitive impairments other than dementia or mental problems. Also, the target population of these studies was actually cognitively impaired older adults, not the distinct group of MOAs.
Methodologically, current research related to MOAs is largely limited by data. The use of police data, for example, is almost always limited in terms of generalizations of research findings, as researchers could only gain access to archived reports from a small number of local police forces (Alison et al. 2001; Bantry-White and Montgomery, 2015; O’Brien et al. 2022). Studies based on missing reports in newspapers also struggled with the self-selection of news reports with “newsworthiness” (Jeanis and Powers, 2017; Jewkes and Linnemann, 2017) which undermined the representativeness of their findings.
The development of digital technologies has dramatically revolutionized the means of locating missing persons (Ceccato and Petersson, 2022; Jeanis et al. 2021; Morewitz, 2016; Solymosi et al. 2021). Accordingly, large volumes of digital data have been generated, making it possible for a population-based description of the health profiles of MOAs. In this study, we retrieved a large dataset from the Toutiao Alert, an extensive missing-person alert platform operated by a social media company in China. The data allowed us to illustrate the prevalence of mental and cognitive impairments of MOAs at the national level and to delineate further the group-specific variation in health impairments by gender, age, region, and year of missing. This work is essential given the accelerated aging and the concerning coverage of missing persons in many societies. The findings may serve as a reference point for comparison in future studies.
Research design and methods
Data Source
Data were from the Toutiao Alert project, which was initiated by Toutiao, one of China’s largest mobile platforms for aggregating and distributing news and information. Toutiao was launched by the China-based company ByteDance in 2012, and as of 2021, the Toutiao app has been China’s most popular news app, amassing over 332 million monthly active users. Most Toutiao users are young and well-educated: users under age 30 make up 90 percent of Toutiao’s user base. To the best of our knowledge, our dataset collected from the Toutiao Alert platform contains one of the largest samples of MOAs currently available in Chinese society, and represents a significant improvement over previous data sources such as newspapers or local police reports.
In general, the creation and distribution of a missing person appeal follow several steps. First, after collecting and verifying a missing person report, the Toutiao Alert team posted the appeal on their platform. Meanwhile, it pushed notifications to the Toutiao users about information related to the missing person, disclosing the name, gender, age, photographs, date of getting lost, location of getting lost, and other notable features such as clothing, mental state, and cognitive status. Backed up by the location-based notification-pushing techniques, a missing person appeal can be sent to all Toutiao users within a specified radius and, occasionally, may reach all the users within a city. The vast-and-young user base facilitates high visibility of the published missing person appeals. Figure 1 shows a typical format of a missing person appeal illustrated on a mobile phone. Once a missing person was found, the missingness status was updated, and the missing person’s name, photos, and related contact information were removed. However, all other information remained on the platform from which we collected our dataset in this study.
It shows a typical format of a missing person appeal illustrated on a mobile phone. Once a missing person was found, the missingness status was updated, and the missing person’s name, photos, and related contact information were removed. However, all other information remained on the platform from which we collected our dataset in this study.
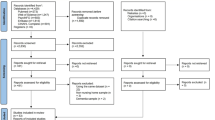
Employing a web-crawler application, we retrieved all the missing person appeals published on the platform between the start of 2017 and the end of 2021, yielding a total of 62812 missing person reports. Of these, individuals under age 60 (n = 29908) and with missing values on age (n = 19) were excluded. As a result, a sample of 32885 MOAs was analyzed.
Coding and derived variables
Mental and cognitive impairments were derived and coded from the “Characteristics” section in a missing person appeal (Fig. 1). On the right side of Fig. 1, we listed several real examples that appeared in our dataset. In the first example, we can observe the phrase “moderate level of dementia”, which can be easily identified and coded as cognitive impairment. In the second example, words like “severe insomnia”, “depression”, and “suicidal tendencies” all point to mental impairments. In the third example, the health status of the missing person was not straightforward but implicitly mentioned. Specifically, we considered the phrases “slurred speech” and “glazed eyes” as symptoms of cognitive impairments. Finally, if neither mental nor cognitive impairments were mentioned, we considered the missing person as “normal”. We created a long list of keywords to identify whether each elderly missing person in our dataset was “normal”, “mentally impaired”, “cognitively impaired”, or “both”. Two of the authors did the coding independently and then worked together to reach an agreement on the unmatched cases.
