Abstract
To evaluate whether single acetabular column can be reserved and the effect of reconstruction with femoral head plus total hip replacement (THR) for primary malignant peri-acetabulum tumors. From 2007 to 2015, nineteen patients with primary malignant peri-acetabulum tumors were enrolled. All cases underwent single column resection with clear surgical margins. Ten of the 19 tumor’s resections were assisted by computer navigation. Femoral heads were applied to reconstruct anterior or posterior column defects; THR was used for joint reconstruction. The surgical safety, oncologic outcome and prosthesis survivorship and function were evaluated by regular follow-up. The average follow-up period was 65.9 months. Surgical margins contained wide resection in 12 cases and marginal resection in 7 cases. One patient with Ewing's sarcoma died 14 months postoperative due to lung metastasis. One case with chondrosarcoma had recurrence. One prosthesis was removed due to infection. The average MusculoSkeletal Tumor Society (MSTS) function score was 83.7%. Due to the relative small number of cases, there was no significant difference in the recurrence rate and prosthesis failure rate between the navigation group and non-navigation group. Single column resection and reconstruction with femoral head autograft plus THR is an effective, safe method with less complication rate and better functional outcome for patients with peri-acetabular tumors.
Similar content being viewed by others
Introduction
The incidence of pelvic tumor is low which accounts for approximate 4% of all bone tumors1. Due to the complexity of anatomical structure and important organs, the surgical treatment of pelvic tumor is difficult, therefore the intraoperative risk and recurrence rate is high1,2. More complications were found postoperatively2,3,4,5. With the improvement of oncological concepts and surgical techniques, more limb salvage surgeries were performed6,7. Therefore, more attention is paid to functional reconstruction and the control of complications6,7. According to Enneking and Dunham pelvic tumor classification8, tumor resection can usually lead to uncompleted and dysfunctional hip joint. Therefore, effective functional reconstruction is necessary but difficult.
There are several reconstruction methods for acetabulum such as inactivation and replantation9,10, saddle prosthesis11,12, semi pelvic prosthesis13,14, massive allograft15,16, or arthrodesis17. The replantation and pelvic prosthesis were relative common but brought significant complications such as infection, nonunion and fracture with unsatisfactory function18. For malignant pelvic tumors which involved single column, extensive resection can significantly reduce recurrence rate19. But the postoperative complications such as infection and delayed healing affected the postoperative functional recovery19.
Some special malignant pelvic tumor may only affect single column of acetabulum. To the best of our knowledge, there has been no special report on surgical treatment of this kind of tumors. Therefore, we focused on the operability, effect and safety of single column resection and reconstruction on malignant peri-acetabulum tumor. How to decrease the recurrence rate and apply effective reconstruction to bring benefit at the same time is a difficult problem. In recent years, we performed study on the reconstruction of acetabular tumors by strict preoperative planning and precise single column resection with respect to the surgical safety, oncological outcome and prosthesis survivorship and function.
Materials and methods
General characteristic
This was a retrospective case series study. This study was approved by the Ethics Committee of Beijing Ji Shui Tan Hospital (approval no. K201809-32), and informed consent was obtained from all patients. This study adhered to the declaration of Helsinki. All methods were performed in accordance with relevant guidelines and regulations. All cases were from the musculoskeletal tumor database in our department. From 2007 to 2015, nineteen cases were included according to the inclusion criteria: tumors located in the anterior or posterior column of acetabulum (zone II), also involved obturator area (zone III); zone I and IV was not affected by tumor; pathological confirmed primary malignant tumor; weight-bearing or stability was limited and reconstruction was necessary; surgical resection of single column and THR was performed. There were 9 males and 10 females. Mean age was 47.2 (24–64) years. Pathological diagnosis included 16 cases of chondrosarcoma (tumor grade: nine grade 1, six grade 2 and one grade 3), one case of undifferentiated pleomorphic sarcoma (UPS), one cases of Ewing's sarcoma and one case of solitary plasmacytoma. The lesion sites included 17 cases of anterior column and 2 cases of posterior column (Table 1).
Preoperative examinations
All patients underwent clinical examination, laboratory examination, X ray, CT and MRI of pelvis and whole-body bone scan (Fig. 1). Pre-operative needle biopsy was performed for pathological examination. Definitive diagnosis was confirmed by postoperative pathology. The osteotomy line (wide margin) was designed as 1.5-cm margin from the edge of tumor.
