Abstract
This study aimed to develop and validate prognostic nomograms that can estimate the probability of 1-, 3- and 5-year overall survival (OS) as well as cancer-specific survival (CSS) for Intrahepatic cholangiocarcinoma (ICCA) patients. Clinical data of 1446 patients diagnosed with ICCA between 2010 and 2017 from the Surveillance, Epidemiology, and End Results (SEER) database were analyzed. In both the OS and the CSS group, the training cohort and validation cohort were divided into a 7:3 ratio. Age, sex, AJCC T stage, AJCC N stage, AJCC M stage, surgical status, and tumor grade were selected as independent prognostic risk factors to build the nomograms. To compare the efficacy of predicting 1-, 3-, and 5-year OS and CSS rates of the nomogram with the 8th edition of the American Joint Committee on Cancer (AJCC) staging system, we evaluated the Harrell’s index of concordance (C-index), area under the receiver operating characteristic curve (AUC) and decision curve analysis (DCA) in both cohorts. The results showed the nomogram for 1-, 3-, and 5-year OS and CSS prediction performed better than the AJCC staging system. In the subgroup analysis for patients could not receive surgery as the primary treatment. We developed two nomograms for predicting the 1-, and 2-year OS and CSS rates following the same analysis procedure. Results indicate that the performance of both nomograms, which contained sex, AJCC T stage, AJCC M stage, chemotherapy, and tumor grade and prognostic factors, was also superior to the AJCC staging system. Meanwhile, four dynamic network-based nomograms were published. The survival analysis showed the survival rate of patients classified as high-risk based on the nomogram score was significantly lower compared to those categorized as low-risk (P < 0.0001). Finally, accurate and convenient nomograms were established to assist clinicians in making more personalized prognosis predictions for ICCA patients.
Similar content being viewed by others
Introduction
Intrahepatic cholangiocarcinoma (ICCA) is a highly lethal tumor with a 5‐year overall survival (OS) near 9%1. It remains the second most prevalent primary liver cancer, which is derived from epithelial cells of the second‐order bile ducts and represents approximately 20% of all hepatic malignancies2. In the past 4 decades, the prevalence of ICCA in the U.S. has been increasing rapidly from 0.44 to 1.18 cases per million3. However, compared with perihilar cholangiocarcinoma (pCC) or distal cholangiocarcinoma (dCC), which were both anatomic subtypes of cholangiocarcinoma, the early stage of ICCA was difficult to diagnose due to the asymptomatic clinical characters4. Most patients diagnosed with ICCA were at the advanced stage and only 20–30% of them were able to undergo complete surgical resection which remained the only potential therapy5. For patients in the advanced stage of ICCA, the chemotherapy regimen of gemcitabine plus cisplatin has been recommended as the first‐line therapy6. In addition, evidence regarding the survival benefits of radiation therapy, whether used alone or in combination, in the treatment of advanced-stage ICCA patients, is continuously accumulating7.
At present, the most commonly accepted survival prediction method for ICCA patients is the 8th edition American Joint Committee on Cancer (AJCC) staging system. However, it only analyzed factors including the local extension of the primary tumor, lymph node, and distant metastasis which neglected other factors such as age, sex, histological grade, and treatment status. Hence, it is necessary to incorporate various prognostic factors into one predictive system which would enable researchers to predict the prognosis of patients with greater accuracy.
Nomogram is a widely used tool for clinical decision-making, which could calculate the probability of clinical events by considering the prognostic weight of each factor and presenting the results visually8. Recent research endeavors have focused on developing nomograms as predictive tools for assessing the prognosis of patients with ICCA from different aspects. Some studies focused on predicting the overall survival (OS) of ICCA patients9,10,11, while some tried to predict the cancer-specific survival (CSS) of ICCA patients after surgery12,13. Liu et al. tried to construct a nomogram for predicting CSS in ICCA patients but failed due to the relatively small sample size (n = 189)14. However, insufficient research has been conducted on a comprehensive cohort of ICCA patients, including those who were ineligible for surgical treatment, resulting in a dearth of predictive models for estimating CSS of ICCA patients of all stages. Based on the current research status, we aimed to conduct a more comprehensive analysis of survival status prediction for patients with ICCA, including OS and CSS analyses. Furthermore, we conducted a subgroup analysis and discussion based on the overall analysis results.
In this study, we extracted independent prognostic factors obtained from the Surveillance, Epidemiology, and End Results (SEER) database to develop and validate two nomograms that can accurately predict OS and CSS in patients diagnosed with ICCA of different stages. According to the nomogram analysis results for OS and CSS, we performed a subgroup analysis according to the surgical status. Additionally, two separate nomograms were developed for patients who could not undergo surgery for primary treatment. In addition, by comparing the nomogram with the 8th AJCC staging system, we expect to demonstrate the model we established with greater performance.