Table 1 shows part of the keywords used to detect mental and cognitive impairments. Concerning the coding result, only 112 missing persons were described with words indicating both mental and cognitive impairments. Therefore, we coded a coexistence of mental and cognitive impairments simply as cognitively impaired. As such, our outcome variable in the analysis had three categories: 1 = “normal”, 2 = “mental impairment”, and 3 = “cognitive impairment”.
We focused on four key independent variables in outlining the distributive patterns of mental and cognitive impairments. Two are related to demographic characteristics: gender (0 = “male”, 1 = “female”) and age group (“60–64”, “65–69”, “70–74”, “75–79”, and “80+”). Two are related to spatiotemporal characteristics: the region of the missing (1 = “Eastern China”, 2 = “Central China”, 3 = “Western China”, 4 = “Northeastern China”) and the year of missing (“2017,” “2018,” “2019,” “2020,” “2021”).
Several other variables available in the data were included in our regression models as control variables, including the body height of an elderly missing person (1 = “less than 150 cm”, 2 = “150–159 cm”, 3 = “160–169 cm”, 4 = “170–179 cm”, 5 = “180+ cm”, and 6 = “missing”), whether an elderly missing person had been reported to the police (0 = “no”, 1 = “yes”), the time duration between the date of the missingness of an elderly missing person and the date of the missingness-alert on the Toutiao Alert platform (1 = “less than 24 h”, 2 = “1–3 days”, 3 = “3 days or more”), and a dummy variable indicating the updated missing status of an elderly missing person (0 = “already found”, 1 = “still missing”).
Statistical analysis
We performed univariate analysis for the overall levels of mental and cognitive impairments in our dataset. We then performed bivariate analysis to see how the mental and cognitive impairments were spread across gender, age, region, and year of missing. Cross-tabulations with chi-square tests were used to illustrate the bivariate-association patterns and statistical significance. We further used regression analysis to assess the associations while adjusting for other covariates. We used the multinomial logit model because our outcome variable had three categories. Coefficients in odds ratios (OR) and 95% confidence intervals were reported. All p-values were based on two-tailed tests and considered to indicate statistical significance if less than 0.05.
Results
Table 2 presents descriptive statistics for our sample. First, the sample was unevenly distributed by gender: for every four women, there were about six men. This is consistent with the conventional wisdom that men are more likely than women to go missing in the adult population (Bantry-White and Montgomery, 2015; Bonny et al. 2016). Across age groups, the number of MOAs varied somewhat: 16.0% were aged 60–64, 19.6% were aged 65–69, 19.9% were aged 70–74, 16.9% were aged 75–79, and notably, 27.6% were aged 80 and over. The proportion of MOAs appears to be much higher than in the older population overall (Lei et al. 2012; Lei et al. 2014).
In addition to demographic features, Table 2 also presents the spatial and temporal distribution of the MOAs. Regarding the geographical distributions, we found that Eastern China, the most developed region in the country, accounted for 42.8% of the MOAs in our sample. In comparison, 14.7 and 7.6% of the MOAs were reported missing in Western China and Northeastern China, two regions roughly with the lowest development levels. The remaining 31.9% of the MOAs were from Central China, which ranks behind Eastern China yet ahead of Western and Northeastern China in socio-economic development. Over the period 2017–2021, the number of MOAs increased first and then declined. It increased from 4723 (14.4%) in 2017 to a peak of 8931 (27.2%) in 2019, and then decreased to 6610 (20.1%) in 2020 and further down to 5501 (16.7%) in 2021. One possible explanation for such an inverted V-shaped pattern may be related to the profound impact of the COVID-19 pandemic, which broke out initially in late 2019 and then continued to the present. A similar pattern was observed in a recent study with UK data (O’Brien et al. 2022).
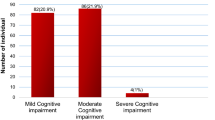
Table 2 reports the overall prevalence of mental and cognitive impairments: 10.6% were reported to have mental impairments, 41.5% were reported to have cognitive impairments, and the remaining 47.9% were reported as “normal.” These percentages reveal a preponderance of cognitive impairments among the MOAs in China.
