Abstract
The prognosis of patients with embolic stroke of undetermined source (ESUS) may vary according to the underlying cause. Therefore, we aimed to divide ESUS into subtypes and assess the long-term outcomes. Consecutive patients with acute ischemic stroke who underwent a comprehensive workup, including transesophageal echocardiography and prolonged electrocardiography monitoring, were enrolled. We classified ESUS into minor cardioembolic (CE) ESUS, arteriogenic ESUS, two or more causes ESUS, and no cause ESUS. Arteriogenic ESUS was sub-classified into complex aortic plaque (CAP) ESUS and non-stenotic (< 50%) relevant artery plaque (NAP) ESUS. A total of 775 patients were enrolled. During 1286 ± 748 days follow-up, 116 major adverse cardiovascular events (MACE) occurred (4.2 events/100 patient-years). Among the ESUS subtypes, CAP ESUS was associated with the highest MACE frequency (9.7/100 patient-years, p = 0.021). Cox regression analyses showed that CAP ESUS was associated with MACE (hazard ratio 2.466, 95% confidence interval 1.305–4.660) and any stroke recurrence (hazard ratio 2.470, 95% confidence interval, 1.108–5.508). The prognosis of ESUS varies according to the subtype, with CAP ESUS having the worst prognosis. Categorizing ESUS into subtypes could improve patient care and refine clinical trials.
Similar content being viewed by others
Introduction
Embolic stroke of undetermined source (ESUS) is defined as a non-lacunar ischemic stroke characterized by the absence of intracranial and extracranial arterial stenoses and major-risk cardioembolic (CE) sources1,2. Up to one-quarter of patients with ischemic stroke have ESUS. The associated stroke recurrence rate is approximately 4.5% per year and mortality rate is approximately 5.2% per year1,2,3,4,5.
Despite the poor outcomes of patients with ESUS, optimal secondary prevention strategies are not established. Given the undetermined embolic source, anticoagulant therapy is expected to be effective for secondary prevention in these patients. However, in two large randomized controlled trials, direct oral anticoagulants showed no benefit over aspirin in patients with ESUS6,7, possibly because of heterogeneity in the embolic source. Patient management can vary according to ESUS subtype. Patients with hidden atrial fibrillation might benefit from anticoagulant therapy, whereas those with < 50% stenosis in the carotid or cerebral arteries and complex aortic plaque (CAP) might benefit from antiplatelet therapy8,9. Therefore, predicting the outcome according to the ESUS subtype is important.
To the best of our knowledge, the prognosis according to ESUS subtype has not been fully investigated, especially in patients who have undergone a comprehensive workup including transesophageal echocardiography (TEE)10. This study aimed to reveal the long-term outcomes of patients with ESUS according to the subtype.
Results
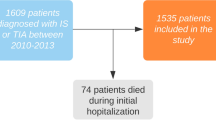
During the study period, 5443 patients with ischemic stroke were registered. Of these, 54 patients who did not undergo continuous ECG monitoring and 3373 patients who did not undergo TEE were excluded. Additionally, 1241 patients with conditions other than ESUS according to the TOAST classification were excluded (517 patients with large-artery atherosclerosis, 308 with cardioembolism, 157 with lacunar infarction, 94 with stroke of other determined etiology, and 165 with stroke of undetermined etiology with two or more causes identified). Finally, 775 (38%) patients were classified as having ESUS, with 161 patients of arteriogenic ESUS (20.8%), 205 patients of minor CE ESUS (26.5%), 184 patients of two or more causes ESUS (23.7%), and 225 patients of no cause ESUS (29.0%). Arteriogenic ESUS was further classified into CAP (70 patients, 9.0%) and NAP (91 patients, 11.7%) ESUS (Fig. 1). Two or more causes ESUS included arteriogenic (CAP and NAP) and minor CE ESUS. The patients with NAP and minor CE causes were 116 (15.0%), CAP and minor CE causes were 43 (5.5%), and CAP, NAP and Minor CE causes were 25 (3.2%) (Supplemental Table 1).
