Abstract
Acetabular defects are a challenging condition for surgeons in revision THA. A crucial aim is an anatomical restoration of the centre of rotation (COR) through grafts. The aim of this study was to determine the cup survival after biological restoration of acetabular defects in THA and the effect of Paprosky classification, age, BMI, and number of previous operations on cup survival. Retrospectively patients with a cup exchange and an impaction of cortico-cancellous or bulk grafts between 2009 and 2012 were included with a follow up with a minimum of 5 year. Implant failure was defined as radiographic loosening or explantation of the cup. The acetabular defect situation was classified to Paprosky. 82 patients (58 female 70.7%) were included. 26 patients were not available to contact. 56 patients (40 female 71.4%) remained for survival analysis with mean age of 75.6 ± 8 years. Survival of the cup after 5 years was 90% and after 7.8 years 88%. There was no difference in survival concerning defect classification, type of implant or graft, age, BMI, and number of previous operations. Patients on the follow up reached an HHS of 67.4 ± 19, a WOMAC Score of 33.4 ± 25.4 points and an unsatisfactory result in the SF-36. Impaction bone grafting of acetabular defects is a good option with satisfactory biomechanical results and survival for small defects. Predictive factors for cup survival could not be clarified in our study. So, the correct indication, knowing the limits of the methods and the correct choice of implant allow a defect-oriented approach and are decisive for the success of the operation.
Similar content being viewed by others
Introduction
Total Hip Arthroplasty (THA) is a common operation with increasing case numbers of primary and revision procedures over the last decades1,2,3. A severe complication after THA requiring revision is loosening of the cup, sometimes associated with a bony defect of the acetabulum and migration of the cup. A crucial aim of primary THA and revision surgery is an anatomical restoration of the centre of rotation (COR)4. Primary and secondary defects of the acetabulum can lead to a non-anatomical positioning of the cup with a potential higher rate of failure, while an anatomical biomechanical position of the cup increases longevity and decreases stress4,5. Slooff et al. described in the 1980s a technique of impaction bone grafting (IBG) for restoring the anatomical COR with bone grafts for a biological reconstruction with good short- and long-term survival6,7,8.
While using a biological graft for restoring the COR and establishing a new bony bed for the cup is advantageous, resorption, cup migration and a lesser primary stability in some cases are serious limitations of this technique. So metallic support like the Trabecular-Metal-Technology (Fa. Zimmer) was developed to reach a better primary stability with the disadvantage of implanting another foreign body, which can lead to an even greater bone defect in potential following revisions9,10,11.
Also, the type of biological grafts seems to play a significant role. Allogenic cortico-cancellous chips showed an incorporation through endochondral ossification and thus biological closure of the defect12,13. A primary mechanical stability is achieved by impacting and using cortico-cancellous chips. Studies using impacted bone chips and cementless cups for the reconstruction of moderate defects show satisfactory results with survival rates of over 90% after more than 10 years14,15. There is consensus that hemispherical press-fit cups should only be used if the cup circumference is intact and that there should be at least 50% contact surface with the recipient's vital bone16. But there is a lack of knowledge about the influencing factors for cup survival to make general recommendations. Another application form of allogenic bone grafting are bulk or solid allografts. They are used for large cavitary and segmental defects up to pelvic discontinuity17,18,19. The bone incorporation in bulk allografts takes place only partially in the revascularized edge zone of the transplant. Inadequate angiogenesis and the risk of resorption of the allograft are often seen as a limitation of their long-term stability and their use is therefore generally controversial20.
The aim of this study was (1) to determine the cup survival after biological restoration of acetabular defects in THA after a minimum follow-up of 5 years, (2) to evaluate the effect of the defect classification of Paprosky on the cup survival and to analyse the influence of age, Body-Mass-Index (BMI) and number of previous operations on cup survival and (3) to compare the Short-Form-36 health questionnaire (SF-36), Harris-Hip-Score and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC-Score) after a minimum follow up of 5 years.
Patients and methods
We retrospectively included all cases with previous THA and a planned cup exchange because of aseptic and septic loosening and an allogenic cortico-cancellous or bulk bone graft from our own bone bank between 2009 and 2012 (Fig. 1). Patients with an additional trabecular metal implant or cancellous bone grafts only were excluded. A minimal follow up of 5 years was determined. Patients were invited for a follow-up investigation with conventional a.p. and axial radiograph of the hip, clinical examination, SF-36-Score, HHS and WOMAC-Score. Patients refusing the invitation were interviewed by telephone. Therapy failure of cup survival was defined as radiographic loosening or explantation of the cup. The acetabular defect situation was determined on conventional a.p. radiographs of the hip to Paprosky classification21. Cup loosening was defined by a circumferent radiolucent line, cup migration and broken fixation screws22,23,24. The standardized Questionnaires were compared to a normal and age adjusted population.