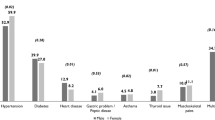
Table 3 shows bivariate associations, splitting the mental and cognitive impairment distribution by gender, age, region, and year of missing. Compared to men, women had a higher prevalence of mental impairments (14.6 vs. 8.0%) and cognitive impairments (43.3 vs. 40.3%). Compared to younger-age groups, older-age groups had lower levels of mental impairments but higher levels of cognitive impairments. Notably, among those aged 80 and over, 47.7% were reported to have certain kinds of cognitive issues, whereas mental problems were hardly ever reported (2.5%). Concerning regional comparisons, the prevalence of cognitive impairments was 44.3% in Central China, 43.7% in Western China, 40.9% in Eastern China, and 27.8% in Northeastern China. The regional variation in mental impairments was relatively small, ranging between 8.6 and 11.1%. Notably, the mental and cognitive impairment levels were comparably low in Northeastern China. Temporally, the prevalence of mental and cognitive impairments declined initially but rebounded in recent years.
Table 4 presents multinomial logit regression results. Women exhibited higher levels of mental and cognitive impairments: ceteris paribus, their odds of having mental impairments were 157.1% higher (OR = 2.571, 95% CI = 2.340–2.825), and the odds of having cognitive impairments were 30.3% (OR = 1.303, 95% CI = 1.230–1.382) higher. The increase in age was associated with lower levels of mental impairments but higher levels of cognitive impairments. The odds of mental impairments among those aged 80+ were 10.9% (OR = 0.109, 95% CI = 0.094–0.127) of the odds among those aged 60–64. In contrast, the odds of cognitive impairments among those aged 80+ were 160.5% (OR = 1.605, 95% CI = 1.482–1.739) of the odds among those aged 60–64. Across regions, MOAs in Northeastern China had a lower likelihood of mental impairments (OR = 0.602, 95% CI = 0.512–0.706) and cognitive impairments (OR = 0.471, 95% CI = 0.427–0.521).
Between 2017 and 2021, the likelihood of mental or cognitive impairments first declined but then substantially increased until the most recent year. The odds of mental impairments decreased by 29.1% in 2018 (OR = 0.709, 95% CI = 0.621–0.810) and by 30.5% in 2019 (OR = 0.695, 95% CI = 0.609–0.795), but significantly increased by 60.7% in 2021 (OR = 1.607, 95% CI = 1.397–1.850), in comparison to the odds of mental impairments in 2017. The odds of cognitive impairments decreased by 18.8% in 2018 (OR = 0.812, 95% CI = 0.749–0.883), by 18.0% in 2019 (OR = 0.820, 95% CI = 0.754–0.890), by 14.6% in 2020 (OR = 0.854, 95% CI = 0.781–0.933), but then significantly increased by 51.0% in 2021 (OR = 1.510, 95% CI = 1.376–1.656). The group-specific predicted probabilities presented in Fig. 2 are derived from the logit estimates while setting the other covariates at their means. Taken together, our bivariate and multiple regression analyses have yielded consistent results regarding the mental and cognitive impairment distributions across gender, age, region, and year of missingness.
Discussion and implications
The MOAs represent an essential intersection between old age and missingness, and their health and well-being deserve more public and policy attention considering the accelerated aging and concerning coverage of missing persons in many societies. We retrieved a large dataset of MOAs (n = 32,885) from an online platform in China to outline the prevalence and patterns of mental and cognitive impairments in this distinct vulnerable group.
In our sample, 52.1% were reported to have mental or cognitive impairments, with cognitive impairments being reported more frequently than mental impairments (41.5 vs. 10.6%). An early study in the UK similarly found that over half of the MOAs aged 60 and over had dementia or mental health problems (Biehal et al. 2003). Prior research has also noticed the particular manifestation of cognitive impairments (Biehal et al. 2003; Xiong, 2017). On the other hand, the relatively lower share of mental impairments may not necessarily indicate fewer psychological challenges. It is likely that when mental and cognitive issues coexist in an elderly missing person, the cognitive problems are more often stressed in a missing-person report. Indeed, depressed older adults tend to display more cognitive symptoms than affective symptoms as they age further (Fiske et al. 2009).
We further assessed whether and how the prevalence of mental and cognitive impairments among MOAs varied by gender, age, region, and year of missing. Our bivariate analysis and multiple regression models yielded consistent results. First, women were more likely than men to have mental and cognitive impairments, even though men usually outnumber women in missing-person reports (Bantry-White and Montgomery, 2015; Bonny et al. 2016). This finding is consistent with prior documents about the whole elderly population that women are more inclined to suffer from mental and cognitive issues (Lei et al. 2012; Lei et al. 2014). Hence, women’s mental and cognitive vulnerabilities in the MOAs may warrant more public and policy attention.
