Abstract
CD36 may defect on platelets and/or monocytes in healthy individuals, which was defined as CD36 deficiency. However, we did not know the correlation between the molecular and protein levels completely. Here, we aim to determine the polymorphisms of the CD36 gene, RNA level, and CD36 on platelets and in plasma. The individuals were sequenced by Sanger sequencing. Bioinformational analysis was used by the HotMuSiC, CUPSAT, SAAFEC-SEQ, and FoldX. RNA analysis and CD36 protein detection were performed by qPCR, flow cytometry, and ELISA. In this study, we found c.1228_1239delATTGTGCCTATT (allele frequency = 0.0072) with the highest frequency among our cohort, and one mutation (c.1329_1354dupGATAGAAATGATCTTACTCAGTGTTG) was not present in the dbSNP database. 5 mutations located in the extracellular domain sequencing region with confirmation in deficient individuals, of which c.284T>C, c.512A>G, c.572C>T, and c.869T>C were found to have a deleterious impact on CD36 protein stability. Furthermore, the MFI of CD36 expression on platelets in the mutation-carry, deleterious-effect, and deficiency group was significantly lower than the no-mutation group (P < 0.0500). In addition, sCD36 levels in type II individuals were significantly lower compared with positive controls (P = 0.0060). Nevertheless, we found the presence of sCD36 in a type I individual. RNA analysis showed CD36 RNA levels in platelets of type II individuals were significantly lower than the positive individuals (P = 0.0065). However, no significant difference was observed in monocytes (P = 0.7500). We identified the most prevalent mutation (c.1228_1239delATTGTGCCTATT) among Kunming donors. Besides, our results suggested RNA level alterations could potentially underlie type II deficiency. Furthermore, sCD36 may hold promise for assessing immune reaction risk in CD36-deficient individuals, but more studies should be conducted to validate this hypothesis.
Similar content being viewed by others
Introduction
CD36, also known as glycoprotein IV (GPIV), is widely expressed on the surfaces of various cell types, including platelets, macrophages/monocytes, and adipocytes1. As a member of the class B scavenger receptor group, CD36 serves diverse physiological functions, encompassing lipid metabolism regulation2, involvement in thrombus formation on collagen3, and malaria-induced immune responses4. CD36 deficiency could occur in healthy individuals and has two subgroups: type I (defect on both platelets and monocytes) and type II (only defect on platelets)5,6. Individuals with CD36 deficiency, particularly type I, have an elevated risk of developing CD36 antibodies upon exposure to positive antigens through pregnancy, transfusion, or transplantation7,8,9,10. CD36 antibodies have a significant role in immune-mediated disorders, such as platelet transfusion refractoriness and fetal/neonatal alloimmune thrombocytopenia (FNAIT)9,11. Notably, CD36 antibodies are the primary pathogenic factor for FNAIT in China12. Intriguingly, recent literature demonstrates that CD36 conforms to the criteria for a new blood group, and anti-CD36 can also cause fetal anemia13, drawing more attention to focus on CD36.
The prevalence of CD36 deficiency varies significantly across regions, countries, and ethnic groups. Africans exhibit a higher incidence at 7.70%14, while Asians range from 1.68 to 8.20%15,16, and Caucasians have a lower prevalence at less than 0.40%17. Interestingly, there are notable regional and interethnic variations in CD36 deficiency within China. Southerners and ethnic minorities, such as the Man and Zhuang, have a frequent incidence of CD36 deficiency18,19. A previous study has demonstrated that 329–332 delAC is one of the most prevalent mutations in the Chinese population for CD36 deficient individuals, and the mutation is also frequently found in heterozygous form among CD36-positive individuals17.
CD36 is not only expressed on cells but also present in plasma, where it is referred to as soluble CD36 (sCD36)20. The sCD36 has displayed its potential as a plasma biomarker and has been linked to conditions such as atherosclerosis, metabolic syndrome, and malaria-infected erythrocytes. Alkhatatbeh et al.21,22 found that sCD36 is non-cleaved, non-soluble, and entirely associated with microparticles released from platelets and endothelial cells. More recently, a study by Phuangtham23 identified a significant correlation between CD36 on platelets and sCD36 in plasma, although the sample size was limited (N = 14). Intriguingly, this study did not find a substantial disparity in sCD36 levels between individuals with type II deficiency and those with a positive CD36 status.