Materials and methods
Study population and data extraction
We selected patients diagnosed with ICCA from the Incidence—SEER Research Plus Data, 18 Registries, Nov 2020 Sub (2000–2018) database. The data were acquired from the SEER*Stat software version 8.4.1. The inclusion criteria were as follows: (1) the International Classification of Diseases for Oncology, Third Edition (ICD-O-3) code was 8160/3: cholangiocarcinoma; (2) Primary Site-Labeled: C22.1-Intrahepatic bile duct; (3) Year of Diagnosis: “2010”, “2011”, “2012”, “2013”, “2014”, “2015”, “2016”, “2017”. Through preliminary screening, we obtained clinical data from 7401 patients. The exclusion criteria were as follows: (1) age of diagnosis below 20; (2) missing data of race, tumor (T) staging, lymph node (N) staging, and metastasis (M) staging of the AJCC staging system, surgical status, tumor grade, and tumor size; (3) ICCA not as the only or first primary tumor; (4) CSS less than 1 month. A total of 1446 patients meeting the criteria were included in the study.
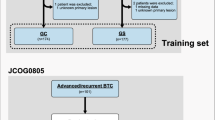
Based on the 1446 eligible patients, we further conducted a subgroup survival analysis based on the patient's cause of death, specifically whether it was due to the cancer, and whether the patient underwent surgical treatment. A total of four nomograms were established and validated to predict the survival status of ICCA patients. The overview of the research process is shown in Fig. 1.
Study variables
Clinical variables of each patient were obtained including year of diagnosis, age at diagnosis, sex, race, tumor size, tumor grade, surgical status, AJCC 7th edition of TNM stage, survival months, cause of death, chemotherapy, and radiation status. The tumor staging system was translated from the 7th edition AJCC system which was available for patients from 2010 to 2017 to the 8th edition based on tumor characteristics15. The age variable was divided into four groups, namely (1) below 50 years old; (2) 50–64 years old; (3) 65–79 years old; (4) no less than 80 years old. Tumor size was divided into two groups: diameter no more than 5 cm and over 5 cm. OS was defined as the time from diagnosis to death or the last follow-up, and CSS excluded the death of other causes.
Statistical analysis
R (version 4.2.1) was the primary analytical software utilized in this study. Two-tailed P values < 0.05 were considered statistically significant. Each analysis group was divided into the training cohortand validation cohortwith a proportion of 7:3 randomly using the “Random Samples and Permutations” function in R14,16. The training cohort was utilized for model construction, while the validation cohort was employed for model validation. Continuous data were reported as the median with interquartile range (IQR), while categorical data were presented as frequencies (proportions) and compared using the Chi-square test. In the univariable Cox proportional hazards regression analyses, the Wald test was used and significance thresholds below 0.05 was considered to be statistically significant. Univariable Cox proportional hazards regression analyses were performed to screen statistically significant variables for further multivariate Cox proportional hazards regression analyses. Seven independent prognostic factors were selected for nomogram construction for predicting 1-, 3- and 5-year OS and CSS rates in ICCA patients based on Kaplan–Meier analyses using the survival package of R. Based on the same analytical method, five independent prognostic factors were screened out for nomogram construction in the subgroup analysis for predicting 1-, and 2-year OS and CSS rates in ICCA patients.
To evaluate the performance of the nomogram, the discriminative power was assessed using the Harrell concordance index (C-index) through internal validation and external validation using the validation cohort. The R packages Hmisc and rms were employed, and bootstrap resampling with 1000 resamples was performed9. The agreement between predictions and observations was evaluated by the calibration curve using R package rms17. Compared to the AJCC 8th TNM staging system as a reference, the time-dependent area under the ROC curves (AUC) using R package survivalROC18 and decision curve analysis (DCA) using R package rmda19 were employed to evaluate the clinical utility and net benefit of the nomogram. In addition, based on the scores derived from the nomogram constructed using the training cohort, patients from two cohorts were divided into high-risk and low-risk groups in a 1:1 ratio accordingly. To assess the risk stratification effect of the nomogram, survival analysis was conducted utilizing Kaplan–Meier (KM) curves and Cox proportional hazard models. Finally, the R package DynNom was utilized to build a web-based nomogram on the Shiny application platform20.
Ethical approval
The author Y-GL has gotten access to the SEER database and signed the “Surveillance, Epidemiology, and End Results Program Data Use Agreement”. This study obtained clinical data from the SEER database, where informed consent from patients was not required.
Results
Demographic and clinical characteristics
A total of 1446 patients diagnosed with ICCA were included from 2010 to 2017 to ensure a follow-up time of no less than 5 years. In the OS analysis group, there were 1446 eligible patients. The training (n = 1012) and validation (n = 434) cohort was randomly generated from the whole population with a proportion of 7:3. In the total cohort of ICCA patients, the majority of patients were between 50 to 80 years old (80.7%) and white (78.1%). The majority of patients were diagnosed with T1 and T2 stages (77.0%), with no lymph nodes (67.0%) or distant metastasis (75.9%). Out of the total cohort, only 13 patients had pathological grade IV, making up a mere 0.9% of the proportion. Accordingly, the groups with pathological grades IV and III were consolidated into a single category. Regarding treatment, surgical intervention was performed in 48.0% of the patients, while the majority (61.5%) underwent chemotherapy. Radiotherapy, on the other hand, was administered to only 16.0% of the patients. The training set and validation set exhibit statistically significant differences in Grade distribution (P = 0.013). Apart from this, the other baseline characteristics between the two cohorts were balanced (Table 1).