Second, cohort age was associated with the likelihood of mental and cognitive impairments, but notably in opposite directions. The positive link between age and cognitive impairment in our sample echoed prior research on the general older population (Lei et al. 2012; Petersen et al. 2018), but the observed adverse age gradient in mental impairments was just contrary to previous studies on general older adults (Lei et al. 2014).
Third, significant disparities existed across broad regions of China. We found lower mental and cognitive impairment levels in Northeastern China compared to other parts of China. There are several possible explanations for these regional differences. One possibility is that the region of Northeastern China included an outlier province, which has led us to a false conclusion. To test this, we presented scatter plots for mental and cognitive impairment prevalence at both the province and regional levels (see Supplementary Fig. S1). The left part of Supplementary Fig. S1 corresponds to the plot that includes information on 31 provinces. The three provinces belonging to Northeastern China (Heilongjiang, Jilin, and Liaoning) are clustered at the lower left corner of the plot, indicating that relatively low levels of mental and cognitive impairments among MOAs were commonplace in Northeastern China as a whole. This point is well captured by the right-side plot that includes information on four regions. Hence, our finding here was not due to a misclassification of regions.
Another possibility is related to economic development or population structure. To test this, we reran our regression models with the inclusion of a set of province-level characteristics such as GDP per capita, percentage of the urban population, number of older adults over 65, and percentage of older adults over 65. Most of the coefficients for these factors, although statistically significant, probably due to our large sample size, did not suggest meaningful, practical differences. We also compared the goodness-of-fit of these models with our original model with the four-category region variable, and the results are reported in Supplementary Table S1. Our original model with a broader-region variable seems better because it has a lower Akaike Information Criterion (AIC) value and a lower Bayesian Information Criterion (BIC) value. We thus argue that the regional differences in mental and cognitive impairments among MOAs in Northeastern China are not closely linked to economic and demographic backgrounds.
It is also a possibility that people in Northeastern China may tend to underreport mental and cognitive impairment due to their more conservative cultural norms. We already know that the stigma of mental illness and cognitive disabilities has prevailed in traditional Chinese culture (Kong et al. 2022; Lei et al. 2014). In particular, the word “dementia” has long been phrased as “Chi Dai” in Chinese, which literally means stupid and dumb (“Chi” means stupid, and “Dai” means dumb). Despite the recent advocation of alternative Chinese terms for dementia, the derogatory term “Chi Dai” continues to dominate public discourse. Such a cultural explanation can be specifically examined in further research based on better data.
Lastly, from 2017 to 2021, the prevalence of mental and cognitive impairments among MOAs went down at first but then substantially increased in the most recent year (i.e., 2021). The initial decrease in mental and cognitive impairments may be attributed to both the increased public awareness of MOAs and the popularity of the Toutiao Alert platform, which may increase the exposure of MOAs (see Table 2), especially those without mental and cognitive problems, and thus decrease the overall prevalence of mental and cognitive problems in our dataset. The later increase in mental and cognitive impairments may be partly due to the effect of the COVID-19 pandemic. It has been suggested that the plethora of lockdown restrictions in response to the COVID-19 pandemic may profoundly affect the proportion of different types of missing persons reported (O’Brien et al. 2022). Possibly due to China’s persistent and strict social lockdowns, the number of MOAs declined continuously after 2019 (see Table 2). In addition, recent research suggests that social isolation (Li et al. 2022), information overload (Liu et al. 2022), and disruption of routine medical care (Wong et al. 2020) may have contributed to an increased risk of mental and cognitive impairments among older adults during the COVID-19 period. Thus, the proportion of MOA with mental and cognitive impairments increased after 2019, in contrast to the decline in previous years. With the further progress of the pandemic, it is necessary to monitor whether and how the different health dimensions among MOAs may change in the current and post-COVID-19 situation.
This study had several limitations. First, the findings might not be convincingly generalized to the entire missing older population in China. Our results were based on a dataset collected from an online platform, which may have selection issues due to selective uploading or intentional deletion. We thus cannot be confident that our sample will sufficiently represent the overall target population, despite its large sample size (n = 32885). Still, the results in the current study can serve as a benchmark for future studies using data from other social media platforms or sample surveys.