In this study, our objective is to explore CD36 genetic polymorphism and assess genetic variations from DNA to protein levels (CD36 on platelets and in plasma). Additionally, we compare RNA level analysis between CD36-positive and CD36-negative individuals, combining to our previous study which reported seven cases of CD36 deficiency16.
Materials and methods
Sample preparation
Platelet donors were recruited from the Kunming Blood Center, following the inclusion criteria and specimen collection strategy outlined in our previous study16. A total of 418 platelet samples and 122 plasma samples were included in this study. All donors provided informed consent to participate in this study. The isolation of cells, DNA and RNA extraction, and cDNA preparation were carried out in accordance with established protocols as described in previous study.
Flow cytometry analysis
The flow cytometry method was described in us previous study16. Briefly, CD36 expression on the cells was determined using flow cytometry (FC500, Beckman Coulter). Platelets were obtained from platelet-rich plasma and incubated with phycoerythrin (PE)-labeled anti-CD41 antibodies (Biolegend, San Diego, CA, USA). Monocyte detection utilized 7-amino-actinomycin D (7-AAD, BD Pharmingen) and PE-conjugated anti-CD14 antibodies (M5E2, BD Pharmingen). CD36 expression was determined using fluorescein isothiocyanate (FITC)-conjugated anti-CD36 antibodies (CB38; BD Pharmingen, San Diego, CA, USA).
DNA analysis
The CD36 gene comprises 15 exons, but only exons 3 to 14 are involved in protein coding. In our research, we examined mutations located within these protein-coding exons in all CD36-positive individuals. The primers, reaction systems, and polymerase chain reaction (PCR) conditions were detailed in the previous publication16. The obtained results were analyzed using Chromas 2.5 and aligned with the reference sequence (Accession Number: NG_008192).
Prediction of the mutation causing amino acid substitution
To gain deeper insights into the impact of mutations involved in coding the extracellular domain, especially those not yet confirmed in deficiency cases, we employed HotMuSiC24, CUPSAT25, SAAFEC-SEQ26 and FoldX27 to assess the protein stability resulting from amino acid substitutions in individuals with missense mutations. Catalogizing the mutations which were predicted as destabilizing by three of these four tools, into the Predicted Group (PreGroup). Meanwhile, to validate the reliability of the predication tools, we also used the tools to predict the protein stability caused by 4 mutations (c.268C>T, c.410T>C, c.1156C>T and c.1163A>T), which has been known that could lead to CD36 deficiency.
RNA level analysis
We analyized RNA using qPCR (Bio-Rad CFX96, Berkeley, CA, USA) in CD36-positive individuals who had CD36 deficiency-related mutations and CD36-negative individuals previously identified. According to our prior study, exon 2–4 could be skipped, therefore, we designed detection primers located at exon 5 and its junction with exon 6 (forward primer: TGGTGCCATCTTCGAACCTT; reverse primer: GGATGCAGCTGCCACAG). We selected β-actin as the reference primer (forward primer: TGGCACCCAGCACAATGAA; reverse primer: CTAAGTCATAGTCCGCCTAGAAGCA). The qPCR analysis utilized the FastStart Universal SYBR Green Master (ROX) kit (Roche, Basel, CH). Each detection was performed twice, and the relative CD36 RNA levels were calculated using the ∆∆Ct method.
Detection of sCD36 in plasma
Plasma collection by centrifugation method with 3000g centrifugal force for 15 min, followed by removing the sediment and remaining the supernat. The obtained plasma was stored at – 80 °C. sCD36 was detected by Human platelet membrane glycoprotein IV, ELISA Kit (CUSABIO, Wuhan, CN), repeated twice for each sample.
Statistical analysis
Continuous values, including the mean fluorescence intensity (MFI) of CD36 on platelets, the concentration of sCD36 in plasma, and the comparative expression of CD36 RNA levels, were presented as mean ± standard deviation (M ± SD). Statistical analysis was conducted using GraphPad Prism 9 (GraphPad Software Inc., San Diego, CA, USA). Differences between two groups were assessed using an independent t-test, with statistical significance defined as a P value less than 0.0500, and multiple groups comparison using One-way Anova. Correlation analysis between CD36 on platelets and sCD36 in plasma was performed using the Simple Linear Regression method, and the results were recorded, including P values and the coefficient of determination (r-value).
