Abstract
Enteral nutrition (EN) is important for critically ill patients. This study investigated the current situation of EN treatment in SHANGHAI intensive care units (ICUs). We hypothesized that improving EN practice in SHANGHAI may benefit the prognosis of ICU patients. Clinical information on EN use was collected using clinic information forms in 2019. The collected data included the patient’s general clinical information, EN prescription status, EN tolerance status, and clinical outcomes. The observation time points were days 1, 3, and 7 after starting EN. A total of 491 patients were included. The proportion of EN intolerance (defined as < 20 kcal/kg/day) decreased, with rates of intolerance of 100%, 82.07%, 70.61%, and 52.23% at 1, 3, 7, and 14 days, respectively. Age, mNutric score, and protein intake < 0.5 g/kg/day on day 7 were risk factors for 28-day mortality.The EN tolerance on day 7 and protein intake > 0.5 g/kg/day on day 3 or day 7 might affect the 28-day mortality. Risk factors with EN tolerance on day 7 by logistic regression showed that the AGI grade on day 1 was a major factor against EN tolerance. The proportion of EN tolerance in SHANGHAI ICU patients was low. Achieving tolerance on day 7 after the start of EN is a protective factor for 28-day survival. Improving EN tolerance and protein intake maybe beneficial for ICU patients.
Similar content being viewed by others
Introduction
Enteral nutrition (EN) is the preferred nutrition route for critically ill patients and is widely adopted in intensive care units (ICUs)1. Still, many problems remain regarding the safety and effective application of EN, among which EN intolerance is one of the most important. EN intolerance is associated with prolonged hospital stays and increased mortality2,3,4. The European Critical Care Association and the Asia Society for Emergency and Critical Care Medicine recommended that the caloric supply reached 20 kcal/kg/day within 72 h from the start of EN as an objective standard of EN intolerance5, 6. “If the patient can use EN safely, then the patient will be saved”7. Therefore, ensuring the effectiveness and safety of EN is an important issue in clinical practice8.
The underfeeding of EN in China has been reported. In 2017, Li et al9. carried out a national nutrition survey covering 116 ICUs with a total of 1900 patients and showed that 60% of patients met the target on the 5–7th day. This results strongly indicated a high rate of EN intolerance in the ICUs across mainland China.Meanwhile, It should be noted that there are significant differences in the medical resources among different regions in China, which may lead to different treatment preferences in ICU nutrition support. Therefore, we conducted this investigation on the implementation of EN in SHANGHAI, especially on the characteristics of EN intolerance. We hope it will be helpful for making further efforts on improving EN application.
Materials and methods
Study design
This observational study included consecutive patients from the ICUs of 15 hospitals in SHANGHAI admitted from January to December 2019. The clinical data were collected according to the designed case report form. This study was approved by the Ethics Committee of our Hospital. As the major purpose is to the relation between EN tolerance and survival in ICU, this is made in a perspective way.
Study population
Inclusion criteria
-
(1) Patients admitted to the ICU of 15 hospitals who consented and agreed to participate in this research.
-
(2) Patients aged > 18 years.
Exclusion criteria
-
(1)
Patients aged > 90 years.
-
(2)
ICU stay < 72 h.
-
(3)
Patients with absolute contraindications to EN, such as uncontrolled high-flow gastrointestinal fistula, unresolved intestinal obstruction, etc.
-
(4)
Patients with uncontrolled malignancy or end-stage chronic organ failure (heart, lung, liver, kidney, etc.)
Data collection
The patient’s information was recorded in a case information sheet that included:
-
(1)
Nutritional risk assessment: NRS2002 score and mNutric score on ICU admission.
-
(2)
Nutrition prescription (days 1, 3, 7, and 14 after ICU admission): the actual calorie of EN and parenteral nutrition (PN), the amount of protein and amino acid.