Inclusion and exclusion criteria and ESUS subtypes. Flowchart showing the inclusion and exclusion criteria. Patients who did not undergo transesophageal echocardiography or continuous electrocardiography (ECG) monitoring and those with a stroke other than ESUS were excluded. ESUS embolic stroke of undetermined source, LAA large-artery atherosclerosis, CE cardioembolism, LAC lacunar, SOD stroke of other determined etiology, UT stroke of undetermined etiology with two or more identified causes.
Baseline characteristics
The mean age was 63.3 ± 13.3 years, and 63% were men. The mean NIHSS score was 2.9 ± 3.6. Among all the groups, the patients with CAP ESUS were the oldest (70.0 ± 10.1 years), and hypertension (85.7%) and diabetes (38.5%) were most frequently observed in the patients with NAP ESUS. Patients with two or more causes ESUS had the highest prevalence of congestive heart failure (4.3%), coronary artery occlusive disease (47.8%), and peripheral artery occlusive disease (9.8%) compared to other subtypes. In pre-stroke medications, antiplatelet alone was most frequently used in patients with CAP (p < 0.001). Laboratory test results showed no significant differences between the ESUS subtypes. After index stroke, the secondary prevention was conducted using the antiplatelet (99.7%), anticoagulant (1.2%), and statin (98.8%) (Table 1).
Prognosis of patients with ESUS
The rates of poor outcomes at 3 months were similar across ESUS subtypes (20.0% for CAP ESUS, 25.3% for NAP ESUS, 16.6% for minor CE ESUS, 14.1% for two or more causes ESUS, and 17.3% for no cause ESUS). Long-term follow-up over 2913 person-years was conducted, with a median of 3.50 years (IQR 2.32–5.25 years). MACEs were observed in 116 patients (4.2/100 patient-years), any stroke recurrence in 69 (2.6/100 patient-years), ischemic stroke recurrence in 54 (2.0/100 patient-years), hemorrhagic stroke in 15 (0.5/100 patient-years), and all-cause mortality in 46 (1.6/100 patient-years). MACE occurred more frequently in patients with CAP ESUS (9.7/100 patient-years) than in those with other ESUS subtypes (NAP ESUS: 4.9/100 patient-years, two or more causes ESUS: 4.3/100 patient-years, no cause ESUS: 4.0/100 patient-years, and minor CE ESUS: 2.8/100 patient-years; p = 0.021; Table 2).
Univariable and multivariable analyses of outcomes according to ESUS subtype
Kaplan–Meier survival analysis revealed that MACE (p = 0.004) and any stroke recurrence rates (p = 0.032) differed according to ESUS subtype. Patients with CAP ESUS showed the highest MACE and any stroke recurrence rates. However, the ischemic stroke recurrence (p = 0.175) and all-cause mortality (p = 0.058) rates were similar across subtypes (Fig. 2).
Long-term outcomes during follow-up. Kaplan–Meier survival curves of MACE (A), any stroke recurrence (B), ischemic stroke recurrence (C), and all-cause mortality (D). Patients with complex aortic plaques show the highest rates of MACE and any stroke recurrence. However, ischemic stroke recurrence (p = 0.175) and all-cause mortality (p = 0.058) rates were similar across subtypes. MACE major adverse cardiovascular event, CE cardioembolism, NAP non-stenotic (< 50%) relevant artery plaque.
Univariable analysis revealed that CAP ESUS was associated with MACE along with age, sex, hypertension, diabetes, previous stroke history and platelet count. Multivariable Cox regression analysis revealed that CAP ESUS was independently associated with MACE (HR 2.466, 95% CI 1.305–4.660; Table 3) and any stroke recurrence (HR 2.470, 95% CI 1.108–5.508; Table 4). However, no significant associations were found between CAP ESUS and ischemic stroke recurrence, hemorrhagic stroke, and all-cause mortality (Supplemental Tables 2–4).s
Predictive value of the ESUS subtype classification for classical risk factors
When comparing the predictive value of the ESUS subtype classification and classical risk factors, the p-value of integrated discrimination index (IDI) of median follow up was 0.016 which was statistically significant. Additionally, the overall p-values are less than 0.2, indicating a tendency for differences between the two models (Supplemental Table 5).