The operation was done in lateral decubitus. The cup type and size were determined by a cup trial and subsequently a customized femoral head allograft from our own bone bank was used to minimize the defect in impaction graft technique. For small defects bone was prepared into small cortico-cancellous pieces of 5 to 8 mm. For greater defects (Paprosky > IIc) the bone was prepared into a bulk. Both were rinsed with a jet lavage with saline to wash out fatty remnants and rinsed with an antibiotic solution with gentamicin. The bone graft was impacted with cup trials and special impactors and subsequently the endoprosthetic treatment was completed. All patients received a perioperative antibiotic single shot and an additional shot if the operation time was longer than 2 h. In case of septic loosening the patients got a germ adapted antibiotic treatment over 12 weeks after operation. After operation the patient had a restrictive physiotherapeutic exercise program with a limited weight bearing of 20 kg or sole contact for 6 weeks. After 6 weeks an X-ray control was done and a gradually increase of weight bearing was started with additional 20 kg every 2 weeks for 6 weeks. After the next X-ray control the limitation of the weight bearing was ended and the crutched were trained off.
The study was approved by the independent ethics committee of the authors’ affiliated institution (IRB NO. 5283-09/2017) and informed consent was obtained from all participants. All procedures being performed were part of the routine care and in accordance with relevant guidelines and regulations.
Statistical analyses
Statistical analysis was performed with the statistics program SPSS (Version 25, IBM). As an analytical approach a student’s t-test was performed for parametric tests of two samples and Log-Rank-test was performed for analysing the influence of confounders. The level of significance was p < 0.05. Investigating the survival of the implant a Kaplan–Meier-Analysis generally and regarding to the defect classification, age, BMI, and number of previous operations was performed.
Ethics approval
Ethical approval was done by the local Ethics Committee of University Jena in view of the retrospective nature of the study. All the procedures being performed were part of the routine care (Reg.-Nr. 5283-09/2017).
Results
We included retrospective 82 patients (24 male 29.3%, 58 female 70.7%) with an acetabular bone defect treated with an allogenic bone graft and a new cup. 26 patients were not available to contact for final follow up (Fig. 1). So, 56 patients (40 female 71.4%, 16 male 38.6%) remained for final survival analysis and 17 patients completed the questionnaires for analysing the patient’s outcome.
Demographic data
Mean age of the 82 patients at the index operation was 70.3 ± 9 years. Mean age of the 56 patients on follow up was 75.6 ± 8 years. Mean BMI at the index operation was 28 ± 4.8 kg/m2, while 30.5% had normal weight, 36.6% had overweight, 26.8% had obesity WHO I°, 3.7% WHO II° and 2.4% WHO III° (Table 1). All patients had a previous operation of the hip, 22.6% had two, 6.8% three, 3.4% four and 1.1% five previous operations (Fig. 2).
Operation data
Indication for index revision surgery was aseptic loosening (81.6%), aseptic loosening in presence of osteolysis by wearing of the PE-inlay (8%), periprosthetic fractures (4.6%) and septic loosening (5.8%). Femoral head allografts from our bone bank were used in all cases. 25 patients (44.8%) had a solid structured bulk graft, 18 (32.2%) cortico-cancellous bone chips and 13 (23%) were treated with a combination of bulk and cortico-cancellous bone grafts. Implants used for endoprosthetic treatment were shown in Fig. 3 and depending on the Paprosky defect type in Fig. 4. Bone defects were classified after Paprosky at the preoperative a.p. radiographs with an occurrence of type 2a in 23.5%, type 2b 27.1%, type 2c 21.2%, 3a 20% and type 3b 8.2%, respectively.
Implant survival
46 of 56 patients had no further operation (82%). 10 patients (18%) had complications after the cup exchange and bone grafting while some occurred in the same patient: 6 aseptic cup loosening (2 press fit cups, 2 jumbo cups, 2 revision cages), 4 periprosthetic infections, 2 recurrent dislocation, 1 periprosthetic fracture and 1 major limb amputation of the thigh on both sides.