-
(3)
Data related to EN tolerance (days 1, 3, 7, and 14 after ICU admission): actual calorie and protein intake, AGI score, and gastrointestinal symptoms. EN tolerance was defined as the caloric supply of the patient reaching 20 kcal/kg/day within 72 h from the start of EN5, 6. The symptoms of FI defined according to the judgement of ICU physician or ESICM Working Group on Abdominal Problems5.
-
(4)
Patients’ outcomes: 28-day mortality and in-ICU mortality.
As for ICU patients who were transferred out earlier than the time point, the laboratory indicators, AGI grade, the amount of calories and protein, organ support, and other items at the time point were analyzed according to the data on the day of transfer.
Statistical analysis
All data were tested for normal distribution. The continuous data not conforming to the normal distribution were expressed as median (interquartile range, IQR). Nonparametric tests were used to compare the two groups. The categorical variables were described as n (%) and analyzed using the chi-square test or Fisher’s exact test. Univariable logistic regression was used for risk factor screening; variables with P-values < 0.05 were included in the multivariable logistic regression for further validation. The survival analysis was performed using the Kaplan–Meier method, and the curves were compared using the log-rank test. COX regression also used for survival. SPSS 22.0 (IBM Corp.) was used for statistical analysis in this study. Two-sided P-values < 0.05 were considered statistically significant. The Cochran–Armitage Trend Test was conducted to test the trend in categorical variables. Jonckheere–Terpstra test is used to determine whether two or more independent samples are derived from the same distribution. The Mantel–Haenszel Test is used to analyze the association between two categorical variables, taking into account the influence of one or more stratified variables.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Ruijin Hospital of Shanghai Jiaotong University School of Medicine, China (Project identification code 2017-78, protocol code 1.0, and date of approval 2017-3-30). All participants provided written informed consent for participation in this study. I confirm that all methods were performed in accordance with the relevant guidelines. All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Results
Baseline data of patients
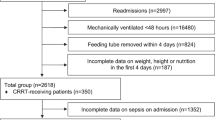
A total of 15 ICUs in SHANGHAI participated in this study, and 491 patients were finally included in the analysis. The flowchart about inclusion and exclusion was in Fig. 1. The basic information of all the patients was shown in (Table 1).
Nutrition implementation on days 1, 3, 7, and 14 of ICU stay
The data on the nutrition therapy on days 1, 3, 7, and 14 of ICU admission of the participants are shown in Table 2. The incidence of intolerance symptoms decreased on the 1st, 3rd, 7th, and 14th days of ICU admission (Table 2).
Comparison of EN implementation in ICU patients with different prognoses
Univariable regression analyses were carried out with 28-day mortality as the outcome. Age, admission mNutric score, ICU APACHE II score, ICU SOFA score, whether calorie intake reached 20 kcal/kg/day on days 3 and 7, whether protein intake reached 0.5 g/kg/day (the median total protein intake) on days 7 is associated with the outcome on day 28 (Table S1). Multivariable logistic regression was performed on the above parameters, and the results showed that age, mNutric score on admission, and protein intake < 0.5 g/kg/day on day 7 were independent risk factors for 28-day mortality. (Table S1).
The effect of EN intake on the survival of ICU patients
Taking the 28-day survival status as the endpoint, the comparison between EN reached 20 kcal/kg/day on day 3 was listed (Table S2). The survival rate was no significant difference. However, Kaplan–Meier survival analyses were performed on whether calories reached 20 kcal/kg/day on day 3 (Fig. 2A or day 7 (Fig. 2B) of ICU admission. The results showed that the survival curve of patients with EN tolerance on day 7 of ICU admission was better than in patients with intolerance (P = 0.01), while there were no differences on day 3 (P = 0.2). The Cox regression shows the same patten: Day 3 p = 0.09, HR 0.83 95% CI (0.67,1.03), Day 7 p = 0.04, HR 0.82 95% CI (0.75,0.98). We adjusted age and ApacheII score in COX regression model.