Second, due to the nature of our data, we adopted the reported characteristics of a missing person to identify the actual existence of any cognitive or mental impairments. This reported outcome may not fit well with outcomes of interest to domain-specific experts. For instance, researchers have developed standardized scales to measure mild cognitive impairment (Petersen et al. 2018) and some other scales to assess depressive symptoms for older adults (Andresen et al. 1994; Radloff, 1977). In constructing our measure of cognitive and mental health status, however, we had to rely on the limited data accessed from a pre-existing online platform initially designed for non-research purposes. Indeed, information incompleteness is one of the key features of digital data (Salganik, 2019). Future research may seek to improve the structure of a missing-alert system, hopefully through cooperation with online service providers, to better capture and collect more detailed and accurate health information about a missing person.
Third, we are aware that the patterns of mental and cognitive impairments among MOAs in China have been outlined at the risk of oversimplification. For example, the time trends were presented on a yearly basis. It might be desirable to investigate the seasonal or monthly patterns of mental and cognitive status of MOAs in future research. Furthermore, the regional patterns presented in the current study were based on the East-Central-West-Northeast categorization, without taking into account the possible rural-urban differences. We already know that among the general elderly population in China, urban residents have both higher levels of cognitive ability (Lei et al. 2012) and lower levels of depressive symptoms (Lei et al. 2014). It would be a great addition to the current study if we could further illustrate the urban-rural differences in the prevalence and patterns of mental and cognitive impairment among missing older adults. Unfortunately, our data were limited in providing a reliable urban-rural measure in this regard.
Despite the limitations, the findings of this study could have practical value in raising scholarly and public awareness of the mental and cognitive health status of the MOAs as a special segment of the elderly population. Moreover, the return of the MOAs is not the end of the story. Some of the returned persons would face a high risk of repeated missing. In this regard, the successful prevention of repeat missing incidents requires a better understanding of these MOAs’ mental and cognitive health conditions. Furthermore, return-home interviews may be conducted by police or charitable organizations. We were aware that in some places of the UK, a return-home interview and a safe-and-well check are carried out by trained professionals from charity organizations (All Party Parliamentary Group (APPG), 2018). However, existing professional practice for missing adults remains to rely on good will instead of good data (All Party Parliamentary Group (APPG), 2018). This study represents one of the first attempts to provide cumulative empirical evidence.
Conclusion
Using data from public missing-person appeals on a large social media platform (i.e., Toutiao Alert), our results showed that over half of the MOAs in our sample were reported to have mental and cognitive problems, and cognitive issues were more likely than mental problems to be reported. Moreover, the prevalence of mental and cognitive impairments differed by gender and age of the MOAs and by region and year of missing. The findings of this study could have practical value in raising scholarly and public awareness of the mental and cognitive health status of the MOAs as a special segment of the expanding elderly population. Since the health and well-being of MOAs is still an under-explored area of research, we call for more systematic examinations of this issue in other social contexts or through a cross-national framework.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request. These datasets were derived from the Toutiao Alert platform: https://www.toutiao.com.
