Abstract
To assess the long-term association between the residual renal volume and the progression of chronic kidney disease (CKD) in kidney donors following open or laparoscopic donor nephrectomy. A retrospective observational study involving 452 individuals who underwent open or laparoscopic donor nephrectomy at Ramathibodi Hospital, Bangkok, Thailand. The study spanned over a comprehensive 60-month monitoring period. Residual renal volume was determined through Computer Tomography. Patient characteristics, surgical techniques, donated kidney side, and estimated glomerular filtration rate (eGFR) were collected and analysed. In a multivariate analysis, a residual renal volume exceeding 50% of original volume is associated with an increased likelihood of developing CKD, with a hazard ratio (HR) of 1.675 (P < 0.05), and male gender has a hazard ratio (HR) of 4.013 (P < 0.001). Additionally, age is identified as a minor risk factor for developing CKD, with hazard ratio (HR) of 1.107 (P < 0.001). Higher residual renal volume, male gender, and older age were identified as independent risk factors for the development of CKD following open or laparoscopic donor nephrectomy during long-term follow-up.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) represents a significant global public health challenge, with a reported global prevalence of 13.4%, and end-stage renal disease (ESRD) affecting approximately 5–7 million individuals worldwide1. In Thailand, CKD affects over 11 million individuals, which accounts for 17.5% of the population, and 5.7 million people, or 8.6%, require renal replacement therapy for ESRD2.
Kidney transplantation (KT) is the primary standard for renal replacement therapy in cases of end-stage renal disease (ESRD)3. Research has consistently shown that patients who undergo KT experience better outcomes, including lower mortality rates, improved quality of life, and cost-effectiveness, when compared to those receiving haemodialysis4,5. Moreover, it is well-established that kidneys from living donors offer higher graft survival rates and lower mortality rates than kidneys from deceased donors6,7. In 2020, Thailand recorded a total of 714 kidney transplantations, with 136 involving living donors and 578 from deceased donors8,9.
Research has indicated that both open donor nephrectomy and laparoscopic donor nephrectomy yield comparable graft outcomes10,11. However, it is worth noting that donor nephrectomy carries a slight risk of inducing chronic kidney disease (CKD) and end-stage renal disease (ESRD) in the donor, estimated to be around 1–5%12,13. A previous study discovered that donors with a pre-donation renal volume of less than 140 ml face an increased risk of developing CKD within 12 months14. Similarly, another study suggested that preoperative renal volume serves as a protective factor against CKD, although this finding lacks long-term follow-up15. Consequently, our current study aims to assess the correlation between residual kidney volume and the risk of CKD following donor nephrectomy, with an extended follow-up period.
Methodology
Study population
This research received ethical approval from the Institutional Committee on Human Rights Related to Research Involving Human Subjects (MURA2019/855). All methods were carried out in accordance with relevant guidelines and regulations. A retrospective observational study was conducted on all patients who underwent open and laparoscopic donor nephrectomy between January 2011 and June 2019. The data collection was retrospective in nature and informed consent was waived by the Institutional Committee on Human Rights Related to Research Involving Human Subjects. In Thailand, a potential kidney donor should possess an estimated glomerular filtration rate (eGFR) exceeding 90 ml/min/1.73 m2. Individuals with a measured glomerular filtration rate (mGFR) below 70 ml/min/1.73 m2 are not considered eligible to be kidney donors. Additionally, they undergo assessments for proteinuria, haematuria, malignancies, and metabolic conditions that could impact both the transplantation outcomes and their post-procedural health. Screening for infectious and psychological diseases is also conducted. Furthermore, a CT angiography is essential for a thorough anatomical evaluation. Data collection extended until the last follow-up visit. Information collected included age, gender, body weight, height, body mass index (BMI), donated kidney side, residual renal volume, underlying diseases including diabetes mellitus, hypertension, dyslipidaemia, hepatitis B viral infection and estimated Glomerular Filtration Rate (eGFR). eGFR values were calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) method16, with CKD criteria set at eGFR < 60 ml/min/1.73 m2 for two consecutive follow-ups. Preoperative computed tomography (CT) scans were routinely utilized to assess renal volume. Patients were excluded if they lacked follow-up records and eGFR results beyond one month, or if their imaging data was incomplete.
Imaging procedure
Extended Brilliance Workspace system software, version 4.5.6.52040 (Philips Medical Systems, Markham, Ontario, Canada) were used to perform Computed Tomography Angiography (CTA) in order to formulate the preoperative renal volume for all patients. The images were oriented in the transverse plane to manually delineate the contours of the kidneys. We excluded the drainage system, vasculature of the renal sinus, adipose tissues in the renal sinus, and any cysts. The remaining renal volume was automatically computed using post-processing software. Furthermore, a technician conducted the measurements independently, performing two separate repetitions, without prior knowledge of the participants' characteristics.