Kaplan–Meier survival analysis of the patient’s 28-day mortality on whether calories reached 20 kcal/kg/day (A) on day 3 (χ2 = 5.59, P = 0.2) or (B) on day 7 (χ2 = 13.09, P = 0.010); (C) whether the protein reached 0.5 g/kg/day on day 3 (χ2 = 13.99, P < 0.010) or (D) on day 7 (χ2 = 14.27, P < 0.010).
The effect of protein intake on the survival of ICU patients
Using the 28-day survival status as the endpoint, the comparison between whether the protein reached 0.5 g/kg/day on day 3 on day 3 or not was listed (Table S2). The survival rate was no significant difference. Kaplan–Meier survival analyses were performed on whether the protein reached 0.5 g/kg/day on day 3 (Fig. 2C) and day 7 (Fig. 2D) of ICU admission. The results showed that the survival curve of patients whose protein intake reached 0.5 g/kg/day on days 3 and 7 was better than those who did not reach 0.5 g/kg/day (Day3 P < 0.01, Day 7 P < 0.01). The Cox regression shows the same patten: Day3 p = 0.04, HR 0.80 95% CI (0.65, 1.00); Day 7 p < 0.01, HR 0.75 95% CI (0.65, 0.92). We adjusted age and ApacheII score in COX regression model.
Influencing factors of EN intake in ICU patients on day 7
The factors that might influence EN tolerance were included in a logistic regression to analyze EN tolerance in ICU patients on day 7. Preliminary analysis by univariable logistic regression showed that the AGI grade on day 1 (OR = 0.53), the use of organ support on day 3 (OR = 1.80), and the subjective judgment of the physician on EN tolerance on day 3 (OR = 2.96) were statistically significant. We take those factors above (they are with statistically significant in univariable regression) to making multivariable logistic regression, it was found that the AGI grade on day 1 (OR = 0.46) and the use of any organ support on day 3 (OR = 2.08) had a significant impact on EN tolerance in critically ill patients on day 7 (Table 3).
Discussion
In this study, we collected clinical information in critically ill patients admitted to the ICUs in 15 hospitals in SHANGHAI. Our data suggest that enteral nutrition tolerance and adequate protein intake are important for improving survival in ICU patients, as we hypothesized.
Nutritional assessment
Nutritional status and risk of malnutrition should be assessed first before nutritional treatment. Heyland7 And Jie8 conducted prospective non-randomized studies that showed that patients with high malnutrition risk were more likely to benefit from early EN. The NRS2002 and Nutric assessments are the most recommended assessment methods. It is necessary to emphasize that there are still controversies regarding the best tool for assessing the malnutrition risk6.Therefore, further research is needed to find more reasonable ways to evaluate the nutritional status of critical patients.
Use of PN
In this study, 59.47% of the patients started PN at ICU admission, while 43.58% on day 3 and 38.69% on day 7. These results agree with Xing et al.9, suggesting that PN was started earlier in ICU patients in China. It is currently believed that PN should be the rescue remedy for EN. Nevertheless, compared with EN, the implementation and monitoring of PN is relatively simple, and it is easy to achieve the nutritional goals, which fits the situation of insufficient ICU resources in China10. The NUTRIREA-2 study showed11 that patients with full PN developed significantly fewer gastrointestinal symptoms, and PN did not increase the mortality rate and incidence of nosocomial infection.
Calories and protein target setting and EN tolerance
Indirect calorimetry (IC) is considered the gold standard for calorie target setting in the ICU so as to prevent underfeeding and overfeeding12,13,14. In this study, the target calorie and protein were mainly calculated according to the guidelines, accounting for 56.82% of the cases. This is reasonable to use a metabolic formula since none of the centers in this study is equipped with IC. The recommendations for calculating target energy differ between guidelines15, 16. According to the ASPEN recommendation, the target calorie in our population was estimated to be 1350–1650 kcal/kg/day (the median weight was 65 kg), similar to the target calorie set by clinicians in the actual practice.