Excluding 59 patients who died due to other causes of death, a total of 1387 patients were included in the CSS analysis. The training (n = 970) and validation (n = 417) cohort was also distributed in a 7:3 ratio of populations. In terms of demographic characteristics, the CSS group and OS group exhibited similar compositions. The majority of the patients were white (77.9%) and between 50 to 80 years old (80.8%). 1065 patients (76.8%) were diagnosed with T1 and T2 stages. The majority (52.1%) of patients have not undergone surgery and only 16.1% of patients underwent radiotherapy. The proportion of patients receiving chemotherapy was higher in the training set with statistical significance (P = 0.014). The rest baseline characteristics between the two cohorts were balanced (Table 2).
Variables screening and nomogram construction
Prior to conducting the univariable Cox regression analysis for each group, we employed Spearman's correlation to verify the absence of collinearity among the screened variables (Supplementary Fig. 1).
In the OS group, we selected eight independent prognostic factors based on the univariable Cox proportional hazards regression analyses in the training cohort: age no less than 65 years old (hazard ratio [HR] = 1.416/2.073, P < 0.01), male (HR = 1.207, P = 0.011), AJCC T2/T3/T4 (HR = 1.651/1.923/1.807, P < 0.001), AJCC N1 (HR = 1.746, P < 0.001), AJCC M1 (HR = 2.407, P < 0.001), tumor grade III + IV (HR = 1.746, P < 0.001), tumor size over 5 cm (HR = 1.458, P < 0.001) and receiving surgery (HR = 0.311, P < 0.001). In the next step, multivariable Cox proportional hazards regression analyses were conducted based on these eight prognostic factors. As a result, seven independent prognostic factors were identified, which showed a significant association with OS in patients with ICCA (Table 3). No significant association between tumor size and OS was revealed in the multivariable Cox regression analysis (HR = 1.048, P = 0.575). In addition, chemotherapy (HR = 0.935, P = 0.380) and radiotherapy (HR = 0.911, P = 0.353) were not prognostic factors for OS in ICCA patients.
In the CSS group, by employing univariable and multivariable Cox regression analyses, the same seven prognostic factors were identified: age, sex, AJCC T stage, AJCC N stage, AJCC M stage, surgery status, and tumor grade. The detailed information on univariable and multivariable Cox regression analyses in the CSS group is shown in Table 4.
Based on the seven prognostic factors and utilizing the training cohort as the data source, we developed two nomograms using the multivariate Cox prognostic model for ICCA patients which enabled the prediction of 1-, 3-, and 5-year OS and CSS rates (Fig. 2). For each patient, every independent predictor with different weights has its corresponding points on the first line. The total points of a patient could be acquired by adding up the points of each factor, which corresponded vertically to the 1-, 3-, and 5-year OS and CSS rates at the bottom lines.
(a) Nomogram predicting 1-, 3- and 5-year OS of patients with ICCA. (b) Nomogram predicting 1-, 3- and 5-year CSS of patients with ICCA. The total points were added up from the corresponding predictors, and through the vertical correspondence relationship, we could get the predicted probability of 1-, 3- and 5-year survival.
Nomogram validation
In the OS group, the C-index of the nomogram in the training and validation cohorts were 0.719 (0.695–0.743) and 0.723 (0.685–0.760) respectively. As a comparison, the C-index of the 8th AJCC staging was 0.648 (0.624–0.671) and 0.638 (0.601–0.674) in the training and validation cohorts. In the CSS group, The C-index of the nomogram in the training and validation cohorts were 0.726 (0.701–0.751) and 0.711 (0.673–0.749). In comparison, the C-index of the 8th AJCC staging was 0.663 (0.639–0.687) and 0.617 (0.580–0.654) in the training and validation cohorts. Furthermore, calibration curves of 1-, 3-, and 5-year OS and CSS were established in both cohorts (Fig. 3a–l). In the calibration plot, a model's observed and predicted probabilities depicted by a dashed line that precisely aligns with the diagonal slash on the plot would be considered highly efficient. In the training and validation cohorts, the 1-, 3-, and 5-year OS and CSS rates predicted by the nomogram were in good agreement with survival status.
Calibration curves of the nomogram for the 1-, 3-, and 5-year OS prediction of patients with ICCA in the training cohort (a–c) and the validation cohort (d–f). Calibration curves of the nomogram for the 1-, 3-, and 5-year CSS prediction of patients with ICCA in the training cohort (g–i) and the validation cohort (j–l).
To compare the performance of the nomogram with the 8th AJCC staging system, the time-dependent ROC curves and DCA curves were plotted. Notably, all of these AUC values surpass the corresponding AUC values of the AJCC stage in both the OS and CSS group, the AUC of the nomogram and the AJCC stage could be observed in Fig. 4a–l. In the OS group, the nomogram consistently exhibits an AUC greater than 0.74 when predicting the 1-, 3-, and 5-year OS rates. While in the CSS group, the nomogram accordingly exhibits an AUC greater than 0.75. More parameters of the nomogram including the positive predictive value for death at 1-, 3-, and 5-year, sensitivity, and specificity at the cut-off point accordingly are listed in Table 5. The result suggested that the nomogram demonstrated favorable discrimination capabilities.