Discussion
In this study, we categorized ESUS into subtypes and found that the prognosis differed among the subtypes. The worst long-term outcomes were observed in patients with CAP ESUS, whereas the best outcomes were observed in patients with minor CE ESUS. After adjusting for covariates, CAP ESUS was independently associated with MACE and any stroke recurrence.
We found that the prognosis of ESUS differed according to the ESUS subtype. Although no differences were observed in the short-term functional outcome at 3 months, the long-term outcomes were significantly different among the ESUS subtypes. MACE occurred most frequently in patients with CAP ESUS, whereas favorable long-term outcomes were most noted in patients with minor CE ESUS. Patients with CAP ESUS experienced three times more MACE during the follow-up period than those with minor CE ESUS.
Secondary prevention of ESUS is not well established. Direct oral anticoagulants have been failed to show significant benefits6,7. These results may be due to heterogeneity in ESUS subgroups. Studies including all ESUS subtypes may have attenuated the effects of the study drugs8,9. Treatments targeting hidden paroxysmal atrial fibrillation might differ from those targeting other embolic sources, including minor CE sources, < 50% stenosis in the cerebral arteries, and CAP. Some patients with a patent foramen ovale may benefit from closure. If the primary embolic sources are white thrombi forming on the aortic plaque or cerebral arteries, prevention with antiplatelet and statin might be beneficial11. To date, no detailed research has been conducted on the prognosis according to ESUS subtype. For patient management and clinical trial design, it is crucial to identify the ESUS subtype and determine the prognosis accordingly.
An exploratory analysis revealed that 8% of the participants of the NAVIGATE ESUS trial had CAP ESUS, with an ischemic stroke recurrence rate of 7.2/100 patient-years12. The ischemic stroke recurrence rate in our study (4.6/100 patient-years) was lower than that in the NAVIGATE ESUS trial, possibly due to different treatment strategy. In our study, all patients with CAP ESUS received antiplatelet therapy, and 97.1% received statin. The Aortic Arch Related Cerebral Hazard (ARCH) Trial investigated the superiority of aspirin plus clopidogrel over warfarin. The ARCH trial failed the difference between treatments. Recurrent stroke or vascular events occurred in 7.6% of patients on aspirin plus clopidogrel and 11.3% of patients on warfarin during a median follow-up 3.4 years13. Until now, the advantages of these two treatments are still unclear. However, current guidelines recommend antiplatelet therapy and intensive lipid-lowering to prevent recurrent stroke in patients with aortic arch atheroma14. Because our study was not a clinical trial and did not intend to test the effects of drugs, we cannot provide the optimal management of aortic atheroma.
Our findings and those of previous studies suggest several hypotheses for the poor prognosis of patients with CAP ESUS. First, the prevalence of CAP ESUS increases with age12, and patients with CAP have many risk factors15, which might influence the long-term outcomes. Second, CAP has been found to be associated with intracranial atherosclerosis and small vessel disease15,16, suggesting that it is a marker of systemic atherosclerosis15. Polyvascular disease is associated with poor prognosis in patients with ischemic stroke. Third, CAP may be accompanied by atrial fibrillation17,18, and the burden of additional embolic sources may result in a poor prognosis17. Therefore, evaluation by TEE to detect CAP in ESUS patients might be helpful in tailoring treatment of ESUS.
This study has several limitations. First, although we included consecutive patients with ESUS, we excluded those who did not undergo a comprehensive workup including TEE and continuous ECG monitoring. ESUS working group investigators recommended a comprehensive stroke workup, but TEE and continuous ECG monitoring were not included as mandatory investigations4. In more than half of cases, TEE examination can uncover embolic sources from heart or aorta that can significantly impact the prognosis of patients with ESUS19. Second, the effects of clinical characteristics of the ESUS subtypes, such as infarction patterns, vascular territory, and clinical symptoms, were not investigated20,21. Since the main purpose of this study was to compare the prognosis according to ESUS subtype, further investigations are needed to evaluate the clinical characteristics of each ESUS subtype. Third, the response to antithrombotic therapy for each ESUS subtype could not be determined in our study because most patients were treated with antiplatelet therapy and lipid-lowering agents.