Statistical analysis
Patients' baseline characteristics were reported in mean ± standard deviation (SD) or median with interquartile range (IQR). Univariate and multivariate analyses with cox proportional regression models were used to analyse the factors affecting long term kidney function. Correlation analyses were drawn for residual renal volume and CKD. All the data were analysed using Stata software, version 14.2 (StataCorp LLC, College Station, TX, USA).
Results
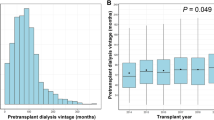
The study comprised 452 patients who had undergone donor nephrectomy. Among these, 289 individuals (63.94%) were female, and 163 (36.06%) were male. The average age of the donors was 39.57 ± 11.00 years (mean ± SD), as indicated in Table 1. A majority of the patients underwent donor nephrectomy on the left side (81.42%). The surgical procedures included open nephrectomy for 188 donors and laparoscopic nephrectomy for 264 donors. Twenty-three patients (5.09%), had underlying conditions such as dyslipidaemia, hypertension, or hepatitis B viral infection.
Prior to the surgery, the average total renal volume was 252.40 ± 46.64 ml. Patients who underwent right nephrectomy had a higher renal volume compared to those who had left nephrectomy, as outlined in Table 1. It is worth noting that a statistically significant difference exists between the percentage of remaining renal volume on the right side (128.87 ± 23.88 ml, 49.53 ± 2.56%) and the left side (127.40 ± 24.23 ml, 50.83 ± 2.22%), with a p-value of less than 0.001. In terms of remaining renal volume, gender, age, and underlying diseases did not exhibit significant differences between the two groups, as shown in Table 2.
Table 3 illustrates that 33.09% of donors developed eGFR deterioration within 1 month after nephrectomy and eGFR gradually decreased over the 24 months follow-up period with some minor variations. After the 24 months follow-up, the proportion of donors who developed CKD remained uniform at approximately 20%. The data lacks information on 41 patients who were lost to follow-up after the first month.
In reference to the risk factors associated with postoperative chronic kidney disease (CKD), the statistical analysis highlights that being male, advancing age, and the remaining kidney volume are significant factors. The hazard ratios (HR) with 95% confidence intervals (CI) are 4.013 (2.67- 6.03) for male gender, 1.107 (1.08–1.13) for age, and 1.675 (1.09–2.58) for remaining volume, as presented in Table 4.
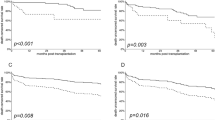
The Kaplan–Meier curve in Fig. 1 illustrates CKD development over a 5-year follow-up, comparing individuals with kidney remnants below 50% to those with remnants exceeding 50%. Those with greater kidney remnants exhibited a faster onset of CKD compared to those with less, with a Log rank P value of 0.049.
Discussion
In our research, we examined the long-term renal function in kidney donors. We identified that gender, age, and greater remaining renal volume independently contribute to the risk of developing chronic kidney disease (CKD) following both open and laparoscopic donor nephrectomy procedures. Our results contradicted those reported in previous studies with differing follow-up durations17,18. Hori et al. and Lange et al. both proposed a correlation between kidney volume and kidney function before and after donation. Additionally, Narasimhamurthy et al. indicated that kidney size is linked to the long-term eGFR. In fact, one study has indicated a robust correlation between the volume of the renal cortex and eGFR after kidney donation19. The total parenchymal renal volume contouring (ReRCoV) method has demonstrated the most substantial predictive efficacy for the development of chronic kidney disease (CKD) one year after kidney donation, as per previous research20.
Our results indicate that higher residual renal volume is associated with developing CKD in long-term follow-up, which contradicted previous studies. Meta-analysis by Habbous et al. might help clarify the inconsistencies, as they discovered that the apparent link between renal volume and post-donation renal function was notably diminished due to factors such as unadjusted measures, risk stratification, and reliance on input distribution21.
Another factor contributing to the disparity between our findings and previous research could be the differences in the measurement and eGFR calculation methods. Moreover, there is a lack of standardized approach for measuring renal volume using CT scans, and the methods differ in terms of software, equipment, and procedures. These include variations such as ReRCoV, total parenchymal three-dimensional renal volume, renal cortical volume, kidney function cortical volumetry (RCoV), and the ellipsoid method19,22. According to a study, it was claimed that RCoV is the most effective volumetric method for predicting post-renal outcomes19. Furthermore, the absence of standardization in the quality of the arterial phase for corticomedullary differentiation of the kidney hinders the comparability of findings from other studies.
