Abstract
We report prevalence and risk factors for multimorbidity and multi-disability among elderly people in residential care in the Hyderabad region in South India. In total, 1182 elderly (aged ≥ 60) participants were examined in 41 homes for the aged centres. Detailed interviews were conducted by trained personnel to collect personal and demographic information. A questionnaire was used to assess the history of non-communicable diseases and Washington Disability Questionnaire (WDQ) was administered to assess disabilities. The mean age of the participants was 75.0 years (SD 8.8 years; range: 60–108 years), 35.4% were men, 20.3% had no formal education, 60.7% had school education and 19% had higher education. The prevalence of multimorbidity was 37.6% (95% CI: 34.8–40.4). Prevalence of multi-disability was 23.6% (95% CI: 21.2–26.3; n = 270). In total, 857 (72.5%) participants reported using at least one medication for NCDs. Over a third of the elderly in residential care had multimorbidity, and a quarter of them had multi-disability. A holistic health care system that comprises health and wellness coupled with rehabilitation to address disabilities is needed to achieve healthy aging in elderly in homes for the aged in India.
Similar content being viewed by others
Introduction
Aging is the hallmark of the twentieth century. An increase in the size of the elderly population has resulted in significant changes in the demographic profile in most countries. In India, individuals aged 60 years and older are considered elderly. From being less than 10% in 2010, the proportion of elderly in the population is expected to double by 20501,2. Also, the number of elderly individuals living separately from their children in the same or different locations, either alone or with their spouses, have gone up due to societal changes3,4. The rise in the number of homes for the aged, especially in urban and suburban areas in India, is another spinoff3.
Globally over a billion people are estimated to have disabilities5. Aging is often associated with a higher prevalence of non-communicable diseases (NCDs) and disabilities5,6. A high prevalence of hypertension, diabetes and heart diseases have been reported in the community-dwelling elderly population in South India and also in the general population in India7,8,9. The 2011 census in India revealed that 5.1% of the elderly had various kinds of disabilities10. A more recent population-based study from the state of Telangana reported that every fifth elderly had at least one disability and every third individual had at least one NCD11. Other community-based studies conducted in India have shown a high prevalence of disabilities and NCDs in the community-dwelling elderly population12,13,14,15. Also, a high prevalence of visual impairment has been reported in the elderly in South India16. A few studies have also highlighted the adverse effect that various kinds of disabilities have on the quality of life of the elderly and their wellbeing17. Multimorbidity, defined as two or more systemic health issues (NCDs) in an individual, is common among the elderly, with a prevalence ranging from 24% to as high as 83%18,19. The adverse effect of multimorbidity in the elderly has been widely reported. However, such data on elderly people in residential care (homes for the aged) is not available20,21,22,23,24.
The Hyderabad Ocular Morbidity in Elderly Study (HOMES) was carried out in homes for the aged centres located in and around Hyderabad in the South Indian state of Telangana25. It was aimed to broaden the understanding of the burden of vision loss, its causes and associated risk factors among the elderly in residential care25. The HOMES study reported that 30.1% of the elderly had vision impairment26. The evaluation of HOMES participants also included collecting detailed information on NCDs including, diabetes, hypertension, heart disease, muscle-skeletal disorders and other conditions. The information on disabilities was collected using the Washington Disability Questionnaire27,28. In this paper, we report on the prevalence and risk factors for multimorbidity and multi-disability in the elderly in residential care.
Methods
Ethics approval
The study protocol was approved by the Institutional Review Board of the Hyderabad Eye Research Foundation, L V Prasad Eye Institute, Hyderabad. Each participant provided written informed consent for their participation in the study. The study was carried out between 2017 and 2019 in accordance with the Declaration of Helsinki.
Sample selection
This study was nested in a study that aimed to understand the prevalence, causes and risk factors of visual impairment. Based on an anticipated prevalence of visual impairment of 15%, a precision of 20% prevalence (± 3%), a non-response rate of 25%, and a design effect of 1.4 to account for clustering, a sample size of 916 individuals was required. This sample is also sufficient for estimation of the prevalence of systemic conditions (NCDs) and disabilities as the prevalence of these conditions is higher than the prevalence of visual impairment.