Surgical treatment
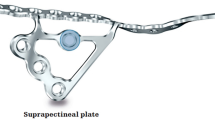
All cases underwent tumor resection performed by experienced senior surgeons. Computer navigation aided surgery was performed in 10 cases. CT and MRI images were fused in navigation system (Stryker Orthomap 3D Navigation System). The accurate three-dimensional model of tumor was showed in workstation of navigation and pre-operative resection planes and margins were designed (Fig. 2). Navigation aided tumor resection was performed intraoperative according to preoperative plan (Figs. 3, 4). After tumor resection, single column of acetabular had obvious bone defect. According to the shape and size of defect, autologous ipsilateral femoral head was shaped. And then it was implanted in the acetabular defect with surfaces of cancellous bone contacted A few long screws were used to fix it. The reconstructed acetabular was then shaped and cemented THR was performed. In addition, according to the site and stability of reconstruction, an acetabular reconstruction cage was used or not. The cage was applied in 12 cases. The postoperative specimen was cut and evaluated (Fig. 3).
The tumor margin and resection plan was designed in navigation system. Tumor range was described as yellow area and the osteotomy planes were designed by virtual planes with different colors. Different cross sections and three-dimensional images showed the resection design (1.5-cm from the edge of the tumor). The anterior column of acetabulum could be resected safely and posterior could be reserved according to the preoperative plan.
The precise single column resection and reconstruction with femoral head plus THR. (A) The bone resection line was marked with the direction of intraoperative navigation. (B) The precise single column resection was then performed. (C) The autologous ipsilateral femoral head was shaped and implanted in the acetabular defect. (D) The cemented THR was performed.
Followed up
Four cases (high grade chondrosarcoma, UPS, Ewing's sarcoma and solitary plasmacytoma) underwent post-operative chemotherapy. All patients were followed every 3 months postoperative (Fig. 5). The X ray and CT of the pelvis, chest CT and bone scan was performed. Postoperative limb function was evaluated with MSTS scoring system20.
Statistical analysis
SPSS 20.0 software was used. The descriptive analysis, mean value t-test, chi square test, Fisher exact probability method and Kaplan Meier method was performed. P < 0.05 was considered as statistically significant.
Result
Surgical result
The average blood loss was 2800 (800–6000) ml and the average operation time was 333 (270–430) minutes. Tumor range and osteotomy line were designed before surgery. There were 12 wide resection, 7 marginal resection (low grade chondrosarcoma) and no intralesional resection. The planned osteotomy lines were obtained in all cases.
Oncological results
The average follow-up period was 65.9 (median 65.5, range 12–149) months. One patient with Ewing's sarcoma died of lung metastasis 14 months postoperative. One patient with chondrosarcoma had recurrence 61 months postoperative and semi-pelvic amputation was performed. The recurrence rate in non-wide margin group and wide margin group was 14.3% (1/7) and 0 (0/12), respectively (p = 0.251). There was no significant difference in the recurrence rate between the navigation group 0 (0/10) and non-navigation group 11.1% (1/9) (p = 0.474).
Prosthesis results
Two prosthesis failures occurred. One case was type IV failure (infection). The patient received arthrodesis 14 months postoperative due to deep infection. No other complication occurred 104 months post-operative. Another patient with type V failure (tumor recurrence) was the recurrent case mentioned above. There was no postoperative prosthesis dislocation and other prosthesis related complications. There was no significant difference in the prosthesis failure rate between the navigation group 0 (0/10) and non-navigation group 22.2% (2/9) (p = 0.211). The 5-year overall prosthesis survival rates were 90.9%. The average survival time was 102.8 (95% confidence interval, 86.1–120.0) months.
There were two minor wound infection: one case recovered after debridement and lavage; another case recovered after conservative treatment. The average MSTS score was 83.7% (25.1, range 17–29). The detailed average scores were as follows: 4.5 (4–5) in pain, 4.2 (2–5) in function, 4.3 (3–5) in emotional acceptance, 4.6 (all were 5 except 1 case needing crutch) in supports, 3.9 (3–5) in walking and 3.6 (2–5) in gait.