-
(1)
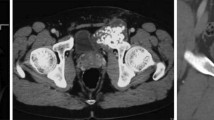
Defining aseptic loosening and periprosthetic fracture as failure of the bone graft, there is a revision free survival after 5 years of 90% and after 7.8 years of 88% (Figs. 5, 6). Figures 7, 8 and 9 show two successfull and one unsuccessfull bone graft reconstruction of acetabular defects (Figs. 7, 8, 9).
-
(2)
Furthermore, there was no significant difference in survival concerning defect classification (p = 0.853), type of implant (p = 0.882) or graft (p = 0.958), age (p = 0.456), BMI (p = 0.910), and number of previous operations (p = 0.517). As well spearman-rho correlation analysis showed no significant correlation between these factors and aseptic loosening. Periprosthetic infection (n = 4) occurred only in bulk grafts in our study group and 5 out of 6 aseptic loosening occurred within the first 2 years.
Follow up data
-
(3)
Patients on the follow up reached an HHS of 67.4 ± 19 points (of 100 points). Subdivided in pain and functional score our patients had 30.4 ± 11.4 (of 44) points regarding on pain and 29.8 ± 11.6 (of 47) points regarding on function.
On WOMAC Score they reached 33.4 ± 25.4 points. Subdivided into pain, stiffness and restrictions of everyday activity patients reached 22.5 ± 25.6 points for pain, 35.0 ± 28.4 points for stiffness and 36.4 ± 27.9 points for restrictions of everyday activity while less points mean a better outcome.
Table 2 shows the subdivided results of the SF-36 from our patients compared to a German normal and age-adjusted baseline population.
Discussion
Reconstruction of large acetabular defects in revision hip arthroplasties continues to constitute a great challenge. Surgical options include next to bone grafts, extra-large hemispheric cups25, reconstruction cages26 and more recent techniques like trabecular metal implants and augments9. Bone impaction grafting of the acetabulum had been advocated as an excellent method for reconstructing acetabular defects and for restoration acetabular bone stock and anatomical COR with good long-term survival19,27. But there is still a controversy which technique to use respective to the defect size.
-
(2)
Our results showed no dependence between survival and defect classification as well as type of implant or graft, age, BMI, and number of previous operations. Furthermore, reconstruction with bulk grafts showed no increased failure than cortico-cancellous grafts. Even reconstruction cages showed no increased failure than cemented or cementless cups in our study. Also, Patel et al. reported no single factor influencing the cup survival, although type III defects showed a higher migration rate of the cup28. But there is still a lack of knowledge about influencing factors to implant survival due to small case numbers and individual surgical strategies.
-
(1)
Our study confirmed that an allogenic bone reconstruction of the acetabulum can lead to satisfactory biomechanical results. We showed a survival in Kaplan-Meyer-analyses of 88% for aseptic loosening after 7.8 years with allogenic acetabular impaction grafting and subsequent implantation of cups and reconstruction cages without significant differences in-between the specific implants. Concerning reconstruction cages, we confirmed the results of Perka et al. who reported a survival rate of 88.8% after 10 years for Paprosky type IIa-IIIb defects treated with Burch-Schneider cages29. Concerning jumbo or extra-large cups Roth et al. also reported survival rates of 85% after 20 years30. An important disadvantage of jumbo cups is the elevation of the hip centre of rotation which can sometimes be handled with a head enlargement31. For bulk allografts a survival of 56% after 4 years20 and 39% after 16.5 years with cemented cups was reported32. For bulk allografts with uncemented cups Paprosky et al. reported a survival of 80% after 10 years for Paprosky type IIIa defects21. Bulk allografts with reconstruction cages showed a survival of 84 to 98%33,34,35,36 in follow up studies between 5 and 19 years, confirming our results with a survivor of 88% (p = 0.958).