In this study, patients reaching 20 kcal/kg/day on day 3 did not show benefit on survival. Several studies12, 17,18,19 reported a higher need for organ support in full-energy supply patients than in underfed patients. The time of reaching the target calorie is controversial. It is believed that endogenous energy is produced in the acute stage, and nutrition support may lead to harmful overfeeding to patients20. An observational study found that meeting 70–80% of the target calorie within 1 week might be ideal21. Notably, the EN formulation used in this study was mostly 1 or 0.9 kcal/ml. Meeting the target energy intake requires about 1300 ml of EN, which increases the difficulty of fluid management in critically ill patients and might be unfavorable for the removal of organ support such as mechanical ventilation or renal replacement therapy. Meanwhile, on day 7, EN intake < 20 kcal/kg/day (intolerance) was happened in 70% patients, with the negative impact on 28-day survive (Kaplan–Meier survival analysis). This result is concordance with other reports10, 11, 15, 16, which reference the benefit to reaching EN tolerance within 7 days.
It is widely accepted that the protein intake in critically ill patients should be > 1 g/kg/day and at least 0.8 g/kg/day for general hospitalized patients22, 23. In this study, only about 50% of patients reached an intake of > 0.5 g/kg/day. In the NEED study by Ke et al.24, the average protein intake was 0.67 g/kg/day. In this study, logistic regression and the Kaplan–Meier survival analysis indicated that a protein intake < 0.5 g/kg/day on day 3 or 7 significantly affected 28-day mortality. These results are supported by other observational studies25, 26, emphasizing the importance of protein intake in the early stage of critical illness. Obviously, improving EN tolerance is helpful to reach the protein target.
Risk factors of EN intolerance
An international nutrition survey showed that the average calorie intake in critically ill patients on day 7 was at 16.5 kcal/kg/day27. The 2017 Nutrition Day survey also showed that less than 25% of the patients reached a target volume of 25 kcal/kg/day within 2 weeks in the ICU28. According to the definition of EN intolerance, it is sure that most patients could be diagnosed with EN intolerance.
FI can also be diagnosed based on symptoms such as abdominal distension, nausea and vomiting, and gastric residual volume (GRV). Taking routine GRV measures is against the mainstream guidelines, while other symptoms lack an objective way of quantification15, 16. Using the actual feeding amount as the criterion for EN intolerance is more relative to the EN intolerance definition, and the method is objective and easy to standardize. Therefore, we defined EN intolerance according to whether the EN could reach 20 kcal/kg/day.
In this study, the main factors predicting EN tolerance on day 7 were AGI grade on day 1 and any organ support on day 3. A study showed that the AGI grade on day 1 was associated with future GI function and ICU outcomes29. The intestinal function of critically ill patients can often be improved after appropriate treatment and organ support (mechanical ventilation, renal replacement therapy, vasopressor, etc.). Thus, organ support means a higher probability of controlling the critical state, so there might be a higher possibility that the GI function could be preserved.
The predictors of EN tolerance are less studied because of the significant differences in the definition of EN tolerance, especially when tolerance is judged according to the symptoms4. Hu et al.4 reported that 15 factors, including pneumonia, nutritional preparation, shock, skin infection, continuous feeding, etc., were associated with tolerance and established a predictive model. Unfortunately, the number of patients was small, and the results need to be confirmed4.
In this study, 15.01% (n = 94) of patients received post-pyloric feeding in the ICU, which is a low level. Post-pyloric feeding can improve EN tolerance and thus improve nutritional intake24, but the regression analysis in this study showed that the use of post-pyloric feeding did not affect whether the patient’s calorie intake reached 20 kcal/kg/day.