References
Alison LJ, Snook B, Stein KL (2001) Unobtrusive measurement: using police information for forensic research. Qual Res 1(2):241–254
All Party Parliamentary Group (APPG) (2018) Inquiry into safeguarding missing adults who have mental health issues. All Party Parliamentary Group, London, In
Andresen EM, Malmgren JA, Carter WB, Patrick DL (1994) Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 10(2):77–84
Bantry-White E, Montgomery P (2015) Dementia, walking outdoors and getting lost: incidence, risk factors and consequences from dementia-related police missing-person reports. Aging Ment. Health 19(3):224–230
Biehal N, Mitchell F, Wade J (2003) Lost from view: missing persons in the UK. Policy Press, Bristol
Bonny E, Almond L, Woolnough P (2016) Adult missing persons: can an investigative framework be generated using behavioural themes? J Investig Psychol Offender Profiling 13(3):296–312
Bowen ME, McKenzie B, Steis M, Rowe M (2011) Prevalence of and antecedents to dementia-related missing incidents in the community. Dement Geriatr Cogn Disord 31(6):406–412
Brookmeyer R, Johnson E, Ziegler-Graham K, Arrighi HM (2007) Forecasting the global burden of Alzheimer’s disease. Alzheimers Dement 3(3):186–191
Ceccato V, Petersson R (2022) Social media and emergency services: information sharing about cases of missing persons in rural sweden. J Plan Lit 37(1):119–119
Fiske A, Wetherell JL, Gatz M (2009) Depression in older adults. Annu Rev Clin Psychol 5:363–389
Freedman VA, Spillman BC (2014) The Residential continuum from home to nursing home: size, characteristics and unmet needs of older adults. J Gerontol Ser B 69(Suppl_1):S42–S50
Hu T, Zhao X, Wu M, Li Z, Luo L, Yang C, Yang F (2022) Prevalence of depression in older adults: A systematic review and meta-analysis. Psychiatry Res 311:114511
Huey L, Ferguson L (2022) ‘Going missing’ as a maladaptive coping behavior for adults experiencing strain. Deviant Behav 43(1):17–29
Jeanis MN, Powers RA (2017) Newsworthiness of missing persons cases: an analysis of selection bias, disparities in coverage, and the narrative framework of news reports. Deviant Behav 38(6):668–683
Jeanis MN, Powers RA, Miley LN, Shunick CE, Storms M (2021) The new milk carton campaign: an analysis of social media engagement with missing persons’ cases. Soc Forces 100(2):454–476
Jewkes Y, Linnemann T (2017) Media and crime in the US. Thousand Oaks: Sage Publications
Kong D, Chen A, Zhang J, Xiang X, Lou WV, Kwok T, Wu B (2022) Public discourse and sentiment toward dementia on Chinese Social Media: Machine Learning analysis of Weibo Posts. J Med Internet Res 24(9):e39805
Lai CKY, Chung JCC, Wong TKS, Faulkner LW, Ng L, Lau LKP (2012) Missing older persons with dementia — a Hong Kong view. Hong Kong J Soc Work 37(02):239–245
Lei XY, Hu YQ, McArdle JJ, Smith JP, Zhao YH (2012) Gender differences in cognition among older adults in China. J Hum Resour 47(4):951–971
Lei XY, Sun XT, Strauss J, Zhang P, Zhao YH (2014) Depressive symptoms and SES among the mid-aged and elderly in China: Evidence from the China Health and Retirement Longitudinal Study national baseline. Soc Sci Med 120:224–232
Li J, Yan C, Yang S, Li Z, Li W, Gui Z, Zhou C (2022) Social isolation transitions and psychological distress among older adults in rural China: A longitudinal study before and during the COVID-19 pandemic. J Affect Disord 308:337–342
Lissemore FM, Shatzman S, Clark N, Nash J, Miller R, Lerner AJ (2019) Dementia reported missing: use of an online search engine to track outcomes in persons With dementia reported missing. Alzheimer Dis Assoc Disord 33(2):142–146
Liu J, Kwan C, Deng J, Hu Y (2022) The mental health impact of the COVID-19 pandemic on older adults in China: A systematic review. Int J Environ Res Public Health 19(21):14362
McShane R, Gedling K, Keene J, Fairburn C, Jacoby R, Hope T (1998) Getting lost in dementia: a longitudinal study of a behavioral symptom. Int Psychogeriatr 10(3):253–260
Morewitz SJ (2016) Missing persons: Forensic sociology factors. In: Steptoe A (Ed.) Handbook of missing persons. Springer, New York, p 93–104
Morewitz SJ, Goldstein ML (2007) Aging and chronic disorders. Springer, New York
Murata S, Takegami M, Onozuka D, Nakaoku Y, Hagihara A, Nishimura K (2021) Incidence and mortality of dementia-related missing and their associated factors: an ecological study in Japan. J Epidemiol 31(6):361–368
National Police Agency (Japan) (2022) Number of people reported missing in Japan in 2021, by age group (in 1,000s). Available via https://www.npa.go.jp/safetylife/seianki/fumei/R03yukuefumeisha.pdf. Accessed 28 Mar 2023
Newiss G, Webb B (1999) Missing presumed…?: The police response to missing persons. Home Office, Policing and Reducing Crime Unit, Research, Development and Statistics Directorate, London