Discussion
The wide resection of malignant pelvic tumor is more complex than limb tumor. Extensive exposure, long operation time and massive intraoperative bleeding increase the incidence of postoperative complications. The function of acetabulum structure is important, but large volume of the implant and the stress concentration cause complications21,22. The reconstruction of pelvic ring continuity and hip joint function is difficult. Long-term stable effect is also difficult to obtain9,10,11,12,13,14,15,16,17.
Because some special peri-acetabulum malignant tumor affect single acetabula column, we performed this study to evaluate whether partial acetabulum can be reserved and the effect of single column resection and reconstruction with femoral head plus THR for malignant pelvic tumors. The surgical safety, oncological outcome, prosthesis survivorship and function were analyzed.
Surgical resection of malignant peri-acetabulum tumor is difficult. The risk of operation and postoperative recurrence rate is high. De Paolis et al.23 reported 42 cases with long follow-up. There were 15 recurrences and 16 distant metastases. Deloin et al.24 reported 62 cases of pelvic chondrosarcoma. There were 18 local recurrences and 12 metastases. Surgical margin was significantly associated with recurrence. Poor margin, high tumor grade and acetabular involvement were risk factors of poor prognosis. Previous reports25,26,27,28,29,30,31,32,33,34 showed the recurrence rate of pelvic chondrosarcoma was 18–45% and surgical margin affected local recurrence.
Our study showed one local recurrence with chondrosarcoma after marginal resection. Therefore, the recurrence rate of chondrosarcoma was 6.3% (1/16). The recurrence rate was 14.3% (1/7) in non-wide cases and 0 (0/12) in wide cases. Therefore, the premise of good local control is safe surgical margin and the premise of obtaining a safe margin is accurate preoperative design and precise intraoperative performance. The excessive sacrifice of normal bone can obtain safe margin, but it also brings trouble in the reconstruction and increases perioperative complications.
A number of studies12,35,36,37 on saddle prosthesis showed high complication rates and unacceptable function. These included the destruction of iliac wing, prosthesis moving up, shortened limb length, prosthesis dislocation, wound infection, fracture and heterotopic ossification. Jansen et al.36 reported 17 cases of saddle prosthesis replacement with average MSTS score of 47%. Three patients couldn’t walk and 13 cases needed crutches. Fourteen cases had complications which contained 9 cases of infection and 2 cases of significant limb length discrepancy.
Semi-pelvic prosthesis can provide higher intensity and acceptable function, but the complications are unacceptable. The incidence rate was 75% and the most common was wound problems38,39. Therefore, it requires a careful consideration when selecting this kind of reconstruction. Abudu et al.40 reported 60% incidence of infection and dislocation, and 40% of the prosthesis were removed.
Reconstruction with massive allograft has high risk. Ozaki et al.41 reported 22 cases of allograft reconstruction and allograft was removed in 9 cases due to complications. Langlais et al.15 reported 13 cases with allograft reconstruction and 44% of them presented poor function. Yoshida et al.42 also reported very high incidence of complications in 19 cases.
Given high complication of saddle prosthesis, semi-pelvic prosthesis and massive allograft, some authors recommend arthrodesis17. But some problems also existed, such as activities limitation, limb length discrepancy, fusion failure and poor function43,44,45.
THR has certain advantages in the reconstruction of acetabular. Clayer et al.46 reported 29 cases with THR and only one case showed prosthesis loosening. Harrington et al.47 applied strengthening ring and screw fixation in THR in acetabular metastases. The postoperative results were good with no prosthesis loosening. Piya et al.48 reported 22 cases of metastases which received cement THR with screws fixation and cage was used in most cases. Only one hip dislocation and one superficial infection occured. Ho et al.49 reported THR with auxiliary of cement and screws. There were no prosthesis and cement loosening. Gill et al.50 suggested appling acetabular cup with wing in the reconstruction of acetabulum, the long-term result was similar with normal hip revision if no tumor recurrence.
In order to avoid complications of metal prosthesis, Puget et al.51 reported THR with autograft in the defect of acetabulum. The model had both advantages of prosthesis and autograft. It provided sufficient strength early term and biological healing of autograft long-term. The long-term result was better than pelvis prosthesis and allograft.
Our study showed two prosthesis failures and one was due to tumor recurrence. It suggested the main reason of prosthesis failure was tumor recurrence. Another failure was caused by deep infection. This failure reason is similar to conventional THR. There was no prosthesis dislocation and other prosthesis related complication. Our results showed high 5-year prosthesis survival rate. The mean postoperative MSTS score was 83.7% with acceptable daily activity. All patients could walk and take care of themselves.