Regarding the calculation of eGFR, our study employed the CKD-EPI method, while another research used the four-variable Modification of Diet in Renal Disease (MDRD) equation. Additionally, a separate study compared the accuracy of three eGFR calculation methods but found them to be less reliable than the Chromium-51 labelled ethylenediaminetetraacetic acid radioisotope GFR23. Notably, in the context of evaluating kidney donors, CKD-EPI has demonstrated superior performance in eGFR measurement compared to MDRD, underscoring the absence of standardization in GFR measurement24. At our institution, the majority of surgical procedures were conducted using laparoscopic technique, with a preference for left kidney donation. This preference is primarily due to the left laparoscopic donor nephrectomy being less surgically intricate, owing to the anatomically longer renal vein25,26, facilitating vascular anastomoses. When dealing with kidneys featuring multiple renal arteries, we evaluate the length of vessels on a case-by-case basis. We opt for the side with less complex vasculature to mitigate the risk of post-transplant ischemia in the renal units. In cases of differing kidney functions, nuclear renal scintigraphy was assessed and the lower functioning kidney is chosen for transplantation. Donors with kidney stones are advised to have them removed before transplantation. Removal of small, uncomplicated renal stones in the chosen kidney can be done after nephrectomy promptly with endoscopy on the operating table to minimize ischemic time before proceeding with transplantation.
Our findings suggested that the residual renal volume is typically higher in left donor nephrectomies, implying that, in general, the right kidney is larger than the left, as supported by our data and previous studies27. This could potentially be a confounding factor influencing the results. Moreover, we identified male gender as a significant risk factor for chronic kidney disease (CKD). While numerous studies have reported similar findings, the underlying reasons for the connection between male gender and CKD in donor nephrectomy cases remain unclear20,28. Some studies have proposed that both age and male gender could impact the renal reserve capacity29,30. Additionally, a separate research study established a link between the cortex-aortic enhancement index and the decline in eGFR, particularly in relation to male donors28.
Our study has certain limitations. Primarily, it is a retrospective observational study, thus could have been influenced by incomplete data and potential biases. Additionally, there is a significant number of participants who were lost to follow-up, impacting the analysis due to the limited number of reported CKD cases. Finally, some participants who marginally met the criteria for CKD and subsequently showed improvement in the subsequent visit, only to experience a decline in eGFR, leading to them meeting the CKD criteria again. These cases essentially represent two distinct occurrences of CKD.
Conclusion
Higher residual renal volume, increasing age and male gender were found to be independent risk predictors of developing CKD after open or laparoscopic donor nephrectomy in long-term follow-up.
Further research
To facilitate cross-study comparisons, it is imperative to standardize measurements by assessing various imaging procedures, methods for measuring renal volume, and eGFR calculation methods. This standardization is crucial to identify the optimal approach for evaluating kidney donors. Subsequently, further research is warranted to elucidate the underlying mechanisms contributing to the increased susceptibility of males to developing CKD following donor nephrectomy.
Data availability
Data supporting this study are included within the article.
References
Lv, J. C. & Zhang, L. X. Prevalence and disease burden of chronic kidney disease. Adv. Exp. Med. Biol. 1165, 3–15 (2019).
Kanjanabuch, T. & Takkavatakarn, K. Global dialysis perspective: Thailand. Kidney 1(7), 671–5 (2020).
Rodger, R. S. C. Approach to the management of end-stage renal disease. Clin. Med. (Lond.) 12(5), 472–475 (2012).
Yoo, K. D. et al. Superior outcomes of kidney transplantation compared with dialysis. Medicine (Baltimore) 95(33), e4352 (2016).
Voora, S. & Adey, D. B. Management of kidney transplant recipients by general nephrologists: Core curriculum 2019. Am. J. Kidney Dis. 73(6), 866–879 (2019).
Altieri, P., Piredda, G., Murgia, M. G., Onano, B. & Meloni, F. Clinical results of the various replacement therapies for chronic renal failure: Haemodialysis and renal transplantation. G. Ital Nefrol. 21(Suppl 26), S3-9 (2004).
Nemati, E., Einollahi, B., Lesan Pezeshki, M., Porfarziani, V. & Fattahi, M. R. Does kidney transplantation with deceased or living donor affect graft survival?. Nephrourol Mon. 6(4), e12182 (2014).
2020 TH.pdf [Internet]. [cited 2022 May 13]. https://www.transplantthai.org/data/annual_report/1/2020%20TH.pdf.
IRODaT - International Registry on Organ Donation and Transplantation [Internet]. [cited 2022 May 13]. https://www.irodat.org/?p=database&c=TH.
Simforoosh, N., Basiri, A., Tabibi, A., Shakhssalim, N. & Hosseini Moghaddam, S. M. M. Comparison of laparoscopic and open donor nephrectomy: A randomized controlled trial. BJU Int. 95(6), 851–855 (2005).