ROC curves of both the nomogram and the 8th AJCC TNM staging system in the training cohort (a–c) and the validation cohort (d–f) for 1-, 3-, and 5-year OS prediction. ROC curves of both the nomogram and the 8th AJCC TNM staging system in the training cohort (g–i) and the validation cohort (j–l) for 1-, 3-, and 5-year CSS prediction.
In addition, we performed DCA analyses in both cohorts to demonstrate the net benefit of the nomogram compared to the AJCC stage (Fig. 5a–l). The DCA analysis can reveal the variation in net benefit as the threshold probability changes based on the model's predicted values21. For instance, in Fig. 5a, if the threshold that one patient had the possibility of 45% dying within 1 year (at the 45% risk threshold), the net benefit was higher in the nomogram model than in the AJCC staging system. In other words, the use of a nomogram for prognosis analysis and subsequent treatment decisions may yield greater net benefits compared to decisions based on the AJCC staging system from wider thresholds. The decisions involved comprehensive and proactive treatment measures for patients, including surgery, aiming to improve both OS and CSS. As a result, the developed nomogram exhibited a greater net benefit when predicting the 1-, 3-, and 5-year OS and CSS rates compared to the 8th AJCC TNM staging system.
Decision curves of both the nomogram and the 8th AJCC TNM staging system in the training cohort (a–c) and the validation cohort (d–f) for 1-, 3-, and 5-year OS prediction. Decision curves of both the nomogram and the 8th AJCC TNM staging system in the training cohort (g–i) and the validation cohort (j–l) for 1-, 3-, and 5-year CSS prediction. The x-axis is the threshold probability, and the y-axis is the net benefit rate. The horizontal dashed line indicates 0 net benefits when all patients with ICCA are not treated. The smooth diagonal line indicates when all patients with ICCA are treated regardless of the predictive model.
Above all, the nomogram we constructed demonstrated superior discriminative ability and accuracy when compared to the 8th AJCC TNM staging system.
Risk stratification for survival analysis
In the OS group, according to the total points derived from the nomogram in the training cohort, we divided patients into high-risk and low-risk groups based on the average score (total points over 187 or under 187) and conducted a survival analysis (Fig. 6a,b). In the training cohort, 506 patients were classified as the low-risk group, with a median OS of 29 (95% CI 24.36–33.65) months. On the other hand, 506 patients were assigned to the high-risk group, with a median OS of 9 (95% CI 7.73–10.27) months. Similarly, the validation cohort was categorized into high-risk and low-risk groups based on the score threshold determined by the training cohort, with the median OS as 9 (95% CI 7.45–10.55) months and 40 (95% CI 31.65–48.35) months. The differences in KM curves between high-risk and low-risk groups are all statistically significant in both cohorts (P < 0.0001).
In the CSS group, high-risk and low-risk groups were separated by the score threshold of 162, and survival analysis was similarly performed (Fig. 6c,d). In the training cohort, the low-risk group has a median CSS of 36 months (95% CI 29.80–42.20), while the high-risk group has a median CSS of 9 months (95% CI 7.86–10.14). In the validation cohort, the high-risk group has a median CSS of 10 months (95% CI 8.06–11.94) and the low-risk group has a median CSS of 37 months (95% CI 22.37–51.63). The differences between high-risk and low-risk groups are statistically significant (P < 0.0001).
Subgroup analysis for ICCA patients without surgery
In both the OS and CSS group, more than half of patients could not undergo surgery for primary treatment (52.0% and 52.1% in the OS group and CSS group separately). While surgical status constitutes a significant proportion of our nomogram model. By conducting a survival analysis of all eligible patients in the OS and CSS group, stratified by surgical status, we identified a significant difference in the prognosis between patients who underwent surgery and those who did not (P < 0.0001) (Fig. 7a,b). Therefore, we conducted a subgroup analysis for the patients without surgery and developed another two nomograms to predict the OS and CSS of these patients.
In the OS analysis group, there were 752 eligible patients. The training (n = 526) and validation (n = 226) cohort was randomly generated from these patients with a proportion of 7:3. In the CSS analysis group, excluding 30 patients who died due to other causes of death, a total of 722 patients were included, including 505 patients from the training cohort and 217 patients from the validation cohort. The demographic and clinical characteristics of the OS group and CSS group were presented in Tables 6 and 7 separately. It is noteworthy that the median survival time of patients in the non-surgical group significantly shortened (P < 0.0001).
In both the OS and CSS groups, by performing univariable and multivariable Cox proportional hazards regression analyses, we screened out the same five independent prognostic factors for the nomogram construction: sex, AJCC T stage, AJCC M stage, tumor grade, and chemotherapy status. The detailed information on univariable and multivariable Cox regression analyses in the OS and CSS group is shown in Supplementary Table 1 and Supplementary Table 2 accordingly.
Differing from the overall population, patients in the non-surgical group experienced a significantly shortened survival time (P < 0.0001). In the training cohort of the OS group, only 1.3% of the patients reached the OS of 5 years and 5.5% reached the OS of 3 years. In the training cohort of the CSS group, the corresponding proportions were 1.4% and 5.7% respectively. Based on patient survival status and five prognostic factors, we developed two nomograms using the multivariate Cox prognostic model for ICCA patients without surgery which enabled the prediction of 1-, and 2-year OS and CSS rates (Fig. 8a,b). To validate the nomogram, we calculated the C-index, AUC of ROC curves, drew calibration curves, and performed the DCA analysis in each cohort.