Acetabular tumors require accurate resection and reconstruction. Our surgical resection and reconstruction depends on reliable preoperative design. Good local control can be obtained by accurate preoperative design and safe removal of tumor. Computer navigation has an advantage in our practice which contains accurate preoperative design and precise intraoperative real-time guide. The accurate resection and reconstruction can be achieved.
We retained single acetabulum to create condition for stable reconstruction. Autograft was applied to fill bone defect of acetabulum and bone fusion was achieved. Compared with artificial pelvis, saddle prosthesis or allograft bone, autologous biological reconstruction has obvious advantages. It can reduce the risk of infection, non-healing, fracture and prosthesis loosening. Three cases with infection were found in all 19 cases. Only one case underwent prosthesis removal and arthrodesis. The other two prostheses had good long-term results. Few complications and satisficed postoperative results were showed in our study. With the development of 3D printing technology and personalized reconstruction, we can perform comparative study between autologous bone and metal acetabular augment reconstruction in future.
There were some limitations in our study. First, it was not a prospective case control study. Second, the sample size was relatively small. The cases in our study were special that single column was involved by tumor and anterior/posterior column can be reserved. Thus, it’s difficult to find many cases suitable for this special operation. Selection bias may exist in our study and many peri-acetabular pelvic malignant tumors are not suitable for this surgical method. The very low recurrence rate and complications may be also related to selection bias. Third, the follow-up period was relative short and some patients were followed less than five years.
In conclusion, early results showed that single column resection and reconstruction with femoral head autograft plus THR is an effective, safe method with less complication rate and better functional outcome for patients with peri-acetabular tumors Partial acetabulum can be reserved through precise plan of resection and reconstruction. Additional studies comparing this method with alternatives and long-term results are required.
A shorter conference version of this paper was reported in CAOS 2018. The 18th Annual Meeting of the International Society for Computer Assisted Orthopaedic Surgery. This manuscript provides a richer data analysis and discussion of related content.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Unni, K. K. Dahlin’s Bone Tumors: General Aspects and Data on 10165 Cases 6th edn, 5–294 (Lippincott Williams & Wilkins, 2009).
Reguerre, Y. et al. Local therapy is critical in localised pelvic rhabdomyosarcoma: Experience of the International Society of Pediatric Oncology Malignant Mesenchymal Tumor (SIOP-MMT) committee. Eur. J. Cancer 48(13), 2020–2027 (2012).
Delloye, C. et al. Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J. Bone Joint Surg. Am. 89(3), 579–587 (2007).
Mankin, H. J. et al. Malignant tumors of the pelvis: An outcome study. Clin. Orthop. Relat. Res. 425, 212–217 (2004).
Ding, Y. et al. The surgical treatment of primary malignant bone tumors of pelvis. Chin. J. Surg. 46(12), 886–890 (2008).
Erikson, U. & Hjelmstedt, A. Limb-saving radical resection of chondrosarcoma of the pelvis. J. Bone Joint Surg. (Am.) 58, 568–570 (1976).
Steel, H. H. Resection of the hemipelvis for malignant disease: An alternative to hindquarter amputation for periacetabular chondrosarcoma of the pelvis. Semin. Oncol. 8, 222–228 (1981).
Ermeking, W. F. & Dunham, W. K. Resection and reconstruction for primary neoplasms involving the innominate bone. J. Bone Joint Surg. Am. 60, 73l–746 (1978).
Kim, H., Kim, K., Han, I., Oh, J. & Lee, S. The use of pasteurized autologous grafts for periacetabular reconstruction. Clin. Orthop. Relat. Res. 464, 217–223 (2007).
Davidson, A., Hong, A., McCarthy, S. & Stalley, P. En-bloc resection, extracorporeal irradiation, and re-implantation in limb salvage for bony malignancies. J. Bone Joint Surg. (Br.) 87, 851–857 (2005).
Cottias, P., Jeanrot, C., Vinh, T. S., Tomeno, B. & Anract, P. Complications and functional evaluation of 17 saddle prosthesesfor resection of periacetabular tumors. J. Surg. Oncol. 78, 90–100 (2001).