Study population
The study included all the 46 homes that agreed to participate (including the five homes selected for the pilot study) from the 76 homes for the aged in the Hyderabad region in Telangana state. About a third of the homes did not consent to participate in the study. The main reasons stated for non-participation were, (a) preference to visit the eye care providers when needed and not to burden the elderly with regular eye examinations as part of the project and (b) no consent and/or non-approval from the family members of the elderly for participation in the study. In addition, six homes agreed to participate in the study, but space was not available for setting up the clinic for assessment.
Residents aged ≥ 60 years, who agreed to participate and were living in these homes for at least one month at the time of enumeration, were included. We have reported the description of these homes, participants' characteristics and the study protocol in our previous publications25,26,29. In brief, the homes were classified as (1) private homes where the individuals or their kin pay a monthly or annual user fee; (2) aided/partially subsidized homes where the individuals or their kin pay a part of the user fee, and the rest of the amount is met by philanthropic support or through other funding sources; (3) free homes where individuals need not pay any user fee as they are supported through external funding.
As described in our previous publications, all the participants underwent a detailed interview by trained investigators25. It involved recording their personal and socio-demographic information, ocular and systemic history (including information on diabetes, hypertension, heart disease and musculoskeletal issues), lifestyle factors such as smoking and alcohol consumption. For those participants who reported systemic condition/s, the duration of the diagnosis of the condition/s and current medication/s were asked and documented. Additionally, the details regarding the current medication/s taken by the residents (after seeing the supplies), their cost and the frequency of each medication/s were recorded. Multimorbidity is defined as reporting two or more NCDs in an individual. Polypharmacy was defined as the use of five or more medication daily30.
Study tools
The Washington Group (WG) developed a brief questionnaire [Washington Disability Questionnaire (WDQ)] to facilitate quick and comparable data collection on disabilities in population-based studies and the population census27,28. These are the most commonly used questionnaires to estimate the prevalence of disabilities. These WG questionnaires are used in over 100 national population censuses to date27. They are also recommended by United Nations and other agencies as indicators for Sustainable Development Goals (SDG) and United Nations Convention on the Rights of People with Disabilities. The WG questionnaires were also used in surveys in India (including the state of Telangana where the current study was conducted) and in other developing countries31.
The Washington Disability Questionnaire was used to assess disabilities in this study25. It was administered to the participants in their local language (Telugu or Hindi) before the eye examination, and included the following questions: (a) Do you have difficulty seeing, despite wearing glasses? (b) Do you have difficulty hearing, despite using a hearing aid? (c) Do you have difficulty walking or climbing steps? (d) Do you have difficulty remembering or concentrating? (e) Do you have difficulty (with self-care such as) cleaning yourself or dressing? (f) Using your usual (customary) language, do you have difficulty communicating, for example, understanding or being understood? Each of these questions had four options based on severity, such as (1) Not at all, (2) Some difficulty, (3) Lot of difficulties and (4) Cannot do at all. ‘Not at all’ and ‘Some difficulty’ were considered as no disability. ‘Lot of difficulties’ and ‘Cannot do at all’ were considered as a disability11 . Multi-disability is defined as reporting two or more disabilities in an individual.
Covariates
Independent variables included age group (60–69, 70–79 and ≥ 80 years), gender (male or female), education (higher education/graduation and above), school education only (1–12 years of education), or no education, marital status (married, widowed/separated, single), type of home (free, subsidized or private), smoking (never smokers and ever smokers, including current and past smoker) and alcohol consumption (no alcohol and ever alcohol, including current and past alcohol consumption).