Ethics approval and consent to participate
The study was approved by the ethics committee of the Institute of Blood Transfusion, Chinese Academy of Medical Sciences, and all methods were performed in accordance with the relevant guidelines and regulations.
Results
Polymorphisms analysis for CD36 protein-coding region
In our study, we included 418 platelet donors, among whom 7 individuals exhibited CD36 deficiency16. Exon 3–14 were investigated by Sanger sequencing among the CD36-positive individuals. The results showed that 15 heterozygous mutations were detected among 26 out of 411 CD36-positive platelet donors (Table 1; Fig. 1). 5 mutations (c.-18 insA, c.43A>C, c.1329_1354dupGATAGAAATGATCTTACTCAGTGTTG, c.1416_1420delAATAA, and c.1418_1420delAAG) were identified in the exons, which collectively cover the coding regions for the 5ʹ untranslated regions (UTR) and the cytoplasmic or transmembrane domains. Particularly, c.1329_1354dupGATAGAAATGATCTTACTCAGTGTTG, seems a new mutation and has not been described before. In addition, there were 9 single nucleotide polymorphisms (SNP) (c.268C>T, c.284T>C, c.410T>C, c.512A>G, c.572C>T, c.879T>C, c.869T>C, c.1156C>T, and c.1157G>A) and one deletion mutation (c.1228_1239delATTGTGCCTATT) located at extracellular topological domain coding sequence region.
We calculated the allele frequencies for the identified mutations and observed that c.1228_1239 delATTGTGCCTATT has the most frequent incidence in our cohort (allele frequency = 0.0072) (Table 1). Among these mutations found in CD36-positive individuals, only c.268C>T, c.410T>C, c.1156C>T, and c.1228_1239delATTGTGCCTATT have been confirmed in individuals with CD36 deficiency5,15,28,30. However, the effects of the rest of the mutations found in this study impacting on CD36 expression are uncertain, particularly those located in exon 4 to exon 13, which code for the extracellular domain and may impact the binding between the receptor and its ligand.
Prediction of substitution mutation on exon 4 to exon 13 responsible for extracellular domain coding.
To conduct an in-depth analysis of mutations (c.284T>C, c.512A>G, c.572C>T, c.869T>C, and c.1157G>A) located within the extracellular domain of the CD36 gene, we employed bioinformatic analysis through HotMuSiC, CUPSAT, SAAFEC-SEQ, and FoldX. We used the CD36-deficiency-related mutation to verify the efficiency of these 4 prediction tools (Table 2), and only HotMuSiC predicts c.1163A>T as a protein stabilizing mutation, suggesting the other 3 prediction models have a better analytical effect than HotMuSiC.
Given the classification criteria described in the method, we defined 4 of these mutations (c.284T>C, c.512A>G, c.572C>T, and c.869T>C) as a destabilizing mutation for protein, except for c.1157G>A with two tools display destabilizing mutation and two show stabilizing mutation (Table 3). Notably, a significant difference emerged between the MFI of these four individuals and the average MFI of all positive donors (P = 0.0400, 6.54 ± 3.84 vs 12.09 ± 5.47).