(a) Nomogram predicting 1-, and 2-year OS for ICCA patients without surgery. (b) Nomogram predicting 1-, and 2-year CSS for ICCA patients without surgery. (c) A web-based dynamic nomogram predicting OS probabilities for ICCA patients without surgery (available at: https://tumornomogram.shinyapps.io/Intrahepatic_cholangiocarcinoma_OS_a/).
In the OS group, The C-index of the nomogram in the training and validation cohorts were 0.676 (0.644–0.709) and 0.700 (0.650–0.750) respectively. As a comparison, the C-index of the 8th AJCC staging was 0.544 (0.514–0.575) and 0.597 (0.549–0.650) in the training and validation cohorts. In the CSS group, The C-index of the nomogram in the training and validation cohorts were 0.680 (0.647–0.713) and 0.694 (0.642–0.745). In comparison, the C-index of the 8th AJCC staging was 0.547 (0.519–0.578) and 0.600 (0.551–0.649) in the training and validation cohorts. Calibration curves of the nomogram for predicting the 1-, and 2-year OS and CSS rates in both cohorts showed good agreement with survival status (Supplementary Fig. 2a–h).
Time-dependent ROC curves and DCA curves were plotted to compare the performance of the nomogram with the 8th AJCC staging system, and all of the AUC values surpassed the corresponding AUC values of the AJCC stage in both the OS and CSS group. Figure 9a–h exhibited the AUC of the nomogram and the AJCC stage in each ROC curve. More detailed parameters of the nomogram are listed in Table 8. The AUC for the prediction of 1-year survival in both the OS and CSS groups was higher than the prediction of 2-year survival.
ROC curves of both the nomogram and the 8th AJCC TNM staging system in the training cohort (a,b) and the validation cohort (c,d) for 1-, and 2-year OS prediction of ICCA patients without surgery. ROC curves of both the nomogram and the 8th AJCC TNM staging system in the training cohort (e,f) and the validation cohort (g,h) for 1-, and 2-year CSS prediction of ICCA patients without surgery.
DCA analyses in both cohorts were performed to exhibit the net benefit of the nomogram compared to the AJCC stage, and the nomogram exhibited a greater net benefit when predicting the 1-, and 2-year OS and CSS rates compared to the 8th AJCC TNM staging system (Supplementary Fig. 3a–h).
Survival analyses were performed according to the risk score. In the training cohort of the OS group, among the 259 patients categorized as the low-risk group with a score below 116, the median survival was 16 months (95% CI 14.16–17.84). The rest 267 patients were assigned to the high-risk group, with a median survival of 6 (95% CI 4.90–7.10) months. In the validation cohort of the OS group, the median survival time was 16 (95% CI 13.23–18.77) months and 3 (95% CI 2.10–3.90) months accordingly. In the training cohort of the CSS group, of the 257 patients with a score below 109 identified in the low-risk group, the median survival was 16 (95% CI 14.22–17.78) months. Conversely, the high-risk group comprised 248 patients, with a median survival of 6 (95% CI 4.89–7.11) months. In the validation cohort of the CSS group, the median survival time was 16 (95% CI 12.88–19.12) months and 4 (95% CI 2.60–5.40) months accordingly. The differences in KM curves between high-risk and low-risk groups were all statistically significant in both cohorts (P < 0.0001) (Fig. 10a–d).
Kaplan–Meier curves for ICCA patients without surgery in the low- and high-risk groups in the training cohort (a) and validation cohort (b) for the prediction of OS. Kaplan–Meier curves for patients in the low- and high-risk groups in the training cohort (c) and validation cohort (d) for the prediction of CSS.
Nomogram publication
After performing the validation and comparative evaluation analysis aforementioned, our nomograms have demonstrated reliability. To further assist researchers in conveniently predicting ICCA patient prognosis, we published four web-based nomograms (https://tumornomogram.shinyapps.io/Intrahepatic_cholangiocarcinoma_OS/, https://tumornomogram.shinyapps.io/Intrahepatic_cholangiocarcinoma_OS_a/, https://tumornomogram.shinyapps.io/Intrahepatic_cholangiocarcinoma_CSS/, and https://tumornomogram.shinyapps.io/Intrahepatic_cholangiocarcinoma_CSS_a/) which could allow for the dynamic visualization of one individual patient’s prognostic outcome. Figure 8c provides an overview of one web-based nomogram for the prediction of OS probabilities for ICCA patients without surgery.
Discussion
ICCA is one of the most common malignant tumors in elderly patients, with an average age of diagnosis around 70 years22. Both the incidence and mortality of patients with ICCA have been increasing steadily over the past 2 decades4. The challenges in early diagnosis of ICCA and the limited availability of radical surgical options further impact the prognosis of patients with ICCA. Therefore, one specifically developed prognostic prediction model for ICCA patients was required to assist researchers in accurately assessing prognosis and facilitating informed treatment decisions. In our study, we constructed four nomograms to predict the OS and CSS of ICCA patients depending on the surgical status of patients, and after validation, the nomograms demonstrated robust discriminative performance and calibration. Moreover, the risk stratification exhibited a commendable capability to distinguish ICCA patients into high- and low-risk groups.