Conclusions
We found that prognosis differed according to ESUS subtype. The long-term outcomes of MACE and any stroke recurrence were the worst in patients with CAP ESUS and the best in those with minor CE ESUS. Sub-classifying ESUS and predicting outcomes based on subtypes may improve patient management and clinical trial design.
Methods
Study population
Consecutive patients with acute ischemic stroke who were prospectively registered in the Yonsei Stroke Registry22 between January 2012 and December 2018 were enrolled. All patients underwent brain magnetic resonance imaging (MRI) and/or computed tomography (CT). Cerebral vessels were evaluated using cerebral angiography (MRI, CT, or digital subtraction angiography). Systemic evaluations included chest radiography, 12-lead electrocardiography (ECG), routine blood tests, and lipid profiling. Cardiac CT were performed in selected patients. To accurately classify ESUS subtypes, we only enrolled patients who had undergone continuous ECG monitoring and TEE. Most patients were admitted to the stroke unit and were continuously monitored with ECG during their stay. Continuous ECG monitoring was also obtained by Holter monitoring and an implantable loop recorder. TEE was part of the standard evaluation but was not performed in patients with a poor general condition, mental decline, impending brain herniation, or an unacceptable esophageal transducer due to swallowing difficulties or tracheal intubation, and in those who did not provide informed consent (Supplemental Table 6)23.
ESUS was defined based on the criteria proposed by the Cryptogenic Stroke/ESUS International Working Group4. A diagnosis of ESUS was made if the patient exhibited non-lacunar stroke, had no more than 50% stenosis of the relevant proximal artery, and presented with no significant CE source. These sources include atrial fibrillation, atrial flutter, sick sinus syndrome, mechanical or bioprosthetic heart valves, mitral stenosis (with or without atrial fibrillation), left atrial or atrial appendage thrombosis, left ventricular thrombus, akinetic left ventricular segment, recent myocardial infarction (occurring less than 4 weeks ago), dilated cardiomyopathy, atrial myxoma, infective endocarditis, and nonbacterial thrombotic endocarditis. Furthermore, patients with ESUS should not have other rare stroke causes such as reversible cerebral artery vasoconstriction syndrome, antiphospholipid syndrome, dissection, moyamoya disease, or cancer related stroke.
According to its potential cause, we classified ESUS into arteriogenic ESUS, minor CE ESUS, two or more causes ESUS, and no cause ESUS. Arteriogenic ESUS was sub-classified into CAP ESUS and non-stenotic (< 50%) relevant artery plaque (NAP) ESUS24,25. Minor CE sources included patent foramen ovale, atrial septal defect, atrial septal aneurysm, congestive heart failure, mitral valve prolapse, mitral annular calcification, left atrial turbulence (smoke), hypokinesia of the left ventricular segment, and myocardial infarction (> 4 weeks but < 6 months)4,26,27,28. CAP was defined by the presence of a plaque in the ascending aorta or aortic arch, which is either 4 mm or more in thickness or contains ulcerated or mobile components (Supplemental Table 1)29,30. The Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification was determined during weekly conferences through the consensus of three stroke neurologists28,31.
Clinical variables
We recorded the following clinical data of each participant: demographic characteristics (age and sex), risk factors (hypertension, diabetes, hypercholesterolemia, current smoking, coronary artery occlusive disease, peripheral artery occlusive disease, and previous stroke status), the initial National Institutes of Health Stroke Scale (NIHSS) score, and laboratory findings (white blood cell count, platelet count, total cholesterol level, triglyceride level, high-density lipoprotein cholesterol level, and low-density lipoprotein cholesterol level). Detailed information is available in a previous publication31.
Follow-up and outcomes
Neurologists and clinical research assistants collected the follow-up information at the outpatient clinic and/or by telephone interview using a structured questionnaire at 3 months, 1 year, and annually thereafter. The mRS score was determined by a structured interview using the Korean version of the mRS (http://stroke-edu.or.kr). A poor outcome at the 3-month follow-up was defined as a modified Rankin scale (mRS) score ≥ 3. Stroke recurrence was defined as a new stroke event occurring > 7 days after the index stroke. Major adverse cardiovascular event (MACE) included ischemic stroke recurrence, hemorrhagic stroke, acute coronary syndrome, heart failure, and all-cause mortality. The censoring date was December 31, 2019. If a patient’s last visit occurred before this date, the date of the last visit was considered the censoring date.