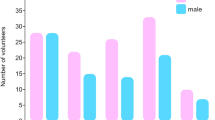
MFI analysis of platelets among wild-type, mutation carrier, predicted mutation, and deficient individuals
Following a comprehensive DNA analysis and bioinformatic prediction, we categorized the 8 individuals harboring CD36 deficiency-associated mutations (c.268C>T, c.410T>C, c.1156C>T, and c.1228_1239delATTGTGCCTATT) into the Carrier Group (CarGroup). In parallel, 4 individuals (c.284T>C, c.512A>G, c.572C>T, and c.869T>C) displaying a predicted deleterious stability, as determined by bioinformatics, were assigned to the Predicted Group (PreGroup). Additionally, we identified 6 individuals carrying mutations (c.43A>C, c.1329_1354dupGATAGAAATGATCTTACTCAGTGTTG, c.1416_1420delAATAA, and c.1418_1420delAAG) within the transmembrane and endodomain sequencing areas, and they were classified into the Unknown-Sense Group (USGroup). Notably, all subjects within these groups were CD36-positive individuals. In contrast, the Deficient Group (DefGroup) comprised 7 individuals16 with confirmed CD36 deficiency. Subsequently, comparing these groups with CD36-positive individuals who exhibited no mutations in Exon 3 to Exon 14 (PosGroup), respectively. The results are illustrated in Fig. 2. Specifically, the MFI of CD36 on platelets in CarGroup, PreGroup, and DefGroup was found to be significantly lower than that of PosGroup (P < 0.0500, 7.89 ± 1.68, 6.54 ± 3.84, 1.22 ± 0.30 vs. 12.09 ± 5.47 respectively), while there was no statistically significant difference observed between USGroup and PosGroup (P = 0.6365, 11.02 ± 4.98 vs. 12.09 ± 5.47).
Analysis of CD36 expression on platelet. PosGroup indicates positive individuals without any mutation on Exon 3 to Exon 14 (N = 390); CarGroup represents that individuals carry CD36 deficiency-related mutations (N = 8); PreGroup indicates the deleterious mutations predicated by PoPMuSiC (N = 4); USGroup and DefGroup respectively represent the individuals containing mutation on transmembrane and endodomain sequencing area (N = 6), and CD36 deficiency individuals (N = 7). “*” and “ns” were used to show statistical significance. “*” and “****” respectively denote P < 0.0500 and P < 0.0001, while ns mean no significant difference.
Analysis for sCD36 in plasma
We assembled a cohort of 122 plasma samples, which encompassed 7 CD36-deficient individuals (type I and type II) and 115 CD36-positive individuals. Our primary objective was to explore the correlation between CD36 expression on platelets and sCD36 in plasma. To accomplish this, we established a linear regression model employing the CD36-positive specimens. The results revealed statistically significant analysis, but indicated no correlation between sCD36 and CD36 expression on platelets (r = 0.31, P = 0.0007, N = 115) (Fig. 3A). Furthermore, we conducted a comparative analysis of sCD36 levels between CD36-positive and CD36-deficient individuals. It was evident that sCD36 levels among type II deficient individuals (N = 6) were notably lower than those of the positive controls (P = 0.0060, 48.36 ± 27.30 ng/ml vs. 76.39 ± 23.78 ng/ml) (Fig. 3B). Interestingly, one of the type II individuals was without mutations in the CD36 exons16, exhibited a higher sCD36 level in comparison to the 5 type II individuals harboring mutations [96.00 ng/ml vs. 38.83 ng/ml (mean value)] (Fig. 3B). In addition, sCD36 was also detected in the plasma of the type I individual (82.43 ng/ml).
Analysis for sCD36 in plasma. (A) Correlation analysis between sCD36 in plasma and CD36 on platelet (N = 116). Abscissa and vertical axis represent the CD36 expression on the platelet by flow cytometry (MFI) and sCD36 level in plasma (ng/ml), respectively; (B) sCD36 comparison between CD36 positive and deficient individuals. The hollow triangle indicated by the arrow in the Type II group represents the individual with type II phenotype, but no mutation was detected on the sequencing region. “**”represent P < 0.0100.
qPCR analysis
To analyze heterogeneity comprehensively, we employed the qPCR method to indirectly assess CD36 mRNA levels via cDNA detection. We selected a sample of 20 individuals, comprising 15 CD36-positive subjects (PosIn) and 5 individuals with type II CD36 deficiency (DefIn). Our initial focus was to compare CD36 mRNA levels derived from platelets among these three groups (Fig. 4A). The results demonstrated a significant difference, with CD36 mRNA in the DefIn group markedly lower in comparison to the PosIn group (P = 0.0065, 0.48 ± 0.22 vs. 2.22 ± 1.24). Additionally, we extended our analysis to compare CD36 mRNA levels in monocytes between the PosIn and DefIn groups, but no significant difference was observed (P = 0.7500, 2.05 ± 1.07 vs. 1.83 ± 0.98) (Fig. 4B).
mRNA level analysis for platelet and monocyte. Posln and Defln respectively represent individuals with CD36 expression and CD36 type II deficiency. (A) Analysis for CD36 cDNA extracted from platelet. “**” indicates P = 0.0065; (B) analysis for CD36 cDNA extracted from monocyte. “ns” indicates P = 0.7500.