Currently, the most widely used 8th edition of the AJCC staging system was imprecise in prognosis evaluation23. In comparison to the AJCC staging system, the development of a nomogram allows for the inclusion of additional risk factors including age, sex, and treatment status, enabling more precise prognoses. Several researchers have utilized nomograms solely for the prediction of OS in patients with ICCA9,10,11, without considering non-cancer-specific mortality. This oversight is particularly significant when considering the substantial population of elderly patients. Some previously published nomograms predicting CSS in ICCA patients concentrated more on the survival status after surgery12,13, which also excluded a significant number of patients who were not able to undergo surgical treatment and restricted the scope of their applicability. Zhao et al. previously conducted a population‑based analysis to build a prognostic model for CSS prediction in ICCA patients24. In contrast to our study, their investigation encompassed a broader spectrum of morphological categories, encompassing spindle cell carcinoma, squamous cell carcinoma, adenocarcinoma, scirrhous adenocarcinoma, and others, rather than being limited to cholangiocarcinoma as typically observed in most relevant research studies, which may result in a reduction in the accuracy of the model. Above all, in the current landscape of prognostic research on ICCA, there is a lack of comprehensive studies on both the OS and CSS analysis. Our study addressed this gap in the field. Additionally, we have embarked on pioneering exploration for the subset of patients who could not undergo surgery.
In the univariable regression analysis of both the OS and CSS group, age, sex, AJCC T stage, AJCC N stage, AJCC M stage, surgery, tumor grade, and tumor size were potential prognostic factors for ICCA patients. After conducting subsequent multivariate regression analysis, it was revealed that the rest seven factors, excluding tumor size, were identified as independent prognostic factors for the development of the nomogram. In both groups, the predictive capability of the nomogram surpassed that of AJCC staging. In addition, the C-index levels between the training set and validation set remained consistent, reflecting the reliability of the nomograms.
Similar findings were observed in the ROC analysis that the nomogram demonstrated superior performance compared to the AJCC staging system (Fig. 4a–l). A widely accepted criterion for determining the discriminative ability of a model is to consider it relatively good if its C-index and AUC surpass the threshold of 0.725. Therefore, our nomogram exhibits a robust discriminatory capacity. In addition, the calibration plots aligned closely with the diagonal slash, indicating excellent calibration of our nomograms26. In the DCA analysis to evaluate the net benefits of different risk thresholds, our nomogram exhibited higher clinical benefits than the AJCC stage in predicting the OS and CSS of patients with ICCA.
Notably, our research found that surgical status had the most significant weight in both nomograms. For ICCA patients, surgery remained the mainstream of the treatment which may prolong a median disease‐free survival up to 34 months27. The primary reasons for unresectable patients include multiple tumors, nodal or peritoneal metastases, and advanced hepatic disease5. For patients with unresectable and metastatic ICCA, chemotherapy with a combination of gemcitabine and cisplatin was recommended as the primary treatment with a median OS of 11.7 months28. One recent study has shown promising results for utilizing the nanoparticle albumin-bound-paclitaxel plus gemcitabine-cisplatin regimen in converting patients who are not eligible for surgery into viable candidates for surgical intervention29. Another recent study has confirmed that when chemotherapy is combined with toripalimab and lenvatinib, it exhibited potential for conversion therapy30. Therefore, although chemotherapy was not one of the independent predictors in the OS and CSS group, we should take note of the contributions of chemotherapy-based treatment in conversion therapy.
Considering that more than half of the patients could not receive surgery as primary treatment in our whole cohort, and coupled with the substantial weight attributed to the surgical status in our results, we performed a subgroup analysis for patients without surgery to explore factors influencing the prognosis of these patients. Constrained by the unfavorable prognosis of patients unable to undergo surgery, our predicted survival time was limited to 1 year and 2 years. We performed two nomograms for the prediction of the OS and CSS accordingly, and both the nomograms contained the same five independent predictive factors: sex, AJCC T stage, AJCC M stage, tumor grade, and chemotherapy. Chemotherapy had the highest contribution to both nomograms. This aligned with the current treatment recommendations for advanced-stage ICCA, advocating for an active systemic therapy centered around chemotherapy. Although the predictive capabilities of both nomograms surpassed the AJCC staging system, they exhibited weaker performance in predicting 2-year OS and CSS compared to their 1-year predictions. The AUC of the nomogram for predicting 2-year OS and CSS in the training cohort was 0.690 and 0.697 respectively, not surpassing 0.7. We attributed this to the limited sample size of patients achieving a 2-year prognosis. However, our nomogram still demonstrated high accuracy in predicting 1-year survival.