Aljassir, F. et al. Outcome after pelvic sarcoma resection reconstructed with saddle prosthesis. Clin. Orthop. Relat. Res. 438, 36–41 (2005).
Ozaki, T. et al. Implantation of hemipelvic prosthesis after resection of sarcoma. Clin. Orthop. Relat. Res. 396, 197–205 (2002).
Guo, W., Li, D., Tang, X., Yang, Y. & Ji, T. Reconstruction with modular hemipelvic prostheses for periacetabular tumor. Clin. Orthop. Relat. Res. 461, 180–188 (2007).
Langlais, F., Lambotte, J. & Thomazeau, H. Long-term results of hemipelvis reconstruction with allografts. Clin. Orthop. Relat. Res. 388, 178–186 (2001).
Delloye, C., Banse, X., Brichard, B., Docquier, P. & Cornu, O. Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J. Bone Joint Surg. (Am.) 89, 579–587 (2007).
Fuchs, B., O’Connor, M., Kaufman, K., Padgett, D. & Sim, F. Iliofemoral arthrodesis and pseudarthrosis: A long-term functional outcome evaluation. Clin. Orthop. Relat. Res. 397, 29–35 (2002).
Jaiswal, P. et al. Periacetabular resection and endoprosthetic reconstruction for tumours of the acetabulm. J. Bone Joint Surg. (Br.) 90, 1222–1227 (2008).
Zheng, K. et al. Giant cell tumor of the pelvis: A systematic review. Orthop. Surg. 7(2), 102–107 (2015).
Enneking, W. F. et al. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin. Orthop. 286, 241 (1993).
Niu, X. & Xu, W. The challenges and difficult issues on surgical management of malignant pelvic tumors in China. Chin. J. Bone Joint 2(5), 241–243 (2013).
Xu, W. et al. Resection and reconstruction of tumors around the acetabulum. Chin. J. Orthop. 15(12), 805–808 (1995).
De Paolis, M. et al. The use of iliac stem prosthesis for acetabular defects following resections for periacetabular tumors. Sci. World J. 2013, 717031 (2013).
Deloin, X. et al. Pelvic chondrosarcomas: Surgical treatment options. Orthop. Traumatol. Surg. Res. 95, 393–401 (2009).
Ozaki, T., Hillmann, A., Lindner, N., Blasius, S. & Winkelmann, W. Chondrosarcoma of the pelvis. Clin. Orthop. Relat. Res. 337, 226–239 (1997).
Henderson, E. D. & Dahlin, D. C. Chondrosarcoma of bone—A study of two hundred and eighty-eight cases. J. Bone Joint Surg. 45(7), 1450–1458 (1963).
Gitellis, S., Bertoni, F. & Campanacci, M. Chondrosarcoma of bone. The experience at Instituto Orthopedico Rizzoli. J. Bone Joint Surg. 63A, 1248–1262 (1981).
Evans, H. L., Ayala, A. G. & Romsdahl, M. M. Prognostic factor in chondrosarcoma of bone: A clinicopathologic analysis with emphasis on histologic grading. Cancer 40, 818–831 (1977).
Sheth, D. S. et al. Chondrosarcoma of the pelvis. Prognostic factors for 67 patients treated with definitive surgery. Cancer 78(4), 745–750 (1996).
Bergh, P., Gunterberg, B., Meis-Kindblom, J. M. & Kindblom, L. G. Prognostic factors and outcome of pelvic, sacral, and spinal chondrosarcomas: A center-based study of 69 cases. Cancer 91(7), 1201–1212 (2001).
Donati, D., El Ghoneimy, A., Bertoni, F., Di Bella, C. & Mercuri, M. Surgical treatment and outcome of conventional pelvic chondrosarcoma. J. Bone Joint Surg. Br. 87(11), 1527–1530 (2005).
Pring, M. E., Weber, K. L., Unni, K. K. & Sim, F. H. Chondrosarcoma of the pelvis. A review of sixty-four cases. J. Bone Joint Surg. Am. 83-A(11), 16301642 (2001).
Bjornsson, J., McLeod, R. A., Unni, K. K., Ilstrup, D. M. & Pritchard, D. J. Primary chondrosarcoma of long bones and limb girdles. Cancer 83(10), 2105–2119 (1998).