Discussion
The CD36 gene comprises 15 exons, encompassing untranslated regions (exon1, 2, and 15) and protein-coding sequence (exon3 to 14). Most of mutations relevant to CD36 deficiency are location on protein-coding exons, while portions may be found on the alternative splicing regions16. Xu et al.17 found variations on 5ʹ UTR was supposed to lower the CD36 level, but there is no any report demonstrates the mutation on non-coding exons can cause CD36 deficiency. Therefore, in our study, we investigated protein-coding sequence polymorphisms in CD36 and identified 15 mutations. Significantly, one of these mutations, c.1329_1354dupGATAGAAATGATCTTACTCAGTGTTG, had not been previously documented in the dbSNP database. Noteworthy among the observed polymorphisms in CD36-positive subjects, only c.268C>T, c.410T>C, c.1156C>T, and c.1228_1239delATTGTGCCTATT displayed an inclination towards the manifestation of CD36 deficiency5,15,28,30. Moreover, our investigation revealed that in comparison to earlier studies17,31, c.1228_1239delATTGTGCCTATT is the most prevalent mutation. In contrast, mutations such as c.329_330delAC exhibited a notably lower allele frequency. Given our findings, particular attention should be devoted to the screening of c.1228_1239delATTGTGCCTATT, especially within the context of CD36 deficiency in the Kunming platelet donor population.
Moreover, the available evidence concerning other SNP, particularly those situated in the ectodomain coding region remains limited. We conducted a systematic assessment of these SNPs using the HotMuSiC, CUPSAT, SAAFEC-SEQ and FoldX tools. These 4 analysis tools are databases used to predict the effects of mutations on protein stability by integrating empirical energy functions, statistical potentials, atomic force data, and structural information, prioritizing mutations for experimental validation and optimizing protein stability for various applications24,25,26,27. In particular, FoldX is notably distinguished for its superior predictive capabilities in estimating the effects of mutations on protein stability27. The results of this study revealed a notable reduction in the stability of CD36. Remarkably, this prediction aligns with our observations from flow cytometry, which consistently showed a decrease in MFI (Table 2; Fig. 2). While this bioinformatic prediction provides valuable insights into the potential association between SNPs and CD36 deficiency, it is imperative to conduct confirmatory experiments at the cellular level to validate these findings.
CD36 deficiency manifests in two subgroups, type I and type II. The underlying mechanistic basis of type II deficiency remains largely elusive. A widely recognized theory put forward by Kashiwagi32 proposes the existence of a "platelet-specific silent allele". However, this hypothesis falls short in explaining type II deficiency in individuals lacking any detectable mutations. Our previous study successfully amplified the truncated CD36 transcript derived from platelets and we inclined that the alteration in RNA level may give us more clues to understand type II phenotype16. In this study, we applied qPCR to analyzed CD36 mRNA levels in both platelets and monocytes. As expected, qPCR results conclusively demonstrated that CD36 mRNA persists in platelets of type II individuals, albeit at a diminished level. Meanwhile, we also detected the CD36 mRNA levels in the type I deficient individual (ΔΔCt value: 0.45). However, we only screened one donor, and the sample size is insufficient to conduct a statistical analysis. When we integrate these findings with our previous work involving a non-mutation type II individual, we propose an optimized explanation of the "platelet-specific silent allele" theory. One of the alleles remains silenced, while the other continues to transcribe CD36 mRNA but undergoes alternative splicing as well as decrease of RNA level, a process potentially governed by enigmatic regulatory mechanisms.