In our study, we incorporated various factors that influenced the OS and CSS of ICCA patients from both demographic and treatment perspectives. While confirming the prognostic value of AJCC staging in patients with ICCA, we have also affirmed the benefits of surgical treatment and chemotherapy for patient prognosis. Therefore, we recommended that ICCA patients should be further divided into high-risk and low-risk groups according to the nomogram risk score to better differentiate the distinct prognoses between the two groups of patients. In our survival analysis, there were significant differences in the median survival time between high-risk and low-risk groups. Therefore, early identification of patients' prognostic status holds crucial guidance for implementing more personalized treatment strategies. For example, if one patient could not receive surgery and was categorized into the high-risk group, based on the currently published clinical survival time and prognosis benefit outcomes, selecting proper clinical trials based on genetic testing results may lead to more effective treatment outcomes. Furthermore, we developed user-friendly web-based predictive tools aimed at facilitating physicians in conducting patient prognosis assessments and implementing personalized treatment plans more conveniently.
Undeniably, this study still has shortcomings. Firstly, this is a retrospective study which may contain selection bias due to the lack of clinical data. Secondly, data extracted from the SEER database lacked information on immunotherapy and targeted therapy, which could effectively improve patient survival. Thirdly, the SEER database only included patients from the United States where the Asian population represented only a small fraction. Whether the result could be utilized in populations of different races, especially in Southeast Asian countries where the incidence of ICCA was much higher than HCC still needs further research4. Finally, in the nomograms, the weight of surgery and chemotherapy are the highest, but radiation is not included in the nomogram. Although nomogram could apply to predict the prognosis, we should not overlook the positive impact of other treatment modalities, including radiotherapy, on patient prognosis. The recommendation of treatment modality should be seriously treated.
Conclusion
In summary, the nomograms which included age, sex, AJCC T, N, M stage, surgery status, and tumor grade as independent prognostic factors for predicting 1-, 3-, and 5-year OS and CSS rates in ICCA patients performed better than the traditional AJCC staging system. For patients who could not receive surgery as primary treatment, the nomograms which included sex, AJCC T, M stage, tumor grade, and chemotherapy as independent prognostic factors for predicting 1-, and 2-year OS and CSS rates also performed better than the AJCC staging system. Notably, surgical status contributed most to the OS and CSS nomograms, and for patients without surgery, chemotherapy contributed most to the OS and CSS prediction. These novel nomograms could enable more accurate prognostic prediction and help clinicians provide better-personalized healthcare.
Data availability
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author. Publicly available datasets of this study could be acquired from: https://seer.cancer.gov/.
References
Yao, K. J., Jabbour, S., Parekh, N., Lin, Y. & Moss, R. A. Increasing mortality in the United States from cholangiocarcinoma: An analysis of the National Center for Health Statistics Database. BMC Gastroenterol. 16, 117. https://doi.org/10.1186/s12876-016-0527-z (2016).
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 72, 7–33. https://doi.org/10.3322/caac.21708 (2022).
Saha, S. K., Zhu, A. X., Fuchs, C. S. & Brooks, G. A. Forty-year trends in cholangiocarcinoma incidence in the U.S.: Intrahepatic disease on the rise. Oncologist 21, 594–599. https://doi.org/10.1634/theoncologist.2015-0446 (2016).
Moris, D. et al. Advances in the treatment of intrahepatic cholangiocarcinoma: An overview of the current and future therapeutic landscape for clinicians. CA Cancer J. Clin. 73, 198–222. https://doi.org/10.3322/caac.21759 (2023).
Endo, I. et al. Intrahepatic cholangiocarcinoma: Rising frequency, improved survival, and determinants of outcome after resection. Ann. Surg. 248, 84–96. https://doi.org/10.1097/SLA.0b013e318176c4d3 (2008).
Benson, A. B. III. et al. Hepatobiliary cancers, version 2.2014. J. Natl. Compr. Cancer Netw. 12, 1152–1182. https://doi.org/10.6004/jnccn.2014.0112 (2014).
Wang, N. et al. Progress in radiotherapy for cholangiocarcinoma. Front. Oncol. 12, 868034. https://doi.org/10.3389/fonc.2022.868034 (2022).
Iasonos, A., Schrag, D., Raj, G. V. & Panageas, K. S. How to build and interpret a nomogram for cancer prognosis. J. Clin. Oncol. 26, 1364–1370. https://doi.org/10.1200/JCO.2007.12.9791 (2008).
Yuan, C., Hu, Z., Wang, K. & Zou, S. Development and validation a nomogram for predicting overall survival in patients with intrahepatic cholangiocarcinoma. Front. Surg. 8, 659422. https://doi.org/10.3389/fsurg.2021.659422 (2021).
Xing, H., Tan, B., Yang, C. & Zhang, M. Incidence trend and competing risk analysis of patients with intrahepatic cholangiocarcinoma: A population-based study. Front. Med. (Lausanne) 9, 846276. https://doi.org/10.3389/fmed.2022.846276 (2022).
Wang, Y. et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J. Clin. Oncol. 31, 1188–1195. https://doi.org/10.1200/JCO.2012.41.5984 (2013).
Huang, G. et al. Prognostic nomogram for cancer-specific survival in patients with intrahepatic cholangiocarcinoma after hepatectomy: A population study of 919 patients. Front. Surg. 9, 1025521. https://doi.org/10.3389/fsurg.2022.1025521 (2022).
Ma, K. et al. Nomograms for predicting overall survival and cancer-specific survival in patients with surgically resected intrahepatic cholangiocarcinoma. Cancer Manag. Res. 11, 6907–6929. https://doi.org/10.2147/CMAR.S212149 (2019).