Data management
Data analysis was conducted using Stata Statistical Software for Windows, version 14 (StataCorp, College Station, TX)32. Prevalence estimates were calculated and presented with 95% Confidence Intervals (CI). Logistic regression models were used to examine the strength of association between multimorbidity and the potential risk factors. In multiple logistic regression analysis, multimorbidity was used as an outcome variable and its association with other sociodemographic covariates (age, gender, level of education, marital status, type of home) was assessed. In the multivariable regression model, covariates were included based on published literature, and were entered into the model at a time. A similar analysis was also conducted for multi-disability. The Hosmer–Lemeshow goodness of fit test was used to assess the model fit. Variance Inflation Factors (VIF) were used to test collinearity between the covariates after fitting a multiple regression model. The adjusted odds ratios (OR) with 95% confidence intervals (CI) were presented. For all analyses, the statistical significance was assessed at the conventional level of p less than 0.05 (two-tailed). However, the exact p values were reported.
Results
Characteristics of the participants
Fifteen hundred and thirteen residents were enumerated from 41 homes, of which 1182 (78.1%) were interviewed and examined in the makeshift eye clinics set up in the homes. The demographic profile of the study participants is presented in our previous publications25,26,29. In short, 179 (11.8%) participants were not available for examination even after two attempts and 152 (10.1%) refused to undergo eye examinations. The mean age (p = 0.05) and gender (p = 0.31) distribution of the participants who were examined and non-examined were similar. The mean age of examined participants was 75.0 years (SD 8.8 years; range: 60–108 years), 35.4% (n = 418) were men, 20.3% (n = 240) had no formal education, 60.7% (n = 717) had school education and 19% (n = 225) had higher education. In all, 501 (42.4%) participants were living in paid/private homes, 419 (41.5%) were living in subsidised homes, and 190 (16.6%) were living in free homes. Data on Body Mass Index (BMI) was available for 929/1,182 (78.6%) participants, of which 463 (49.8%) were normal/underweight, 310 (33.4%) were overweight, and 156 (16.8%) were obese.
Multimorbidity
The prevalence of multimorbidity was 37.6% (95% CI: 34.8–40.4; n = 444). Overall, 836 (70.7%; 95% CI: 68.0–73.3) participants reported at least one NCD. The prevalence of multimorbidity stratified by personal and socio-demographic factors is shown in Table 1. Hypertension was the most common NCD (57.4%; 95% CI: 54.5–60.3; n = 678) followed by diabetes (28.0%; 95% CI: 25.4–30.6; n = 331), musculoskeletal pains (10.7%; 95% CI: 9.0–12.6; n = 127) and heart disease (9.9%; 95% CI: 8.2–11.7; n = 117) (Fig. 1).
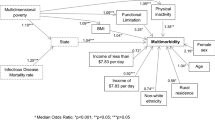
On simple logistic regression analysis, multimorbidity was associated with 70–79 years age group, type of residence, and BMI. On multiple logistic regression analysis, the multimorbidity was associated with older age groups. In comparison with those aged 60–69 years, the odds of having multimorbidity were higher for those aged 70–79 years (OR:1.37; 95% CI: 1.01–1.86) and 80 years and older age groups (OR: 1.13; 95% CI: 0.82–1.56). In comparison to those elderly who resided in ‘free’ homes, the odds for multimorbidity were higher for those residing in subsidised’ (OR: 1.73; 95% CI: 1.18–2.53) and ‘private homes’ (OR:1.79; 95% CI: 1.20–2.67). Compared to the elderly who had normal BMI, the odds for multimorbidity were higher among those who were overweight (OR: 1.86; 95% CI: 1.37–2.52) and obese (95% CI: 1.71; 95% CI: 1.16–2.51). Gender, level of education, smoking, and alcohol consumption were not associated with multi-morbidity. (Table 1).
Table 2 shows the stratification of numbers of NCDs among the participants (Table 2).