In our comparative analysis of protein levels using MFI, we observed a significant reduction in CD36 protein expression in individuals harboring CD36 deficiency-associated mutations, consistent with previous research15,17. Notably, flow cytometry serves as the predominant technique for CD36 deficiency detection, albeit with relatively demanding sample and equipment requirements. To address these challenges, Phuangtham et al. proposed the utility of sCD36 as a potential biomarker for CD36-deficient individuals. Their study revealed the absence of detectable sCD36 in the plasma of type I deficient individuals and demonstrated a strong correlation between sCD36 levels in plasma and CD36 expression on platelets (r2 = 0.8551)23. In our study, we also incorporated sCD36 detection into our research. Intriguingly, our study did not find such a good correlation, and different sample size may be the main reason for this disparity. However, Peter Wilhelmsen et al.33 also demonstrated that there may be no correlation between CD36 on platelets and sCD36 in plasma. Besides, we also detected sCD36 in one individual exhibiting a type I phenotype, a departure from Phuangtham's findings. This variance can be attributed to genotype differences. Specifically, the type I individual in our study was in a heterozygous state (c.268 C>T) but with no CD36 protein expression on platelet and monocyte caused by only mutant transcript occurrence16, while wild-type CD36 mRNA may present in other cell types and sCD36 could be secreted. Moreover, speculative evidence from Kashiwagi suggests that type I deficient individuals with c.268C>T homozygosity fail to produce CD36 antibodies when exposed to positive antigens, possibly due to the limited presence of antigens on the cell surface28,34. Consequently, we hypothesize that the development of CD36 antibodies may not occur after exposure to positive antigens in the type I individual identified in our donor cohort. Conversely, Phuangtham et al.23 found no significant difference in sCD36 levels between type II and CD36-positive individuals, whereas our results revealed a contrary significance. These discrepant outcomes can also be attributed to different genotypic profiles. In our studies, type II individuals without mutations exhibited higher sCD36 levels compared to those harboring mutations. In Phuangtham's study, however, 4 out of 6 type II individuals without mutation, while only one individual among type II phenotypes displayed no mutations in our study. Furthermore, the majority of reported CD36 antibody-mediated severe diseases have been associated with type I individuals, with limited literature addressing type II phenotypes. In conclusion, we posit that sCD36 detection may offer advantages in assessing the risk of immune reactions in CD36-deficient individuals. Nonetheless, additional clinical trials and fundamental research are warranted to substantiate these findings.
In summary, this study investigates CD36 gene mutations associated with CD36 deficiency. We found 15 mutations, including a novel one (c.1329_1354dupGATAGAAATGATCTTACTCAGTGTTG). Four mutations (c.268C>T, c.410T>C, c.1156C>T, and c.1228_1239delATTGTGCCTATT) are linked to CD36 deficiency. Especially, the prevalence of c.1228_1239delATTGTGCCTATT, the most frequent genetic variant associated with CD36 deficiency. Therefore, special attention should be dedicated to this variant during screenings for CD36 deficiency. Bioinformatics analysis confirms reduced CD36 stability for specific mutations. The study also proposes an optimized interpretation of the "platelet-specific silent allele" theory for type II CD36 deficiency. Additionally, it suggests sCD36 as a potential biomarker for immune reactions in CD36-deficient individuals but calls for further research to validate these findings.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Greenberg, M. E. et al. Oxidized phosphatidylserine-CD36 interactions play an essential role in macrophage-dependent phagocytosis of apoptotic cells. J. Exp. Med. 203, 2613–2625. https://doi.org/10.1084/jem.20060370 (2006).
Li, Y. et al. CD36 favours fat sensing and transport to govern lipid metabolism. Prog. Lipid Res. 88, 101193. https://doi.org/10.1016/j.plipres.2022.101193 (2022).
Kuijpers, M. J. et al. Supporting roles of platelet thrombospondin-1 and CD36 in thrombus formation on collagen. Arterioscler. Thromb. Vasc. Biol. 34, 1187–1192. https://doi.org/10.1161/ATVBAHA.113.302917 (2014).
Thylur, R. P. et al. CD36 receptor regulates malaria-induced immune responses primarily at early blood stage infection contributing to parasitemia control and resistance to mortality. J. Biol. Chem. 292, 9394–9408. https://doi.org/10.1074/jbc.M117.781294 (2017).
Imai, M. et al. Genomic heterogeneity of type II CD36 deficiency. Clin. Chim. Acta 321, 97–106. https://doi.org/10.1016/s0009-8981(02)00102-x (2002).
Yanai, H. et al. Phenotype-genotype correlation in CD36 deficiency types I and II. Thromb. Haemost. 84, 436–441 (2000).