Limitations
This study has limitations. First, as an observational study, the causal relationship between EN treatment and the patient outcome cannot be established. Secondly, the number of hospitals involved in this study was less than half of the number of tertiary hospitals in SHANGHAI and did not cover the secondary hospitals, thus biasing the results. In addition, although this study included consecutive patients admitted over 1 month in 15 ICUs, the sample size was relatively small. Third, the study time in each center was about 1 month, and no further long-term prognosis of the patients was followed up. The impact of nutritional therapy on patients might be difficult to reflect on in the short term, and follow-up for long-term outcomes is necessary.
The institutions that participated in the study covered half of the city districts (8/16 districts in SHANGHAI) and were mainly tertiary hospitals that admitted patients from all over SHANGHAI. Thus, we believe the patients’ data are representative of the SHANGHAI ICU patients.
Conclusions
The proportion of EN intolerance in ICU patients is high. Patients with better EN tolerance have a better 28-day survival rate. A protein intake on day 7 of < 0.5 g/kg/day is an important factor affecting patient survival at 28-day survival. Improving EN tolerance and protein intake in early ICU days may improve the outcomes of the patients.
Data availability
All data generated or analysed during this study are included in this published article.
References
Preiser, J. C. et al. A guide to enteral nutrition in intensive care units: 10 expert tips for the daily practice. Crit. Care 25, 424 (2021).
Heyland, D. K. et al. Incidence, risk factors, and clinical consequence of enteral feeding intolerance in the mechanically ventilated critically Ill: An analysis of a multicenter. Multiyear Database Crit. Care Med. 49, 49–59 (2021).
Shankar, B., Daphnee, D. K., Ramakrishnan, N. & Venkataraman, R. Feasibility, safety, and outcome of very early enteral nutrition in critically ill patients: Results of an observational study. J. Crit. Care 30, 473–475 (2015).
Arabi, Y. M. Predicting enteral feeding intolerance in patients with sepsis: Why and how?. Saudi J. Gastroenterol. 28, 1–2 (2022).
Reintam Blaser, A. et al. Gastrointestinal function in intensive care patients: terminology, definitions and management. Recommendations of the ESICM Working Group on Abdominal Problems. Intensive Care Med. 38, 384–394 (2012).
Chinese Abdominal Intensive Care Association. Asia society for emergency and critical care medicine. Expert consensus on enteral nutrition for gastrointestinal dysfunction in critically ill patients. Chin. J. Dig. Surg. 20, 1123–1136 (2021).
Heyland, D. K., Dhaliwal, R., Jiang, X. & Day, A. G. Identifying critically ill patients who benefit the most from nutrition therapy: The development and initial validation of a novel risk assessment tool. Crit Care. 15, R268 (2011).
Jie, B. et al. Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition 28, 1022–1027 (2012).
Xing, J. et al. Enteral nutrition feeding in Chinese intensive care units: A cross-sectional study involving 116 hospitals. Crit. Care 22, 229 (2018).
Li, Z. et al. Association between hospital and ICU structural factors and patient outcomes in China: A secondary analysis of the national clinical improvement system Data in 2019. Crit. Care. 26, 24 (2022).
Reignier, J. et al. Enteral versus parenteral early nutrition in ventilated adults with shock: A randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2). Lancet 391, 133–143 (2018).
De Waele, E., Jonckheer, J. & Wischmeyer, P. E. Indirect calorimetry in critical illness: A new standard of care?. Curr. Opin. Crit. Care. 27, 334–343 (2021).
Singer, P. et al. The tight calorie control study (TICACOS): A prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med. 37, 601–609 (2011).
Duan, J. Y., Zheng, W. H., Zhou, H., Xu, Y. & Huang, H. B. Energy delivery guided by indirect calorimetry in critically ill patients: A systematic review and meta-analysis. Crit. Care. 25, 88 (2021).
McClave, S. A. et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: Society of critical care medicine (SCCM) and American society for parenteral and enteral nutrition (A.S.P.E.N.). JPEN J. Parenter. Enteral. Nutr. 40, 159–211 (2016).