Multi-disability
Data on disabilities were available for 1,140/1,182 (96.4%) participants. The prevalence of multi-disability was 23.6% (95% CI: 21.2–26.3; n = 270). Half (50.0%) of the elderly residents had at least one disability (95% CI: 47.0–52.9; n = 570). In terms of the number of disabilities in an individual, 300 (26.3%) reported one disability, 153 (13.4%) reported two disabilities and 117 (10.3%) reported three or more disabilities. Mobility (38.1%; 95% CI: 35.2–41.0) was the most commonly reported disability followed by cognition (13.3%; 95% CI: 11.4–15.4), vision (12.8%; 95% CI: 10.9–14.9), hearing (11.8%; 95% CI: 10.0–13.9), self-care (9.6%; 95% CI: 7.9–11.5) and communication (6.0%; 95%: 4.7–7.5) (Fig. 2).
On simple logistic regression analysis, multi-disability was associated with older age groups, lower levels of education and higher BMI categories. On multiple logistic regression analysis, multi-disability was associated with 80 years and older age group (OR:2.50; 95% CI: 1.64–3.33). Those elderly who had no education had significantly higher odds (OR: 2.60; 95% CI: 1.31–5.15) for multi-disability compared to those who had higher education. Though odds for multi-disability were higher among those with school education, it was not statistically significant (p = 0.99). Multi-disability was associated with the type of home with individuals living in subsidised/aided homes having higher odds (OR:1.60; 95% CI: 1.06–2.57) compared to those living in paid homes. Gender, alcohol, and smoking status and BMI were not associated with multi-disability (Table 3).
Table 4 shows the stratification of number of disabilities in the study participants (Table 4).
Current medication and assistive devices usage
In total, 840/1,182 (71.1%) of the participants reported using at least one medication. Among these, 261 (31.3%) participants were on one medication, 386 (46.2%) were on 2–4 medications. Polypharmacy (5 or more medications) was reported by 88 (22.5%) participants. In terms of assistive devices being used, spectacles for vision (57.1%) were the most common devices, followed by devices for walking (29.7%), including 15 people who were using a wheelchair for mobility, and hearing aids (3.1%). One person reported using a hand magnifier for near work. Approximately 70% (n = 823) of the elderly were using at least one assistive device (69.6%; 95%CI: 66.9–72.2). Among those using assistive devices, 70.6% (n = 581) were using one device, 27.7% (n = 228) were using two devices, and only 1.7% (n = 14) were using three devices.
On multiple logistic regression analysis, the use of an assistive device was associated with older age with odds of 1.83 (95% CI:1.35–2.49) for those aged 70–79 years and 2.22 (95% CI: 1.60–3.09) for those aged 80 years and older. Those elderly who had higher levels of education were more likely to use an assistive device. Higher odds were also found for those with school education (OR:1.70; 95% CI:1.24–2.34) and higher education (OR:2.14; 95% CI:1.35–3.38) compared to those without any education. The use of assistive devices was not associated either with gender or type of home (Table 5).
Discussion
One out of every three elderly in residential care had multimorbidity, and a quarter of them had multi-disability. Over two-thirds of the elderly had at least one NCD, and half of them had at least one disability. Also, close to 73% of them were on at least one medication for their systemic health. Close to 70% of the elderly were using at least one assistive device, spectacles being the most commonly used device. Only 3% of the elderly were using hearing aids despite hearing impairment being one of the common disabilities. A large burden of NCDs and disabilities was also reported in a community-based sample of the elderly population in Telangana state using a similar protocol11.
Multimorbidity was associated with older age groups, similar to other studies in India and other regions33,34. The odds were higher among those living in subsidized (aided) and private homes than those staying in free homes. The prevalence of multimorbidity was recorded based on self-reporting. It is possible that those living in private and subsidised homes had better access to care or were more health conscious. Thus, they sought health care and were more aware of their health issues. And, with more resources at their disposal, they tended to live in subsidized and private homes.
Diabetes and hypertension are public health challenges in India and highly prevalent among elderly individuals in the community7,8,35,36. Both diabetes and hypertension are known to be associated with irreversible vision loss. Hence, they are of special interest to the eye care community. From the service delivery aspect, these conditions need continuity of care to ensure that they are in control and do not lead to complications and subsequent disabilities37,38,39.