Xu, X. et al. Studies on CD36 deficiency in South China: Two cases demonstrating the clinical impact of anti-CD36 antibodies. Thromb. Haemost. 110, 1199–1206. https://doi.org/10.1160/TH13-05-0435 (2013).
Ogata, T. et al. CD36 (Naka) sensitization with platelet-transfusion refractoriness in a liver transplant recipient. Transplantation 79, 620. https://doi.org/10.1097/01.tp.0000146431.70743.89 (2005).
Ikeda, H. et al. A new platelet-specific antigen, Naka, involved in the refractoriness of HLA-matched platelet transfusion. Vox Sang 57, 213–217. https://doi.org/10.1111/j.1423-0410.1989.tb00826.x (1989).
Flesch, B. et al. Successful autologous hematopoietic progenitor cell transplantation in a patient with an isoantibody against CD36 (glycoprotein IV, Naka). Bone Marrow Transplant 42, 489–491. https://doi.org/10.1038/bmt.2008.190 (2008).
Xu, X. et al. Successful management of a hydropic fetus with severe anemia and thrombocytopenia caused by anti-CD36 antibody. Int. J. Hematol. 107, 251–256. https://doi.org/10.1007/s12185-017-2310-5 (2018).
Wu, G. et al. Platelet immunology in China: Research and clinical applications. Transfus. Med. Rev. 31, 118–125. https://doi.org/10.1016/j.tmrv.2016.12.001 (2017).
Alattar, A. G., Storry, J. R. & Olsson, M. L. Evidence that CD36 is expressed on red blood cells and constitutes a novel blood group system of clinical importance. Vox Sang https://doi.org/10.1111/vox.13595 (2024).
Lee, K. et al. CD36 deficiency is frequent and can cause platelet immunization in Africans. Transfusion 39, 873–879. https://doi.org/10.1046/j.1537-2995.1999.39080873.x (1999).
Masuda, Y. et al. Diverse CD36 expression among Japanese population: Defective CD36 mutations cause platelet and monocyte CD36 reductions in not only deficient but also normal phenotype subjects. Thromb. Res. 135, 951–957. https://doi.org/10.1016/j.thromres.2015.03.002 (2015).
Lyu, Q. et al. Frequency and molecular basis of CD36 deficiency among platelet donors in Kunming, China. Platelets 34, 2176168. https://doi.org/10.1080/09537104.2023.2176168 (2023).
Xu, X. et al. Variants of CD36 gene and their association with CD36 protein expression in platelets. Blood Transfus. 12, 557–564. https://doi.org/10.2450/2014.0209-13 (2014).
Liu, J. et al. Distribution of CD36 deficiency in different Chinese ethnic groups. Hum. Immunol. 81, 366–371. https://doi.org/10.1016/j.humimm.2020.05.004 (2020).
Ma, C. et al. A single-center investigational study of CD36 antigen deficiency and platelet alloantibody distribution in different populations in Northern China as well as platelet alloantibodies effect on pregnancy. Clin. Chim. Acta 498, 68–75. https://doi.org/10.1016/j.cca.2019.08.009 (2019).
Handberg, A., Levin, K., Hojlund, K. & Beck-Nielsen, H. Identification of the oxidized low-density lipoprotein scavenger receptor CD36 in plasma: A novel marker of insulin resistance. Circulation 114, 1169–1176. https://doi.org/10.1161/CIRCULATIONAHA.106.626135 (2006).
Alkhatatbeh, M. J., Mhaidat, N. M., Enjeti, A. K., Lincz, L. F. & Thorne, R. F. The putative diabetic plasma marker, soluble CD36, is non-cleaved, non-soluble and entirely associated with microparticles. J. Thromb. Haemost. 9, 844–851. https://doi.org/10.1111/j.1538-7836.2011.04220.x (2011).
Alkhatatbeh, M. J., Enjeti, A. K., Acharya, S., Thorne, R. F. & Lincz, L. F. The origin of circulating CD36 in type 2 diabetes. Nutr. Diabetes 3, e59. https://doi.org/10.1038/nutd.2013.1 (2013).