The study was approved by the relevant institutional review board of Severance Hospital of Yonsei University Health System, and the requirement for informed consent was waived because of the retrospective nature of the study (4-2021-1724). The original prospective hospital-based observational study was approved by the institutional review board (4-2007-0389) and informed consent was obtained from the patients or legal representatives. The study was performed in accordance with the World Medical Association Declaration of Helsinki.
Statistical analyses
Differences between ESUS subtypes were assessed using the chi-square test for categorical variables and independent two-sample t-test or Mann–Whitney U-test for continuous variables. Continuous variables are presented as either the mean with standard deviation or median with interquartile range (IQR). Categorical variables are presented as counts with percentages (%). Kaplan–Meier curves were constructed and the differences across ESUS subtypes were analyzed using the log-rank test. The results were evaluated by considering both statistical and clinical aspects using effect size (mean, proportion, HR), 95% CI and p-value. We assessed how the addition of the ESUS subtype variable to classical risk factors impacts the predictive accuracy of the Cox hazard model for outcomes. We compared the model of classical risk factors alone with model of novel. We calculated Harrell's c-index, Heagerty's area under the curve (AUC), the net reclassification index (NRI), and the integrated discrimination improvement (IDI). Statistical analyses were performed using SPSS for Windows, version 26 (IBM Corp., Armonk, NY, USA), R version 4.3.2 (R Foundation for Statistical Computing, Vienna, Austria) and MedCalc Statistical Software, version 20.026 (MedCalc Software Ltd., Ostend, Belgium; https://www.medcalc.org).
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Ntaios, G. et al. Embolic strokes of undetermined source in the Athens Stroke Registry: A descriptive analysis. Stroke 46, 176–181 (2015).
Hart, R. G., Catanese, L., Perera, K. S., Ntaios, G. & Connolly, S. J. Embolic stroke of undetermined source: A systematic review and clinical update. Stroke 48, 867–872 (2017).
Ntaios, G. et al. Potential embolic sources and outcomes in embolic stroke of undetermined source in the NAVIGATE-ESUS trial. Stroke 51, 1797–1804 (2020).
Hart, R. G. et al. Embolic strokes of undetermined source: The case for a new clinical construct. Lancet Neurol. 13, 429–438 (2014).
Ntaios, G. et al. Risk stratification for recurrence and mortality in embolic stroke of undetermined source. Stroke 47, 2278–2285 (2016).
Hart, R. G. et al. Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N. Engl. J. Med. 378, 2191–2201 (2018).
Diener, H.-C. et al. Dabigatran for prevention of stroke after embolic stroke of undetermined source. N. Engl. J. Med. 380, 1906–1917 (2019).
Tsivgoulis, G. et al. Embolic strokes of undetermined source: theoretical construct or useful clinical tool?. Ther. Adv. Neurol. Disord. 12, 1756286419851381 (2019).
Kamel, H. et al. The atrial cardiopathy and antithrombotic drugs In prevention after cryptogenic stroke randomized trial: Rationale and methods. Int. J. Stroke 14, 207–214 (2019).
Ueno, Y. et al. Large aortic arch plaques correlate with CHADS(2) and CHA(2)DS(2)-VASc scores in cryptogenic stroke. Atherosclerosis 284, 181–186 (2019).
Viedma-Guiard, E., Guidoux, C., Amarenco, P. & Meseguer, E. Aortic sources of embolism. Front. Neurol. 11, 606663 (2020).
Ntaios, G. et al. Aortic arch atherosclerosis in patients with embolic stroke of undetermined source: An exploratory analysis of the NAVIGATE ESUS trial. Stroke 50, 3184–3190 (2019).
Amarenco, P. et al. Clopidogrel plus aspirin versus warfarin in patients with stroke and aortic arch plaques. Stroke 45, 1248–1257 (2014).
Kleindorfer, D. O. et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke 52, e364–e467 (2021).