In our study population, similar to the population-based studies, we found a high prevalence of mobility issues, vision loss and hearing impairment11. A population-based study using a similar examination protocol in the same state has reported that one-fifth of the elderly had at least one disability, and over a third of them had at least one NCD11. Some studies have reported a large regional variation in the burden of disabilities within the same states ranging from 23.4 to 53.6% in Uttar Pradesh 40,41 and from 20.6 to 68% in Tamil Nadu42. The study conducted in Tamil Nadu reported visual disability as more common compared to mobility42.
Two other studies, one in Odisha and one in Rajasthan, have reported the prevalence of cognitive impairment as 25% and 51%, respectively—much higher than what we found in our study in Telangana43,44. The variability reported in the burden is due to the varying methods adopted in these studies and the study participants. Moreover, the results from these community-based studies are not comparable with our study because of difference in lifestyle and other socio-demographic factors of the participants.
Disabilities were associated with older age with significantly higher odds among those aged 80 years and older. Interestingly, disability was not associated with gender and BMI. After adjusting for covariates, those with no education and residing in free homes had higher odds for disability. It is suggestive of their poor access and limited financial resources to seek care. Disability is often related to the inability of an individual to perform a particular task as perceived by an individual. On the other hand, NCDs such as hypertension and diabetes are often based on biological parameters and can result in disabilities as a complication. Those with higher levels of education were probably better at managing their systemic conditions resulting in lower odds of disabilities than those with no education. They were also more likely to use assistive devices.
Providing quality and holistic health care and rehabilitation are public health challenges. And in India, this challenge is expected to compound in future years with the demographic transition. But without the implementation of appropriate health policies—healthy and happy aging—cannot be achieved. The governments, especially in developing countries such as India, are developing socio-economic schemes and health welfare policies and programmes focusing on the elderly45.
The Government of India launched the National Programme for Health Care of the Elderly (NPHCE) in 2010 to create a health care framework for the elderly to provide accessible, affordable, and comprehensive health care17,46. It also includes financial support in terms of a monthly pension for the elderly. The National Health Policy of 2017 aims for universal and affordable health care for all. There is a need to study the impact of these initiatives and replicate them with a special focus on the elderly in residential care47. An integrated approach that includes physical and mental health, social services, lifestyle, and community institutions is recommended48.
In India, a few non-government organizations have been focussing on elderly health and wellness49. To ensure continuity of care, there is a need to make home-based care available to these vulnerable groups by using innovative approaches such as telehealth and other similar models. Also, there is a need for comprehensive elderly-centric health care covering all aspects of the elderly including, health and wellness, yoga and meditation for mental and physical wellbeing, rehabilitation, and assistive devices for disabilities. Novel home-based eye care initiatives for the elderly eye care are also being pilot tested in India. If found successful, these initiatives can be expanded to incorporate preliminary screening for NCDs and disabilities in the elderly with appropriate referrals and eye health could thus become an entry point for holistic health care for the elderly50.
We reported on multimorbidity and multi-disability among the elderly in residential care as a part of a larger eye health study for the first time in India. The study also assessed the use of assistive devices. Our results can also be generalized to the elderly in residential care in other urban areas in India. We used a questionnaire-based approach and self-report from the elderly and did not do the objective assessment of the health conditions. It could have resulted in a potential bias. Also, as we have used a cross-sectional study design, the association between the outcome and other variables cannot be firmly established. Despite these limitations, our study has provided valuable insights on disability and the systemic health situation of the elderly in residential care. The insights provide a good base for developing elderly centric services to contribute to healthy ageing in India.
Data availability
The datasets generated during the study are not publicly available as further data analysis is being carried out. The data can be made available from the corresponding author on a reasonable request.
References
UN. World Population Prospects 2017. (United Nations, Department of Economic and Social Affairs, Population Division, 2017).
UNPF. United Nations Population Fund—The State of World Population 2011. (2011).