Next to extra-large cups and reconstruction cage, trabecular metal implants enjoy increasing popularity37. First studies showed an excellent survival rate > 90% for Paprosky type IIa–IIIb defects after 5 and 10 years10,38,39. The disadvantage of trabecular metal augments is a missing bony replenishment of the defect. In case of potential revision surgery, a larger defect can occur after explanting the metal augment. Furthermore, there is less known about the effect of the potential wearing of the trabecular metal augments. Elevated level of metal particles in the periprosthetic soft tissue and blood samples are reported after aseptic loosening and revision surgery40,41,42. But recent studies showed that especially for larger defects (Paprosky IIIa, b) trabecular metal augments show a good outcome and could be recommend11,43. Furthermore, Shen et al. showed in a meta-analysis no difference in survival of trabecular metal and non-trabecular metal cups in acetabular revision surgery overall, but with a lower incidence of aseptic loosening and infection and a higher incidence of dislocation for trabecular metal compared to non-trabecular metal cups11. Finally, a comparison between the studies remains difficult because of the use of different defect classification and implants, surgical experiences as well as small sample numbers (Table 3).
Table 3 Review of cup survival in literature. -
(3)
Our study population showed a poor functionality with an HHS of 67.4 points. Regis et al. and Wedemeyer et al. reported better functional outcomes (HHS > 75 points) in their studies with comparable defects after 7 and 10 years35,44. But their patients had a lower average age of 65 years in comparison to 70.3 years in our study. In our study there was no correlation between functional outcome measured in HHS and defect size (p = 0.745)45. Concerning the WOMAC- and SF-36-Score Sembrano et al. confirmed our results of 33 points in WOMAC and 65 points in psychological and 48 points in functional SF-36-score46.
Limitations of the study were the small number of cases with several types of cups or cages and a variability in patients’ condition without a control group in a retrospective study design and a mid-term follow up of only 7.8 years. Another limitation was the classification in Paprosky defect type through the pre-operative X-ray. Further intraoperative damage on the acetabulum was not verified. Furthermore, comparison remains difficult because of different defect classification and implants, small case numbers and the surgeons experience. As well the missing preoperative functional score and baseline characteristics of the joint function without drawing the course of the score and joint characteristics pre- and postoperatively is a limitation.
Conclusion
In conclusion bone grafting of acetabular defects for reconstruction of the COR is a validated and a good option with satisfactory biomechanical results and a good survival, especially in smaller acetabular defects. There could be no predictive factors for cup survival clarified in our study group. Neither pre-existing operation, defect classification nor implant model showed a significant influence on survival or outcome. In the end the correct indication, knowing the limits of the methods and the correct choice of implant allow a defect-oriented approach and are decisive for the success of the operation.
References
Grimberg, A. et al. EPRD-Jahresbericht 2020 (EPRD Deutsche Endoprothesenregister, 2020).
Pivec, R., Johnson, A. J., Mears, S. C. & Mont, M. A. Hip arthroplasty. Lancet 380, 1768–1777 (2012).
Statistisches Bundesamt. Fallpauschalenbezogene Krankenhausstatistik (DRG-Statistik) Operationen und Prozeduren der vollstationären Patientinnen und Patienten in Krankenhäusern (4-Steller)—2019 (Statistisches Bundesamt, 2019).
Watts, C. D., Abdel, M. P., Hanssen, A. D. & Pagnano, M. W. Anatomic hip center decreases aseptic loosening rates after total hip arthroplasty with cement in patients with crowe type-II dysplasia: A concise follow-up report at a mean of 36 years. J. Bone Jt. Surg. Am. 98, 910–915 (2016).
Kaku, N., Tabata, T. & Tsumura, H. Influence of cup-center-edge angle on micro-motion at the interface between the cup and host bone in cementless total hip arthroplasty: Three-dimensional finite element analysis. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 25, 1271–1277 (2015).
Slooff, T. J. et al. Acetabular and femoral reconstruction with impacted graft and cement. Clin. Orthop. Relat. Res. 324, 108–115 (1996).
Abdelnasser, M. K. et al. Post-operative hip centre restoration and migration after impaction bone grafting in revision and complex primary hip arthroplasty. Eur. J. Orthop. Surg. Traumatol. 29, 1411–1417 (2019).
Schreurs, B. W., Slooff, T. J., Buma, P. & Verdonschot, N. Basic science of bone impaction grafting. Instr. Course Lect. 50, 211–220 (2001).
Gill, K., Wilson, M. J., Whitehouse, S. L. & Timperley, A. J. Results using Trabecular Metal™ augments in combination with acetabular impaction bone grafting in deficient acetabula. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 23, 522–528 (2013).
Löchel, J., Janz, V., Hipfl, C., Perka, C. & Wassilew, G. I. Reconstruction of acetabular defects with porous tantalum shells and augments in revision total hip arthroplasty at ten-year follow-up. Bone Jt. J. 101-B, 311–316 (2019).