Fiorenza, F. et al. Risk factors for survival and local control in chondrosarcoma of bone. J. Bone Joint Surg. Br. 84(1), 93–99 (2002).
Menendez, L. R., Ahlmann, E. R., Falkinstein, Y. & Allison, D. C. Periacetabular reconstruction with a newendoprosthesis. Clin. Orthop. Relat. Res. 467(11), 2831–2837 (2009).
Jansen, J. A., Van de Sande, M. A. J. & Dijkstra, P. D. S. Poor long-term clinical results of saddle prosthesis after resection of periacetabular tumors. Clin. Orthop. Relat. Res. 471(1), 324–331 (2013).
Cottias, P., Jeanrot, C., Vinh, T. S., Tomeno, B. & Anract, P. Complications and functional evaluation of 17 saddle prostheses for resection of periacetabular tumors. J. Surg. Oncol. 78, 90–100 (2001).
Witte, D. et al. Limb-salvage reconstruction with MUTARS hemipelvicendoprosthesis: A prospective multicenter study. Eur. J. Surg. Oncol. 35, 1318–1325 (2009).
Ji, T., Guo, W., Yang, R. L., Tang, X. D. & Wang, Y. F. Modular hemipelvicendoprosthesis reconstruction—Experience in 100 patients with mid-term follow-up results. Eur. J. Surg. Oncol. 39, 53–60 (2013).
Abudu, A., Grimer, R. J., Cannon, S. R., Carter, S. R. & Sneath, R. S. Reconstruction of the hemipelvis after the excision of malignant tumours. J. Bone Joint Surg. B. 79(5), 773–779 (1997).
Ozaki, T. et al. High complication rates with pelvic allografts. Experience of 22 sarcoma resections. Acta Orthop. Scand. 67(4), 333–838 (1996).
Yoshida, Y., Osaka, S. & Mankin, H. J. Hemipelvic allograft reconstruction after periacetabular bone tumor resection. J. Orthop. Sci. 5(3), 198–204 (2000).
Windhager, R. et al. Limb salvage in periacetabular sarcomas: Review of 21 consecutive cases. Clin. Orthop. Relat. Res. 331, 265–276 (1996).
Campanna, R. et al. Complications of pelvic resections. Arch. Orthop. Trauma Surg. 106, 71–77 (1987).
Davis, A. M., Bell, R. S., Badley, E. M., Yoshida, K. & Williams, J. I. Evaluating functional outcome in patients with lower extremity sarcoma. Clin. Orthop. Relat. Res. 358, 90–100 (1999).
Clayer, M. The survivorship of protrusio cages for metastatic disease involving the acetabulum. Clin. Orthop. Relat. Res. 468, 2980–2984 (2010).
Harrington, K. D. The management of acetabular insufficiency secondary to metastatic malignant disease. J. Bone Joint Surg. Am. 63, 653–664 (1981).
Piya, K. et al. Functional outcome and complications following reconstruction for Harrington class II and III periacetabular metastasis. World J. Surg. Oncol. 13(4), 1–5 (2015).
Ho, L., Ahlmann, E. R. & Menendez, L. R. Modified Harrington reconstruction for advanced periacetabular metastatic disease. J. Surg. Oncol. 101, 170–174 (2010).
Gill, T. J., Sledge, J. B. & Müller, M. E. The Bürch-Schneider anti-protrusio cage in revision total hip arthroplasty: Indications, principles and long-term results. J. Bone Joint Surg. (Br.) 80(6), 946–953 (1998).
Puget, J. & Utheza, G. Reconstruction of the iliac bone using the homolateral femur after resection for pelvic tumor. Orthop. Traumatol. Surg. Res. 100, 43–47 (2014).
Funding
Beijing Hospitals Authority Youth Programme (QML20200403); Beijing Jishuitan Hospital Elite Young Scholar Programme (XKGG202108); Beijing JST Research Funding (ZR-202104).
Author information
Authors and Affiliations
Contributions
Y.Y. and X.N. wrote the main manuscript text. Y.Y. and Y.L. performed the follow up. W.L. performed the statistical analysis. X.N. edited and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Y., Li, Y., Liu, W. et al. Precise single column resection and reconstruction with femoral head plus total hip replacement for primary malignant peri-acetabulum tumors. Sci Rep 14, 3412 (2024). https://doi.org/10.1038/s41598-024-52019-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52019-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.