Nichols E, Szoeke CE, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, Aichour MTE, Akinyemi RO, Alahdab F, Asgedom SW (2019) Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18(1):88–106
O’Brien F, Collie C, Greene KS, Giles S (2022) The impact of COVID-19 lockdown restrictions on missing person reports. Polic Soc 32(8):997–1011
Petersen RC, Lopez O, Armstrong MJ, Getchius TS, Ganguli M, Gloss D, Gronseth GS, Marson D, Pringsheim T, Day GS (2018) Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 90(3):126–135
Radloff LS (1977) The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1(3):385–401
Randone J, Thomas SDM (2022) The victim-offender overlaps among Australian youth missing persons. Polic-J Policy Pract
Rowe MA, Bennett V (2003) A look at deaths occurring in persons with dementia lost in the community. Am J Alzheimers Dis Other Dement 18(6):343–348
Rowe MA, Vandeveer SS, Greenblum CA, List CN, Fernandez RM, Mixson NE, Ahn HC (2011) Persons with dementia missing in the community: is it wandering or something unique? BMC Geriatr 11(1):28
Ruiz-Rizzo AL, Archila-Meléndez ME, González Veloza JJF (2022) Predicting the probability of finding missing older adults based on machine learning. J Comput Soc Sci 5(2):1303–1321
Salganik MJ (2019) Bit by bit: social research in the digital age. Princeton University Press, Princeton
Solymosi R, Petcu O, Wilkinson J (2021) Exploring public engagement with missing person appeals on Twitter. Polic Soc 31(7):798–821
Stevenson E, Thomas SDM (2018) A 10 year follow-up study of young people reported missing to the police for the first time in 2005. J Youth Stud 21(10):1361–1375
Van Houtven CH, Konetzka RT, Taggert E, Coe NB (2020) Informal and formal home care for older adults with disabilities increased, 2004–16. Health Aff 39(8):1297–1301
Victor CR, Rippon I, Quinn C, Nelis SM, Martyr A, Hart N, Lamont R, Clare L (2021) The prevalence and predictors of loneliness in caregivers of people with dementia: findings from the IDEAL programme. Aging Ment Health 25(7):1232–1238
Wikipedia contributors (2022) Missing person. In Wikipedia, The Free Encyclopedia
Wong SYS, Zhang D, Sit RWS, Yip BHK, Chung RY-n, Wong CKM, Chan DCC, Sun W, Kwok KO, Mercer SW (2020) Impact of COVID-19 on loneliness, mental health, and health service utilisation: a prospective cohort study of older adults with multimorbidity in primary care. Br J Gen Pract 70(700):e817–e824
World Health Organization (2020) Decade of healthy ageing: plan of action. Available via https://www.who.int/publications/m/item/decade-of-healthy-ageing-plan-of-action. Accessed 28 Mar 2023
Xin Y, Cai T (2019) Child trafficking in China: Evidence from sentencing documents. Int J Popul Stud 4(2):1–10
Xiong G (2017) Analysis of the total number of lost elderly in China and regional distribution characteristics–Based on a random sample survey of rescue stations nationwide (in Chinese). Popul Dev 23(06):103–108
Zeng Y, Feng Q, Hesketh T, Christensen K, Vaupel JW (2017) Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet 389(10079):1619–1629
Acknowledgements
We would like to thank Toutiao for establishing the Toutiao Alert platform, which played a valuable role in finding some missing persons and from which we collected the data analyzed in the current study. This work was supported by the Scientific Research Start-up Foundation for Talent Plan of Harbin Institute of Technology (Grant No.: AUGA5710014023).
Author information
Authors and Affiliations
Contributions
All authors have contributed substantially to the article. YZ and ZZ designed the research. ZZ performed data collection and data cleaning. YZ performed data analysis and draft the manuscript. YZ and FZ reviewed and revised the manuscript. All authors have given their final approval to the version to be published. All authors have agreed to take responsibility for all aspects of the work to ensure that questions about the accuracy or integrity of any part of the work are properly investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was not required because the study was non-interventional and based on secondary, publicly available data from the Toutiao Alert platform. The study did not contain any studies with human participants performed by any of the authors.
Informed consent
The study was based on data that were publicly available on the Toutiao Alert platform. The study did not contain any studies with human participants performed by any of the authors. Therefore, informed consent from participants was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Z., Zhu, F. & Zhang, Y. Prevalence and patterns of mental and cognitive impairments among missing older adults in China. Humanit Soc Sci Commun 10, 793 (2023). https://doi.org/10.1057/s41599-023-02311-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-023-02311-8