Shen, X., Qin, Y., Li, Y., Tang, X. & Xiao, J. Trabecular metal versus non-trabecular metal acetabular components for acetabular revision surgery: A systematic review and meta-analysis. Int. J. Surg. (London, England) 100, 106597 (2022).
van der Donk, S., Buma, P., Slooff, T. J. J. H., Gardeniers, J. W. M. & Schreurs, B. W. Incorporation of morselized bone grafts: A study of 24 acetabular biopsy specimens. Clin. Orthop. Relat. Res. 396, 131–141 (2002).
Buma, P. et al. Impacted graft incorporation after cemented acetabular revision. Histological evaluation in 8 patients. Acta Orthop. Scand. 67, 536–540 (1996).
Della Valle, C. J., Berger, R. A., Rosenberg, A. G. & Galante, J. O. Cementless acetabular reconstruction in revision total hip arthroplasty. Clin. Orthop. Relat. Res. 420, 96–100 (2004).
Jones, C. P. & Lachiewicz, P. F. Factors influencing the longer-term survival of uncemented acetabular components used in total hip revisions. J. Bone Jt. Surg. Am. 86, 342–347 (2004).
Bader, R. et al. Revisionsendoprothetik der Hüftpfanne (Springer, 2008).
van Haaren, E. H., Heyligers, I. C., Alexander, F. G. M. & Wuisman, P. I. J. M. High rate of failure of impaction grafting in large acetabular defects. J. Bone Jt. Surg. Br. 89, 296–300 (2007).
Marx, A., Beier, A., Richter, A., Lohmann, C. H. & Halder, A. M. Major acetabular defects treated with the Burch–Schneider antiprotrusion cage and impaction bone allograft in a large series: A 5- to 7-year follow-up study. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 26, 585–590 (2016).
Garcia-Cimbrelo, E., Cruz-Pardos, A., Garcia-Rey, E. & Ortega-Chamarro, J. The survival and fate of acetabular reconstruction with impaction grafting for large defects. Clin. Orthop. Relat. Res.® 468, 3304–3313 (2010).
Hooten, J. P., Engh, C. A., Heekin, R. D. & Vinh, T. N. Structural bulk allografts in acetabular reconstruction. Analysis of two grafts retrieved at post-mortem. J. Bone Jt. Surg. Br. 78, 270–275 (1996).
Paprosky, W. G., Perona, P. G. & Lawrence, J. M. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J. Arthroplast. 9, 33–44 (1994).
DeLee, J. G. & Charnley, J. Radiological demarcation of cemented sockets in total hip replacement. Clin. Orthop. Relat. Res. 121, 20–32 (1976).
Hooten, J. P. & Engh, C. A. Failure of structural acetabular allografts in cementless revision hip arthroplasty. J. Bone Jt. Surg. Br. 76, 419–422 (1994).
Johnston, R. C. et al. Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J. Bone Jt. Surg. Am. 72, 161–168 (1990).
Whaley, A. L., Berry, D. J. & Harmsen, W. S. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J. Bone Jt. Surg. Am. 83, 1352–1357 (2001).
Gross, A. E., Wong, P. & Saleh, K. J. Grafts and cages: Managing massive bone loss. Orthopedics 23, 973–974 (2000).
Schreurs, B. W. et al. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented acetabular component: A 20- to 25-year follow-up. J. Bone Jt. Surg. Br. 91, 1148–1153 (2009).
Patel, S., Sukeik, M. & Haddad, F. S. Initial implant stability predicts migration but not failure in cementless acetabular revision with bone grafting. J. Arthroplast. 28, 832–837 (2013).
Perka, C. & Ludwig, R. Reconstruction of segmental defects during revision procedures of the acetabulum with the Burch–Schneider anti-protrusio cage. J. Arthroplast. 16, 568–574 (2001).
von Roth, P., Abdel, M. P., Harmsen, W. S. & Berry, D. J. Uncemented jumbo cups for revision total hip arthroplasty: A concise follow-up, at a mean of 20 years, of a previous report. J. Bone Jt. Surg. Am. 97, 284–287 (2015).
Nwankwo, C. D. & Ries, M. D. Do jumbo cups cause hip center elevation in revision THA? A radiographic evaluation. Clin. Orthop. Relat. Res.® 472, 2793–2798 (2014).
Shinar, A. A. & Harris, W. H. Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J. Bone Jt. Surg. Am. 79, 159–168 (1997).