Mane, A. B. Ageing in India: Some social challenges to elderly care. J. Gerontol. Geriatr. Res. 5, e136 (2016).
Yeolekar, M. E. Elderly in India–Needs and issues. J. Assoc. Phys. India 53, 843–844 (2005).
WHO. World Report of Disability 2011. (WHO, 2011).
WHO. Global Status Report on Noncommunicable Diseases 2014. (WHO, 2014).
Anchala, R. et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J. Hypertens. 32, 1170–1177. https://doi.org/10.1097/HJH.0000000000000146 (2014).
Geldsetzer, P. et al. Diabetes and hypertension in India: A nationally representative study of 1.3 million adults. JAMA Intern. Med. 178, 363–372. https://doi.org/10.1001/jamainternmed.2017.8094 (2018).
Gupta, R. & Gaur, K. Emerging trends in hypertension epidemiology in India. J. Hum. Hypertens. 33, 575–587. https://doi.org/10.1038/s41371-018-0117-3 (2019).
Velayutham, B., Kangusamy, B., Joshua, V. & Mehendale, S. The prevalence of disability in elderly in India—Analysis of 2011 census data. Disabil. Health J. 9, 584–592. https://doi.org/10.1016/j.dhjo.2016.04.003 (2016).
Marmamula, S., Modepalli, S. B., Kumbham, T. R., Challa, R. & Keeffe, J. E. Prevalence of disabilities and non-communicable diseases in an elderly population in the Telangana state, India: A population-based cross-sectional study. BMJ Open 11, e041755. https://doi.org/10.1136/bmjopen-2020-041755 (2021).
Gupta, P., Mani, K., Rai, S. K., Nongkynrih, B. & Gupta, S. K. Functional disability among elderly persons in a rural area of Haryana. Indian J. Public Health 58, 11 (2014).
Shah, B. & Prabhakar, A. K. Chronic morbidity profile among elderly. Indian J. Med. Res. 106, 265–272 (1997).
Srinivasan, K., Vaz, M. & Thomas, T. Prevalence of health related disability among community dwelling urban elderly from middle socioeconomic strata in Bangaluru, India. Indian J. Med. Res. 131, 515–521 (2010).
Lena, A., Ashok, K., Padma, M., Kamath, V. & Kamath, A. Health and social problems of the elderly: a cross-sectional study in Udupi taluk, Karnataka. Indian J. Commun. Med. 34, 131–134. https://doi.org/10.4103/0970-0218.51236 (2009).
Marmamula, S., Challa, R., Khanna, R. C., Kunkunu, E. & Rao, G. N. Population-based assessment of vision impairment in the elderly population in Telangana State in India—Policy implications for eye health programmes. Ophthalmic Epidemiol. 28, 144–151. https://doi.org/10.1080/09286586.2020.1797122 (2021).
Lahariya, C., Khandekar, J. & Pradhan, S. K. Effect of impairment and disability on health-related quality of life of elderly: A community-based study from urban India. Indian J. Commun. Med. 37, 223–226. https://doi.org/10.4103/0970-0218.103469 (2012).
Navickas, R., Petric, V. K., Feigl, A. B. & Seychell, M. Multimorbidity: What do we know? What should we do?. J. Comorb. 6, 4–11. https://doi.org/10.15256/joc.2016.6.72 (2016).
Salive, M. E. Multimorbidity in older adults. Epidemiol. Rev. 35, 75–83. https://doi.org/10.1093/epirev/mxs009 (2013).
Ara, S. Old-age homes & the profile of their residents. Indian J. Med. Res. 106, 409–412 (1997).
Liebig, P. S. Old-age homes and services: Old and new approaches to aged care. J. Aging Soc. Policy 15, 159–178. https://doi.org/10.1300/J031v15n02_10 (2003).
Varma, G. R., Kusuma, Y. S. & Babu, B. V. Health-related quality of life of elderly living in the rural community and homes for the elderly in a district of India. Application of the short form 36 (SF-36) health survey questionnaire. Z. Gerontol. Geriatr. 43, 259–263. https://doi.org/10.1007/s00391-009-0077-x (2010).