Singer, P. et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 38, 48–79 (2019).
Ichimaru, S., Fujiwara, H., Amagai, T. & Atsumi, T. Low energy intake during the first week in an emergency intensive care unit is associated with reduced duration of mechanical ventilation in critically ill, underweight patients: A single-center retrospective chart review. Nutr. Clin. Pract. 29, 368–379 (2014).
Rice, T. W. et al. Initial trophic vs full enteral feeding in patients with acute lung injury: The EDEN randomized trial. Jama 307, 795–803 (2012).
Arabi, Y. M. et al. Permissive underfeeding or standard enteral feeding in critically Ill adults. N. Engl. J. Med. 372, 2398–2408 (2015).
Oshima, T. et al. Indirect calorimetry in nutritional therapy. A position paper by the ICALIC study group. Clin. Nutr. 36, 651–662 (2017).
Zusman, O. et al. Resting energy expenditure, calorie and protein consumption in critically ill patients: A retrospective cohort study. Crit. Care. 20, 367 (2016).
Thibault, R. et al. ESPEN guideline on hospital nutrition. Clin. Nutr. 40, 5684–5709 (2021).
Ochoa Gautier, J. B. et al. How much and what type of protein should a critically Ill patient receive?. Nutr. Clin. Pract. 32, 6s–14s (2017).
Ke, L. et al. Actively implementing an evidence-based feeding guideline for critically ill patients (NEED): A multicenter, cluster-randomized, controlled trial. Crit. Care. 26, 46 (2022).
Nicolo, M., Heyland, D. K., Chittams, J., Sammarco, T. & Compher, C. Clinical outcomes related to protein delivery in a critically Ill population: A multicenter, multinational observation study. JPEN J. Parenter. Enteral. Nutr. 40, 45–51 (2016).
Allingstrup, M. J. et al. Provision of protein and energy in relation to measured requirements in intensive care patients. Clin. Nutr. 31, 462–468 (2012).
Bendavid, I. et al. NutritionDay ICU: A 7 year worldwide prevalence study of nutrition practice in intensive care. Clin. Nutr. 36, 1122–1129 (2017).
Ridley, E. J. et al. Nutrition therapy in Australia and new Zealand intensive care units: An international comparison study. JPEN J. Parenter. Enteral. Nutr. 42, 1349–1357 (2018).
Zhong, M. et al. Association of changes in acute gastrointestinal injury grade with prognosis in critically Ill patients: A prospective, single-center,Observational Study. J. Multidiscip. Healthc. 14, 279–286 (2021).
Acknowledgements
Great gratitude should be given to Wen Xu and Wenjie Chen for their great help in manuscript preparation. Many thanks are to be sent for the helpful contributions of all the ICU staff, as well as for the understanding and love of all the family members.
Funding
The study was supported by the Program for Outstanding Medical Academic Leaders and Clinical innovation Program in science and technology by Shengkang hospital development center (SHD22021304).
Author information
Authors and Affiliations
Contributions
M.Z., Y.Z.Q., H.P.Q. and E.Z.C. equally contributed to the conception and design of the research; Y.G., J.G.T., J.Y.Z., G.F., S.W. and X.Y.L. contributed to the design of the research; T.T.P., R.L.W., Y.G., X.B.W. and Z.X.W. contributed to the acquisition and analysis of the data; T.T.P., R.L.W., X.B.W., Y.C.L., Z.F.L., Z.X.W., J.G.T., X.L., X.M.W., Y.G., G.F. and J.Y.Z. contributed to the interpretation of the data; and M.Z., Y.Z.Q. and T.T.P. drafted the article. All authors critically revised the article, agree to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhong, M., Qiu, Y., Pan, T. et al. Improving enteral nutrition tolerance and protein intake maybe beneficial to intensive care unit patients. Sci Rep 13, 21614 (2023). https://doi.org/10.1038/s41598-023-49050-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-49050-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.