Schlegel, U. J. et al. Mueller reinforcement rings in acetabular revision: Outcome in 164 hips followed for 2–17 years. Acta Orthop. 77, 234–241 (2006).
Gerber, A., Pisan, M., Zurakowski, D. & Isler, B. Ganz reinforcement ring for reconstruction of acetabular defects in revision total hip arthroplasty. J. Bone Jt. Surg. Am. 85, 2358–2364 (2003).
Regis, D., Magnan, B., Sandri, A. & Bartolozzi, P. Long-term results of anti-protrusion cage and massive allografts for the management of periprosthetic acetabular bone loss. J. Arthroplast. 23, 826–832 (2008).
Regis, D., Sandri, A. & Bonetti, I. Acetabular reconstruction with the Burch–Schneider antiprotrusio cage and bulk allografts: Minimum 10-year follow-up results. Biomed. Res. Int. 2014, 194076 (2014).
Torre-Escuredo, B., Gómez-García, E., Álvarez-Villar, S., Bujan, J. & Ortega, M. A. Bone impaction grafting with trabecular metal augments in large defects in young patients: Unravelling a new perspective in surgical technique. BMC Musculoskelet. Disord. 21, 1–8 (2020).
Jenkins, D. R., Odland, A. N., Sierra, R. J., Hanssen, A. D. & Lewallen, D. G. Minimum 5-year outcomes with porous tantalum acetabular cup and augment construct in complex revision total hip arthroplasty. J. Bone Jt. Surg. Am. 99, e49 (2017).
Whitehouse, M. R., Masri, B. A., Duncan, C. P. & Garbuz, D. S. Continued good results with modular trabecular metal augments for acetabular defects in hip arthroplasty at 7 to 11 years. Clin. Orthop. Relat. Res.® 473, 521–527 (2015).
Babis, G. C., Stavropoulos, N. A., Sasalos, G., Ochsenkuehn-Petropoulou, M. & Megas, P. Metallosis and elevated serum levels of tantalum following failed revision hip arthroplasty—A case report. Acta Orthop. 85, 677–680 (2014).
Sanchez Marquez, J. M., Del Sel, N., Leali, A. & Della González Valle, A. Case reports: Tantalum debris dispersion during revision of a tibial component for TKA. Clin. Orthop Relat. Res.® 467, 1107–1110 (2009).
Schoon, J. et al. Multi-elemental nanoparticle exposure after tantalum component failure in hip arthroplasty: In-depth analysis of a single case. Nanomed. Nanotechnol. Biol. Med. 13, 2415–2423 (2017).
Russell, S. P. et al. Trabecular metal augments for severe acetabular defects in revision hip arthroplasty: A long-term follow-up. J. Arthroplast. 36, 1740–1745 (2021).
Wedemeyer, C. et al. Strukturelle Femurkopfallografts in der Revisionschirugie von gelockerten Hüftendoprothesenpfannen. Unfallchirurg 110, 104–110 (2007).
Duarte, G. M. H., Pires, R. E., Machado, C. J. & Andrade, M. A. P. Reconstruction of acetabular defects with impaction grafting in primary cemented total hip arthroplasty produces favorable results: Clinical and radiographic outcomes over 6.4 years on average. J. Arthroplast. 36, 200–209 (2021).
Sembrano, J. N. & Cheng, E. Y. Acetabular cage survival and analysis of factors related to failure. Clin. Orthop. Relat. Res.® 466, 1657–1665 (2008).
Winter, E. et al. Allogeneic cancellous bone graft and a Burch-Schneider ring for acetabular reconstruction in revision hip arthroplasty. J. Bone Jt. Surg. Am. 83(6), 862–867. https://doi.org/10.2106/00004623-200106000-00007 (2001).
Wachtl, S. W. et al. The Burch-Schneider antiprotrusio cage in acetabular revision surgery: a mean follow-up of 12 years. J. Arthroplast. 15(8), 959–963. https://doi.org/10.1054/arth.2000.17942 (2000).
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by N.D., S.B. and E.R. The first draft of the manuscript was written by S.R. and S.B. and corrected by G.M. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rohe, S., Dörr, N., Böhle, S. et al. Mid-term results in revision hip arthroplasty with impaction bone grafted cup reconstruction for acetabular defects. Sci Rep 12, 13322 (2022). https://doi.org/10.1038/s41598-022-17526-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17526-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.