Pathania, A. et al. Prevalence of fall, and determinants of repeat incidents of fall in older persons living in old age homes in the National Capital Territory of Delhi, India. Natl. Med. J. India 31, 329–333. https://doi.org/10.4103/0970-258X.262912 (2018).
Samuel, R., McLachlan, C. S., Mahadevan, U. & Isaac, V. Cognitive impairment and reduced quality of life among old-age groups in Southern Urban India: Home-based community residents, free and paid old-age home residents. QJM 109, 653–659. https://doi.org/10.1093/qjmed/hcw040 (2016).
Marmamula, S. et al. Hyderabad Ocular Morbidity in Elderly Study (HOMES)—Rationale, study design and methodology. Ophthalmic Epidemiol. 27, 83–92. https://doi.org/10.1080/09286586.2019.1683867 (2020).
Marmamula, S. et al. Prevalence and risk factors for visual impairment among elderly residents in “homes for the aged” in India: The Hyderabad Ocular Morbidity in Elderly Study (HOMES). Br. J. Ophthalmol. https://doi.org/10.1136/bjophthalmol-2019-315678 (2020).
Groce, N. E. & Mont, D. Counting disability: Emerging consensus on the Washington Group questionnaire. Lancet Glob. Health 5, e649–e650. https://doi.org/10.1016/S2214-109X(17)30207-3 (2017).
Madans, J. H., Loeb, M. E. & Altman, B. M. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: The work of the Washington Group on Disability Statistics. BMC Public Health 11, S4. https://doi.org/10.1186/1471-2458-11-S4-S4 (2011).
Marmamula, S. et al. Uncorrected refractive errors for distance among the residents in “homes for the aged” in South India-The Hyderabad Ocular Morbidity in Elderly Study (HOMES). Ophthalmic Physiol. Opt. https://doi.org/10.1111/opo.12684 (2020).
Masnoon, N., Shakib, S., Kalisch-Ellett, L. & Caughey, G. E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 17, 230. https://doi.org/10.1186/s12877-017-0621-2 (2017).
Mactaggart, I. et al. Interrogating and reflecting on disability prevalence data collected using the Washington Group Tools: Results from population-based surveys in Cameroon, Guatemala, India, Maldives, Nepal, Turkey and Vanuatu. Int. J. Environ. Res. Public Health. https://doi.org/10.3390/ijerph18179213 (2021).
StataCorp. Stata Statistical Software: Release 14. (StataCorp LP, 2014).
Arokiasamy, P., Uttamacharya, & Jain, K. Multi-morbidity, functional limitations, and self-rated health among older adults in India: Cross-sectional analysis of LASI pilot survey, 2010. SAGE Open 5, 2158244015571640 (2015).
Marengoni, A. et al. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 10, 430–439. https://doi.org/10.1016/j.arr.2011.03.003 (2011).
Kapil, U. et al. Prevalence of hypertension, diabetes, and associated risk factors among geriatric population living in a high-altitude region of rural Uttarakhand, India. J. Fam. Med. Prim. Care 7, 1527–1536. https://doi.org/10.4103/jfmpc.jfmpc_108_18 (2018).
Unnikrishnan, R., Anjana, R. M. & Mohan, V. Diabetes mellitus and its complications in India. Nat. Rev. Endocrinol. 12, 357–370. https://doi.org/10.1038/nrendo.2016.53 (2016).
Zheng, Y., He, M. & Congdon, N. The worldwide epidemic of diabetic retinopathy. Indian J. Ophthalmol. 60, 428–431. https://doi.org/10.4103/0301-4738.100542 (2012).
Cheung, N., Mitchell, P. & Wong, T. Y. Diabetic retinopathy. Lancet 376, 124–136. https://doi.org/10.1016/S0140-6736(09)62124-3 (2010).