Phuangtham, R. et al. Frequency of CD36 deficiency in Thais analyzed by quantification of CD36 on cell surfaces and in plasma. Transfusion 60, 847–854. https://doi.org/10.1111/trf.15737 (2020).
Dehouck, Y., Kwasigroch, J. M., Gilis, D. & Rooman, M. PoPMuSiC 2.1: A web server for the estimation of protein stability changes upon mutation and sequence optimality. BMC Bioinform. 12, 151. https://doi.org/10.1186/1471-2105-12-151 (2011).
Parthiban, V., Gromiha, M. M. & Schomburg, D. CUPSAT: Prediction of protein stability upon point mutations. Nucleic Acids Res. 34, W239-242. https://doi.org/10.1093/nar/gkl190 (2006).
Li, G., Panday, S. K. & Alexov, E. SAAFEC-SEQ: A sequence-based method for predicting the effect of single point mutations on protein thermodynamic stability. Int. J. Mol. Sci. 22, 25. https://doi.org/10.3390/ijms22020606 (2021).
Buss, O., Rudat, J. & Ochsenreither, K. FoldX as protein engineering tool: Better than random based approaches?. Comput. Struct. Biotechnol. J. 16, 25–33. https://doi.org/10.1016/j.csbj.2018.01.002 (2018).
Kashiwagi, H. et al. Molecular basis of CD36 deficiency. Evidence that a 478C–>T substitution (proline90–>serine) in CD36 cDNA accounts for CD36 deficiency. J. Clin. Invest. 95, 1040–1046. https://doi.org/10.1172/JCI117749 (1995).
Kashiwagi, H. et al. Identification of molecular defects in a subject with type I CD36 deficiency. Blood 83, 3545–3552 (1994).
Okajima, S. et al. Two sibling cases of hydrops fetalis due to alloimmune anti-CD36 (Nak a) antibody. Thromb. Haemost. 95, 267–271. https://doi.org/10.1160/TH05-05-0378 (2006).
Li, R., Qiao, Z., Ling, B., Lu, P. & Zhu, Z. Incidence and molecular basis of CD36 deficiency in Shanghai population. Transfusion 55, 666–673. https://doi.org/10.1111/trf.12890 (2015).
Kashiwagi, H. et al. Family studies of type II CD36 deficient subjects: Linkage of a CD36 allele to a platelet-specific mRNA expression defect(s) causing type II CD36 deficiency. Thromb. Haemost. 74, 758–763 (1995).
Wilhelmsen, P. et al. Elevated platelet expression of CD36 may contribute to increased risk of thrombo-embolism in active inflammatory bowel disease. Arch. Physiol. Biochem. 119, 202–208. https://doi.org/10.3109/13813455.2013.808671 (2013).
Kashiwagi, H. et al. Analyses of genetic abnormalities in type I CD36 deficiency in Japan: Identification and cell biological characterization of two novel mutations that cause CD36 deficiency in man. Hum. Genet. 108, 459–466. https://doi.org/10.1007/s004390100525 (2001).
Acknowledgements
We like to thank Dr. Yin Yonghua for assistance on the data analysis.
Funding
This work was supported by the CAMS Innovation Fund for Medical Sciences (2021-1-I2M-060), Science and Technology Department of Sichuan Province (2020YFH0024), Kunming Health Science and Technology Talent Training Project (Grant/Award Number: 2020-SW -07), Yunnan Province young and middle-aged academic and technical leaders reserve talent project number (Grant/Award Number:202405AC350043) and Yunnan Provincial Hematology Clinical Research Center Project.
Author information
Authors and Affiliations
Contributions
L.Q. conducted and coordinated the study, analyzed data, and wrote the manuscript. L.Y. and P.Y. were responsible for experiment operation, data collection and analysis, and wrote the draft of this study, and they contributed equally to this work and shared the first authorship. G.X., J.X., P.M., L.Q., W.Z., and Z.Z. assisted with donor collection and sample treatment. L.Z., S.P., and W.J. contributed to the study design, data collection, and manuscript revision, and are the corresponding authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lyu, Q., Lin, Y., Pan, Y. et al. The polymorphism analysis for CD36 among platelet donors. Sci Rep 14, 8534 (2024). https://doi.org/10.1038/s41598-024-58491-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58491-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.