Liu, K. et al. Construction and validation of a nomogram for predicting cancer-specific survival in hepatocellular carcinoma patients. Sci. Rep. 10, 21376. https://doi.org/10.1038/s41598-020-78545-2 (2020).
Lee, A. J. & Chun, Y. S. Intrahepatic cholangiocarcinoma: The AJCC/UICC 8th edition updates. Chin. Clin. Oncol. 7, 52. https://doi.org/10.21037/cco.2018.07.03 (2018).
Jiang, S. et al. A novel nomogram based on log odds of positive lymph nodes to predict survival for non-metastatic gallbladder adenocarcinoma after surgery. Sci. Rep. 12, 16466. https://doi.org/10.1038/s41598-022-20933-x (2022).
He, C. et al. Nomogram to predict cancer-specific survival in patients with pancreatic acinar cell carcinoma: A competing risk analysis. J. Cancer 9, 4117–4127. https://doi.org/10.7150/jca.26936 (2018).
Huang, R., Chen, Z., Li, W., Fan, C. & Liu, J. Immune system-associated genes increase malignant progression and can be used to predict clinical outcome in patients with hepatocellular carcinoma. Int. J. Oncol. 56, 1199–1211. https://doi.org/10.3892/ijo.2020.4998 (2020).
Van Calster, B. et al. Reporting and interpreting decision curve analysis: A guide for investigators. Eur. Urol. 74, 796–804. https://doi.org/10.1016/j.eururo.2018.08.038 (2018).
Huang, Y., Wang, C., Tang, D., Chen, B. & Jiang, Z. Development and validation of nomogram-based prognosis tools for patients with extremity osteosarcoma: A SEER population study. J. Oncol. 2022, 9053663. https://doi.org/10.1155/2022/9053663 (2022).
Vickers, A. J., van Calster, B. & Steyerberg, E. W. A simple, step-by-step guide to interpreting decision curve analysis. Diagn. Progn. Res. 3, 18. https://doi.org/10.1186/s41512-019-0064-7 (2019).
Florio, A. A. et al. Global trends in intrahepatic and extrahepatic cholangiocarcinoma incidence from 1993 to 2012. Cancer 126, 2666–2678. https://doi.org/10.1002/cncr.32803 (2020).
Kang, S. H. et al. Prognostic comparison of the 7th and 8th editions of the American Joint Committee on Cancer staging system for intrahepatic cholangiocarcinoma. J. Hepatobiliary Pancreat. Sci. 25, 240–248. https://doi.org/10.1002/jhbp.543 (2018).
Zhao, K., Yang, D., Zhou, Y. & Ding, Y. Clinical features and prognostic models in patients with intrahepatic cholangiocarcinoma: A population-based analysis. J. Gastrointest. Surg. 27, 945–955. https://doi.org/10.1007/s11605-023-05602-2 (2023).
Steyerberg, E. W. et al. Prediction of indolent prostate cancer: Validation and updating of a prognostic nomogram. J. Urol. 177, 107–112. https://doi.org/10.1016/j.juro.2006.08.068(discussion 112)
Van Calster, B. et al. A calibration hierarchy for risk models was defined: From utopia to empirical data. J. Clin. Epidemiol. 74, 167–176. https://doi.org/10.1016/j.jclinepi.2015.12.005 (2016).
Mavros, M. N., Economopoulos, K. P., Alexiou, V. G. & Pawlik, T. M. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: Systematic review and meta-analysis. JAMA Surg. 149, 565–574. https://doi.org/10.1001/jamasurg.2013.5137 (2014).
Valle, J. et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N. Engl. J. Med. 362, 1273–1281. https://doi.org/10.1056/NEJMoa0908721 (2010).
Shroff, R. T. et al. Gemcitabine, cisplatin, and nab-paclitaxel for the treatment of advanced biliary tract cancers: A phase 2 clinical trial. JAMA Oncol. 5, 824–830. https://doi.org/10.1001/jamaoncol.2019.0270 (2019).
Shi, G. M. et al. Toripalimab combined with lenvatinib and GEMOX is a promising regimen as first-line treatment for advanced intrahepatic cholangiocarcinoma: A single-center, single-arm, phase 2 study. Signal Transduct. Target. Ther. 8, 106. https://doi.org/10.1038/s41392-023-01317-7 (2023).
Acknowledgements
For the completion of this study, I would like to express my deepest gratitude to Prof. Xu and Prof. Lu, who have given me the most valuable suggestions and guides.
Funding
This article was partially sponsored by the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (CIFMS) (No. 2020-I2M-CT-B-026), the National High Level Hospital Clinical Research Funding (2022-PUMCH-C-049 and 2022-PUMCH-A-237).
Author information
Authors and Affiliations
Contributions
X.L. and Y.-Y.X. conceived and designed the study. Y.-G.L. wrote the manuscript and participated in the design of the study. S.-T.J. and Y.-G.L. were responsible for data analysis. All authors contributed to the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, YG., Jiang, ST., Zhang, JW. et al. Development and validation of web-based nomograms for predicting survival status in patients with intrahepatic cholangiocarcinoma depending on the surgical status: a SEER database analysis. Sci Rep 14, 1568 (2024). https://doi.org/10.1038/s41598-024-52025-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52025-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.