Fraser-Bell, S., Symes, R. & Vaze, A. Hypertensive eye disease: A review. Clin. Exp. Ophthalmol. 45, 45–53. https://doi.org/10.1111/ceo.12905 (2017).
Gupta, S., Yadav, R. & Malhotra, A. K. Assessment of physical disability using Barthel index among elderly of rural areas of district Jhansi (UP), India. J. Fam. Med. Prim. Care 5, 853 (2016).
Keshari, P. & Shankar, H. Prevalence and spectrum of functional disability of urban elderly subjects: A community-based study from Central India. J. Fam. Commun. Med. 24, 86 (2017).
Venkatarao, T., Ezhil, R., Jabbar, S. & Ramkrishnam, R. Prevalence of disability and handicaps in geriatric population in rural South India. Indian J. Public Health 49, 11 (2005).
Nayak, S., Mohapatra, M. K. & Panda, B. Prevalence of and factors contributing to anxiety, depression and cognitive disorders among urban elderly in Odisha—A study through the health systems’ Lens. Arch. Gerontol. Geriatr. 80, 38–45. https://doi.org/10.1016/j.archger.2018.09.008 (2019).
Patel, M., Bhardwaj, P., Nebhinani, N., Goel, A. D. & Patel, K. Prevalence of psychiatric disorders among older adults in Jodhpur and stakeholders perspective on responsive health system. J. Fam. Med. Prim. Care 9, 714–720. https://doi.org/10.4103/jfmpc.jfmpc_1016_19 (2020).
Verma, R. & Khanna, P. National program of health-care for the elderly in India: A hope for healthy ageing. Int. J. Prevent. Med. 4, 1103–1107 (2013).
Lahariya, C. “Ayushman Bharat” program and universal health coverage in India. Indian Pediatr. 55, 495–506 (2018).
Murthy, G. et al. Access to health care and employment status of people with disabilities in South India, the SIDE (South India Disability Evidence) study. BMC Public Health 14, 1125–1125. https://doi.org/10.1186/1471-2458-14-1125 (2014).
Bhan, N. et al. Health needs, access to healthcare, and perceptions of ageing in an urbanizing community in India: A qualitative study. BMC Geriatr. 17, 156. https://doi.org/10.1186/s12877-017-0544-y (2017).
Sawhney, M. The role of non-governmental organizations for the welfare of the elderly: The case of HelpAge India. J. Aging Soc. Policy 15, 179–191. https://doi.org/10.1300/J031v15n02_11 (2003).
Marmamula, S., Yanamala, N. K. & Khanna, R. C. “Eyecare on call”—Extending the frontiers of care through home-based eye care—Concept and the protocol. Indian J. Ophthalmol. 68, 2625–2627. https://doi.org/10.4103/ijo.IJO_2352_20 (2020).
Acknowledgements
The authors thank the individuals for their participation in the study. Rajesh Challa and Madhuri Bhakki are acknowledged for his assistance in data collection. Ms. Muni Rajya Lakshmi is acknowledged for her support with data management. Authors thank Ms. Neha Hassija for the language inputs on earlier versions of the manuscript.
Funding
This work was supported by DBT Wellcome Trust India Alliance Fellowship [IA/CPHE/14/1/501506] awarded to Dr. Srinivas Marmamula and Hyderabad Eye Research Foundation (HERF), India.
Author information
Authors and Affiliations
Contributions
S.M. conceived the idea, designed and conducted the study, analyzed the data and wrote the manuscript. T.R.K., S.B.M. and N.V.R. assisted in data collection, clinical quality control and supervised the field activities. R.Y. provided assistance in data management. R.S. and J.K. reviewed earlier versions of the manuscript and provided intellectual inputs. All authors have reviewed the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marmamula, S., Kumbham, T.R., Shidhaye, R. et al. Multimorbidity and multi-disability among the elderly in residential care in India: the Hyderabad Ocular Morbidity in Elderly Study (HOMES). Sci Rep 12, 11779 (2022). https://doi.org/10.1038/s41598-022-15943-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15943-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.