Simforoosh, N. et al. Long-term graft function in a randomized clinical trial comparing laparoscopic versus open donor nephrectomy. Exp. Clin. Transplant. 10(5), 428–432 (2012).
Lentine, K. L., Lam, N. N. & Segev, D. L. Risks of living kidney donation. Clin. J. Am. Soc. Nephrol. 14(4), 597–608 (2019).
Kiberd, B. A. & Tennankore, K. K. Lifetime risks of kidney donation: a medical decision analysis. BMJ Open 7(8), e016490 (2017).
Wu, F. M. W. et al. Preoperative renal volume: A surrogate measure for radical nephrectomy-induced chronic kidney disease. J. Endourol. 29(12), 1406–1411 (2015).
Leenanupunth, C., Hajidae, M. & Phongkitkaru, S. Correlation between preoperative remaining kidney volume and chronic kidney disease after donor nephrectomy. Insight Urol. 40(1), 22–29 (2019).
Pugliese, G. et al. The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation provides a better definition of cardiovascular burden associated with CKD than the Modification of Diet in Renal Disease (MDRD) Study formula in subjects with type 2 diabetes. Atherosclerosis 218(1), 194–199 (2011).
Lange, D. et al. Renal volume assessed by magnetic resonance imaging volumetry correlates with renal function in living kidney donors pre- and postdonation: a retrospective cohort study. Transpl. Int. 31(7), 773–780 (2018).
Hori, S. et al. Remnant renal volume can predict prognosis of remnant renal function in kidney transplantation donors: A prospective observational study. BMC Nephrol. 22(1), 367 (2021).
Gardan, E. et al. Renal cortical volume: High correlation with pre- and post-operative renal function in living kidney donors. Eur. J. Radiol. 1(99), 118–123 (2018).
Khalil, A. et al. Correlation and prediction of living-donor remaining function by using predonation computed tomography-based volumetric measurements: Role of remaining kidney volume. Exp. Clin. Transplant. 18(1), 39–47 (2020).
Habbous, S., Garcia-Ochoa, C., Brahm, G., Nguan, C. & Garg, A. X. Can split renal volume assessment by computed tomography replace nuclear split renal function in living kidney donor evaluations? A systematic review and meta-analysis. Can. J. Kidney Health Dis. 19(6), 2054358119875459 (2019).
Sharma, K. et al. Kidney volume measurement methods for clinical studies on autosomal dominant polycystic kidney disease. PLoS One 12(5), e0178488 (2017).
Burballa, C. et al. MDRD or CKD-EPI for glomerular filtration rate estimation in living kidney donors. Nefrologia (Engl. Ed.) 38(2), 207–212 (2018).
Lujan, P. et al. CKD-EPI instead of MDRD for candidates to kidney donation. Transplantation 94, 637–41 (2012).
Skrekas, G., Papalois, V. E., Mitsis, M. & Hakim, N. S. Laparoscopic live donor nephrectomy: A step forward in kidney transplantation?. JSLS 7(3), 197–206 (2003).
Bowdino CS, Owens J, Shaw PM. Anatomy, Abdomen and Pelvis, Renal Veins. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [cited 2022 May 19]. http://www.ncbi.nlm.nih.gov/books/NBK538298/.
Okur, A. et al. Relationship between kidney volume and body indexes in the Turkish population determined using ultrasonography. Int braz j urol. 40, 816–822 (2014).
Szczurowska, A. et al. Preoperative computed tomography parameters and deterioration of remaining kidney function in living donors. Transplan. Proc. 50(6), 1597–1601 (2018).
Massie, A. B. et al. Quantifying postdonation risk of ESRD in living kidney donors. J. Am. Soc. Nephrol. 28(9), 2749–2755 (2017).
Rook, M. et al. Nephrectomy elicits impact of age and BMI on renal hemodynamics: Lower postdonation reserve capacity in older or overweight kidney donors. Am. J. Transplan. 8(10), 2077–2085 (2008).
Acknowledgements
We would like to acknowledge Ms. Suraida Aeesoa for the data collection from the electronic medical records and statistical analysis support.
Author information
Authors and Affiliations
Contributions
T.H. was a major contributor in data interpretation and writing the manuscript. C.L. helped interpretation of data and did the administrative support. M.S. analysed and helped interpretation of data. P.S. contributed to the conception and design, data analysis, interpretation and revised the manuscript. S.P. did the data collection and the interpretation of data. W.K. and K.K. did the provision of study materials, patients and data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hoontrakul, T., Leenanupunth, C., Siantong, M. et al. Residual renal volume as a long-term independent predictive factor of developing chronic kidney disease after donor nephrectomy. Sci Rep 14, 5341 (2024). https://doi.org/10.1038/s41598-024-55499-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-55499-3
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.