Chatzikonstantinou, A., Ebert, A. D., Schoenberg, S. O., Hennerici, M. & Henzler, T. Atherosclerosis in intracranial, extracranial, and coronary arteries with aortic plaques in patients with ischemic stroke of undetermined etiology. Int. J. Neurosci. 125, 663–670 (2015).
Chatzikonstantinou, A. et al. Coexisting large and small vessel disease in patients with ischemic stroke of undetermined cause. Eur. Neurol. 68, 162–165 (2012).
Suzuki, M. et al. Complex aortic arch atherosclerosis in acute ischemic stroke patients with non-valvular atrial fibrillation. J. Atheroscler. Thromb. 28, 776–785 (2021).
Blackshear, J. L. et al. Aortic plaque in atrial fibrillation: Prevalence, predictors, and thromboembolic implications. Stroke 30, 834–840 (1999).
Katsanos, A. H. et al. The value of transesophageal echocardiography for embolic strokes of undetermined source. Neurology 87, 988–995 (2016).
Kashima, S., Shimizu, T., Akiyama, H. & Hasegawa, Y. Magnetic resonance imaging white matter hyperintensity as a predictor of stroke recurrence in patients with embolic stroke of undetermined source. J. Stroke Cerebrovasc. Dis. 27, 3613–3620 (2018).
Shang, Z. Y. et al. The characteristics of intracranial plaques of unilateral, anterior circulation embolic stroke of undetermined source: An analysis of different subtypes based on high-resolution imaging. Eur. J. Neurol. 29, 2654–2663 (2022).
Lee, B. I., Nam, H. S., Heo, J. H. & Kim, D. I. Yonsei Stroke Registry. Analysis of 1,000 patients with acute cerebral infarctions. Cerebrovasc. Dis. 12, 145–151 (2001).
Nam, H. S. et al. Long-term mortality in patients with stroke of undetermined etiology. Stroke 43, 2948–2956 (2012).
Amarenco, P. et al. Atherosclerotic disease of the aortic arch and the risk of ischemic stroke. N. Engl. J. Med. 331, 1474–1479 (1994).
Tao, L. et al. Intracranial atherosclerotic plaque as a potential cause of embolic stroke of undetermined source. J. Am. Coll. Cardiol. 77, 680–691 (2021).
Hart, R. G. et al. Rivaroxaban for secondary stroke prevention in patients with embolic strokes of undetermined source: Design of the NAVIGATE ESUS randomized trial. Eur. Stroke. J. 1, 146–154 (2016).
Diener, H. C. et al. Design of randomized, double-blind, evaluation in secondary stroke prevention comparing the efficacy and safety of the oral thrombin inhibitor dabigatran etexilate vs. acetylsalicylic acid in patients with embolic stroke of undetermined source (RE-SPECT ESUS). Int. J. Stroke. 10, 1309–1312 (2015).
Adams, H. P. et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24, 35–41 (1993).
Nam, H. S. et al. Association of aortic plaque with intracranial atherosclerosis in patients with stroke. Neurology 67, 1184–1188 (2006).
Song, T.-J. et al. Association between aortic atheroma and cerebral small vessel disease in patients with ischemic stroke. J. Stroke 18, 312–320 (2016).
Lee, H., Heo, J., Lee, I. H., Kim, Y. D. & Nam, H. S. Association between blood viscosity and early neurological deterioration in lacunar infarction. Front. Neurol. 13, 979073 (2022).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2022R1A2C1007948).
Author information
Authors and Affiliations
Contributions
I.H.L., J.K. & H.S.N. designed research; I.H.L., J.H., H.L., J.J., J.K., M.H., J.Y., J. K., M.B., H.P., J.W.J., Y.D.K. & H.S.N. collected data; I.H.L., J.K., J.W.J., Y.D.K. & H.S.N. interpreted the data; I.H.L. & H.S.N. analyzed data and wrote the manuscript with contributions from J.H., H.L., J.J., J.K., M.H., J.Y., J. K., M.B., H.P., J.W.J. & Y.D.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, I.H., Heo, J., Lee, H. et al. Long-term outcomes of patients with embolic stroke of undetermined source according to subtype. Sci Rep 14, 9295 (2024). https://doi.org/10.1038/s41598-024-58292-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58292-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.